Introduction
The lumbosacral spine consists of five large vertebrae that make up the lumbar spine and five fused vertebrae that make up one single bone which articulate on each side of pelvis called the sacrum. Overall, spinal balance is determined by a mixture of kyphosis and lordosis throughout the spine. Lumbar lordosis is an important factor in overall sagittal balance, which contributes to bipedalism posture and upright gait. Approximately 40–60 degrees of lordosis is present in the lumbar spine. Although there is inherent variability between patients, there is an increase in lumbar lordosis from the upper to lower segments with approximately two-thirds of lumbar lordosis occurring at the L4-S1 levels. The balance, alignment, and motion of the spine are determined by lumbopelvic alignment and pelvic compensation for sagittal alignment in the thoracic and lumbar spine.
Ultimately lumbopelvic parameters have an important impact on the pathogenesis of lumbar degenerative conditions and spinal deformity. The relationship between the lumbosacral spine and the pelvic morphology stresses the importance of plain radiographs in overall spinal alignment. The present chapter discusses the importance of plain radiographs in determining the relationship between the lumbosacral spine and the pelvis with an emphasis on clinical relevance and techniques when performing these measurements.
Specific Radiographic Parameters
During examination of the lumbosacral spine, indications for full-length or isolated posteroanterior and lateral radiographs may differ upon the presenting complaints. Standing full-length 36-inch posteroanterior and lateral radiographs are the baseline imaging studies to evaluate sagittal balance, which has been described in depth in a previous chapter. The hips and knees should be extended during standing radiographs to negate any compensatory mechanisms. The use of posteroanterior projection decreases patient radiation exposure by 41% in comparison with the use of anteroposterior projection. If a practitioner chooses to obtain isolated standing lumbosacral radiographs, the femoral heads should be included to adequately assess the relationship between lumbosacral and pelvic parameters. All measurements are made using lateral radiographs unless otherwise specified.
General Lumbar Spine
Coronal balance
When evaluating overall spinal balance, coronal alignment should be assessed with full-length 36-inch standing posteroanterior radiographs with the hips and knees extended. The presence of deformity, pelvic obliquity, and leg length discrepancy can be noted on posteroanterior radiographs. If a leg length discrepancy greater than 2 cm is already known, then a leg lift can be placed under the shorter leg during radiographic evaluation.
Coronal regional alignment
Coronal lumbar and lumbosacral curves are defined as having an apex from L1 to L5 and L5 to S1, respectively, as measured by the Cobb method from the end vertabrae. The cephalad end vertebra is the first vertebra in the cephalad direction whose superior endplate is tilted maximally toward the concavity of the curve. The caudad end vertebra is the first vertebra in the caudad direction whose inferior endplate is tilted maximally toward the concavity of the curve. Apical vertebral translation (AVT) is defined as the horizontal distance measured from the C7 plumb line to the center of the central sacral vertical line (CSVL) for lumbar and lumbosacral curves. The central sacral vertical line is defined as a vertical line drawn through the center of the S1 endplate. Coronal spinal balance is defined from the center of C7 and the midpoint of the thoracic trunk to the sacrum. Coronal imbalance of greater than 4 cm has been correlated with deterioration in pain and function scores in unoperated patients but not in patients with surgery. This suggests that sagittal correction may be more important than coronal correction and will be discussed later in this chapter.
Coronal pelvic alignment
Coronal pelvic alignment can be defined by leg length discrepancy and pelvic obliquity. Pelvic obliquity is measured by the angle created by a horizontal line and a line tangential to the top of the sacral ala. Pelvic obliquity can be seen as a compensatory mechanism from lumbar or lumbosacral deformity, leg length deformity, or both. Leg length discrepancy is defined as the vertical distance measured between horizontal lines drawn tangential to the top of each femoral head. It is important to note the etiology of the pelvic obliquity as compensatory lumbar or lumbosacral curves can be mistaken for true deformity in the setting of an undiagnosed leg length discrepancy greater than 2 cm.
Spinopelvic Parameters
Overall sagittal balance and the relationship between the lumbosacral spine and the pelvis are evaluated from the lateral radiograph. Key components of spinopelvic parameters include lumbar lordosis (LL), pelvic incidence (PI), pelvic tilt (PT), and sacral slope (SS). The influence of the cervical spine on the overall sagittal balance is worth mentioning here and is measured by the C7–S1 sagittal vertical axis (SVA) ( Fig. 1 ).
- •
C7–S1 sagittal vertical axis
- •
Draw a vertical plumb line centered at the midline of the C7 vertebral body to the posterior-superior corner of the S1 endplate
- •
Measure the horizontal distance from the vertical plumb line
- •
SVA has a (+) value when anterior to the sacral reference point and a (−) value when posterior to the sacral reference point.
- •
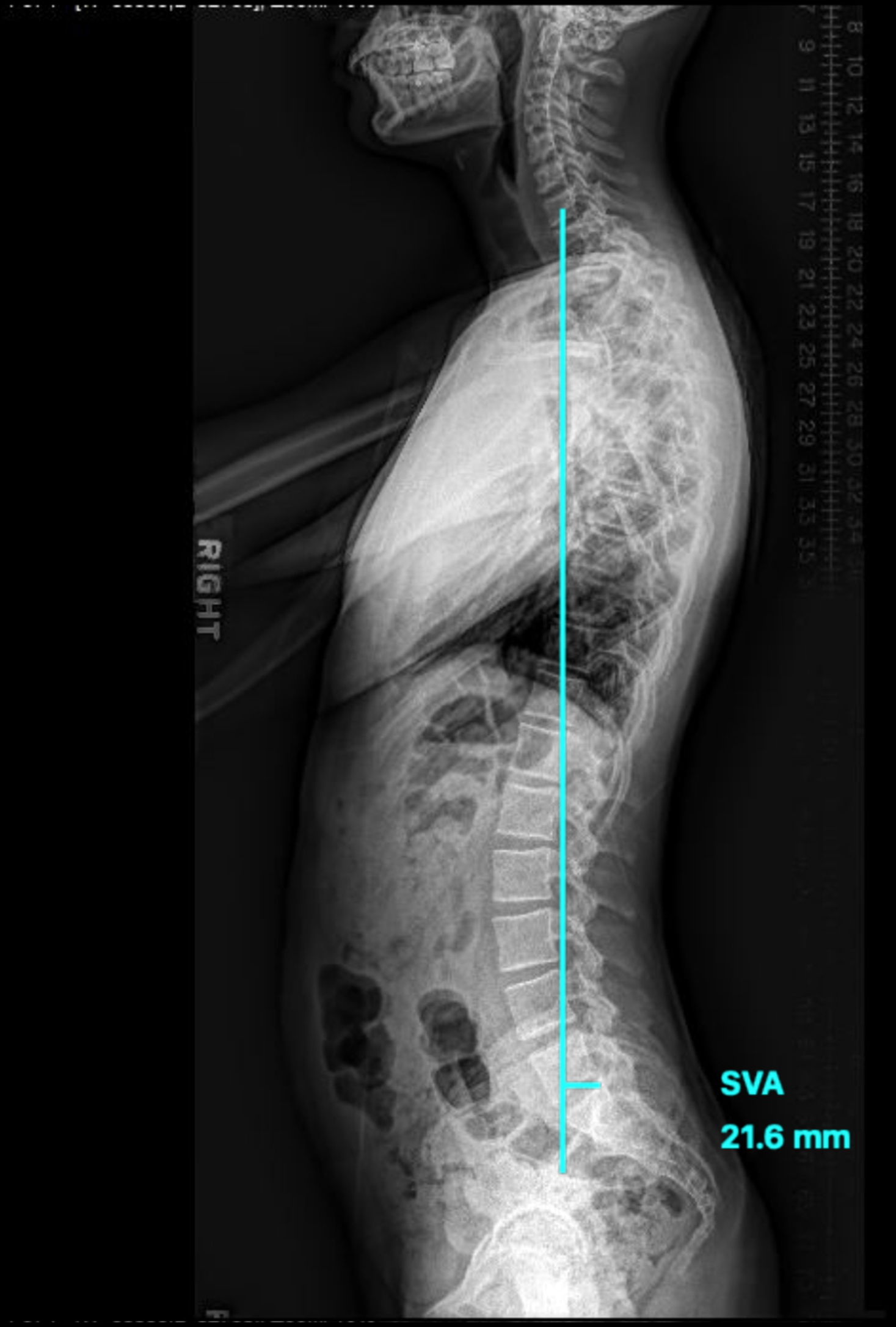
There is an association between the loss of lordosis and an anterior shift of the SVA. Spinopelvic harmony exists when the SVA < 50 mm. Restoration of the SVA achieves level gaze and has been found to lead to better Health Related Quality of Life (HRQoL) scores.
Lumbar lordosis
There is a relationship between thoracic kyphosis and lumbar lordosis as well as a relationship between lumbar lordosis and pelvic incidence. Different patterns of lordosis have been reported, each defined by the patient’s pelvic incidence. Defining lumbar lordosis is important when evaluating sagittal balance ( Fig. 2 ).
- •
Cobb angle
- •
Draw a line along the superior endplate of L1
- •
Draw a perpendicular line intersecting the first line
- •
Draw a line along the superior endplate of S1
- •
Draw a perpendicular line intersecting the second line
- •
The angle formed by the intersection of the two perpendicular lines is the Cobb angle measurement for lumbar lordosis.
- •
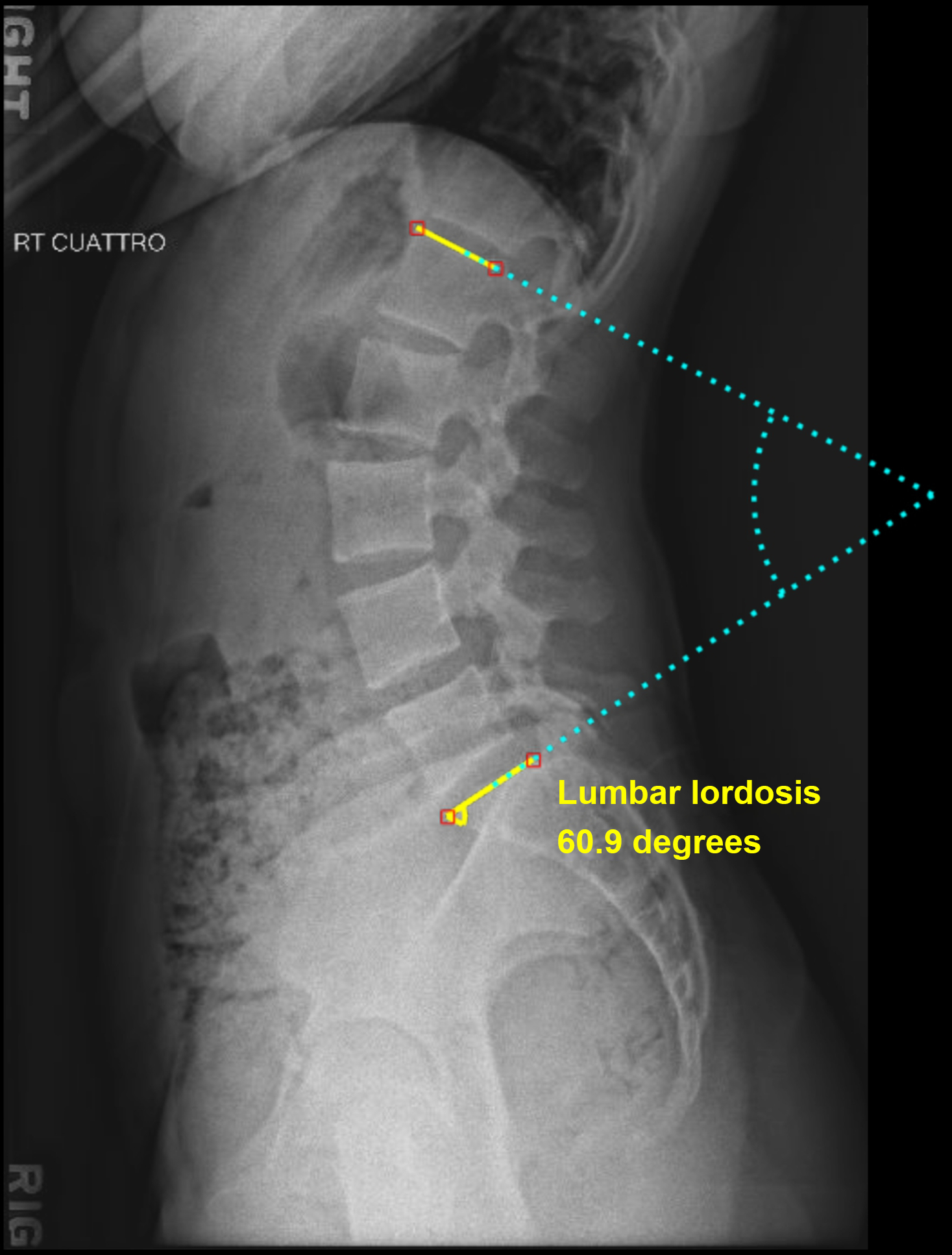
In spinopelvic harmony, the LL will match PI within 11 degrees. Normal values of lumbar lordosis can be seen within 60 degrees ± 12 degrees. The majority of lumbar lordosis resides within L4-S1. Degenerative changes within the spine such as loss of disc height can lead to a decrease in lordosis as patients age. Trauma such as compression fractures can also lead to a loss of lumbar lordosis. Iatrogenic flatback deformity from spinal fusions can create a hypolordotic spine and lead to the overall sagittal imbalance. Understanding the etiology of a patient’s lordosis in the lumbar spine is important as lumbar lordosis is the most readily changed spinopelvic parameter with surgery.
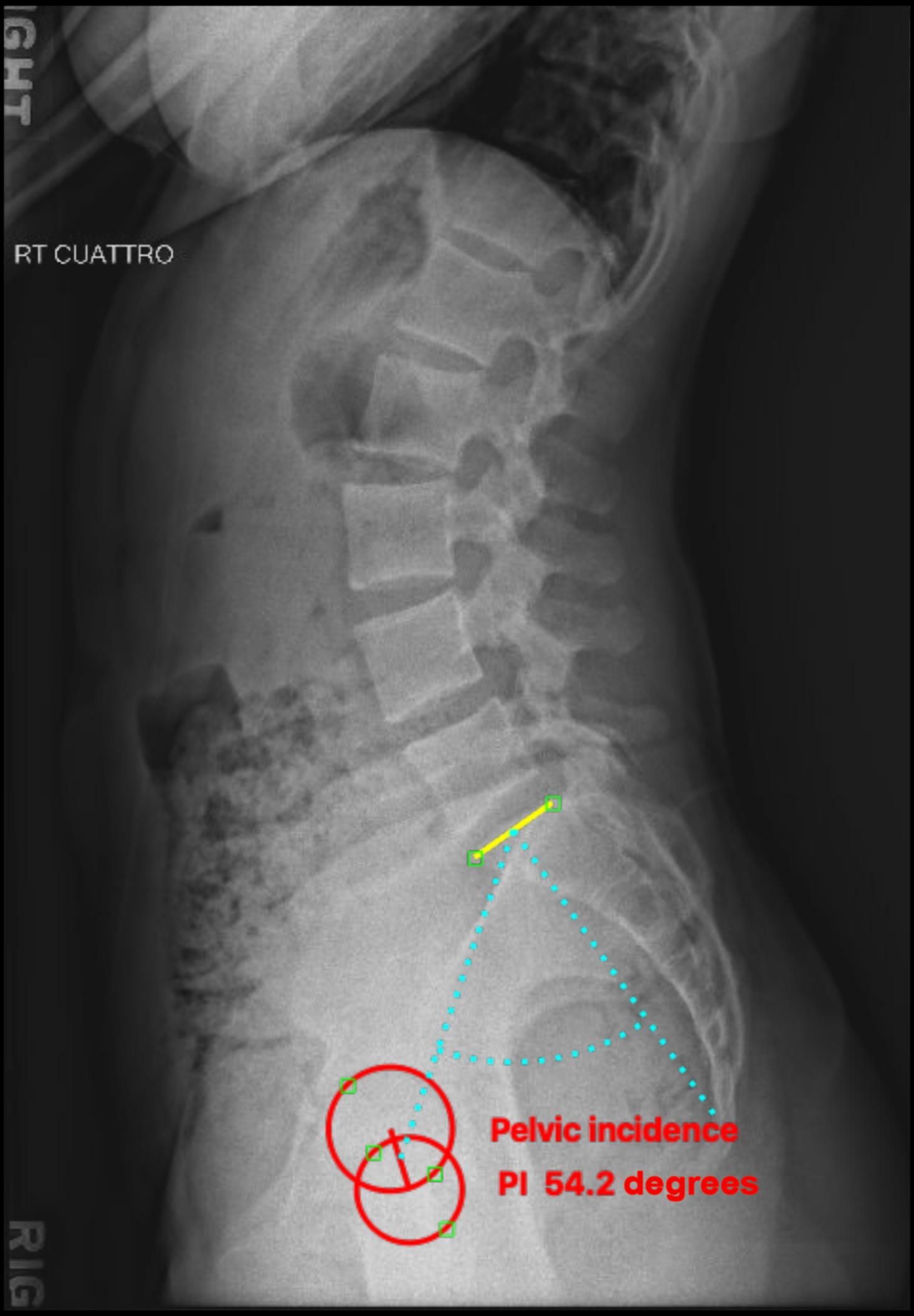
Pelvic incidence
Pelvic incidence is an anatomic value that is constant and unique to each patient, and does not change with spatial orientation of the pelvis ( Fig. 3 ). As stated previously, PI can influence LL as well as thoracic and cervical sagittal contours.
- •
Pelvic incidence
- •
Draw a line from the center of the femoral head to the midpoint of the sacral endplate
- •
If the femoral heads are not overlapping, then choose a point equidistance between the femoral heads.
- •
- •
Draw a line orthogonal to the sacral endplate
- •
The angle formed between the two lines is defined as pelvic incidence and is also the sum of the sacral slope and pelvic tilt. (PI = SS + PT) ( Fig. 4 ).
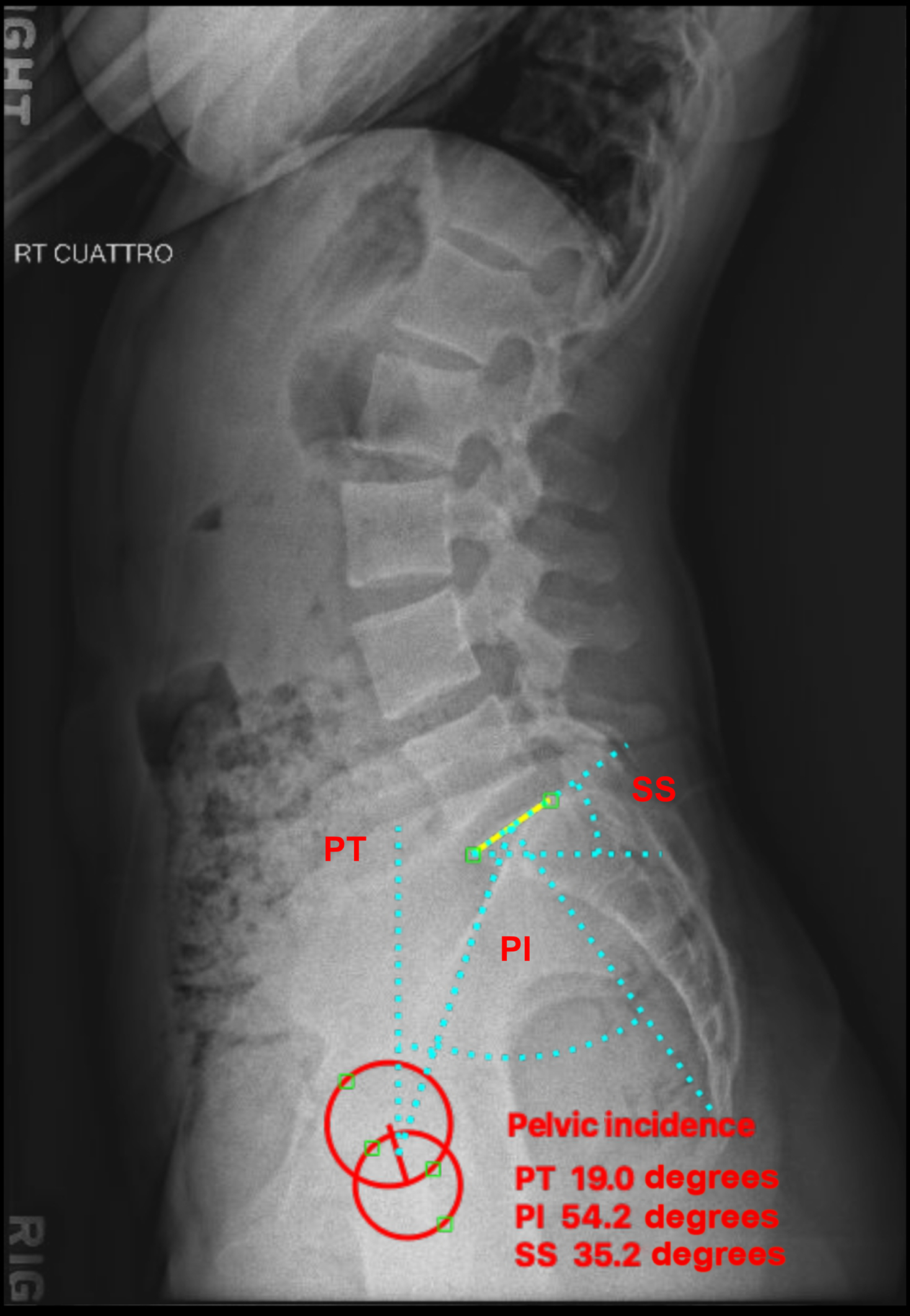
Fig. 4
Sagittal pelvic parameters.
- •
Pelvic incidence is a fixed value for patients; therefore, we must evaluate its relationship with lumbar lordosis. The impact of the relationship between PI and LL has been studied extensively, and a value of greater than 11° (PI-LL) was associated with disability in terms of the Oswestry Disability Index (ODI) scores. Pelvic incidence can be increased in patients with high-grade spondylolisthesis. While the value itself cannot be changed, it is important to note PI when evaluating the amount of correction needed in the lumbar spine during sagittal correction.
Pelvic tilt
Now that we have assessed the relationship between lumbar lordosis and pelvic incidence, we can evaluate the patient’s compensatory mechanism for PI-LL mismatch and positive SVA by the use of pelvic tilt. Pelvic tilt is a variable spinopelvic parameter and is used to compensate for the loss of lumbar lordosis by extending through the pelvis to maintain a normal sagittal balance ( Fig. 4 ).
- •
Pelvic tilt
- •
Draw a vertical line through the center of the femoral heads
- •
Draw a line from the center of the femoral heads to the midpoint of the sacral endplate
- •
The angle between the two lines is defined as pelvic tilt
- •
Normal value < 25 degrees.
- •
Increasing PT or pelvic retroversion reflects the patient’s need to compensate for sagittal imbalance. Significant correlation has been noted between SVA and PT. In addition, pain and disability scores are increased in patients that are found to have PT > 25 degrees and a high SVA > 50 mm. The ability of a patient to compensate for sagittal imbalance via PT can vary and can be limited in patients with joint stiffness and muscle tightness. As a patient exhibits positive SVA, he or she will compensate by retroverting the pelvis and flexing the knees to maintain horizontal gaze and center the head over the pelvis. This method of compensation requires increased energy expenditure and has been noted with decreased HRQoL scores.
Pelvic tilt is not changed by surgical intervention but should be assessed during the evaluation of the lumbosacral spine in order to identify a patient that is compensating for sagittal imbalance. Patients with flatback deformity who have increased posterior pelvic tilt have been found to have little change in posterior pelvic tilt from a standing to sitting position. This lack of change in posterior tilt can lead to femoroacetabular impingement in patients undergoing total hip arthroplasty.
Sacral slope
While PI, PT, and LL receive much attention in regard to spinopelvic parameters, there is a high correlation between lumbar lordosis and sacral slope. Sacral slope is not a fixed angle and depends on the position of the pelvis relative to the hip axis. Pelvic incidence is the sum of sacral slope and pelvic tilt creating an inverse relationship between PT and SS ( Fig. 4 ).
- •
Sacral slope
- •
Draw a line along the sacral endplate
- •
Draw a line from the posterosuperior endplate to the horizontal
- •
The angle formed between the two lines is defined as sacral slope.
- •
Patients with a lower lumbar lordosis and a more horizontal sacrum are more likely to develop lumbar degenerative pathology, including disc herniation. Patients with a higher SS and correlating PI and a lumbar lordosis apex of L3 or above are more likely to develop spinal stenosis. Patients with a high pelvic incidence and sacral slope shift their center of axis anteriorly creating higher shear forces in the lumbosacral spine. This can lead to pathologies such as developmental spondylolisthesis. While there is no normal value for sacral slope, it is important to take into account its value in the overall sagittal balance. Patients who are fused in a positive sagittal balance with a high sacral slope are more likely to develop adjacent segment degeneration. Correcting a PI-LL mismatch will establish a normal pelvic tilt and normalization of the SS.
Degenerative Lumbar Spine
When evaluating the degenerative lumbosacral spine, it is important to obtain standing posteroanterior and lateral radiographs. If there is concern for spondylolisthesis, standing flexion and extension lumbar radiographs should be obtained as well. The femoral heads should always be included in case a provider wishes to evaluate spinopelvic parameters in the degenerative lumbar patient. All radiographs should be evaluated for signs of osteophytes, foraminal narrowing, endplate sclerosis, disc space narrowing, and vacuum phenomenon within the disc.
Spondylosis
Lumbar spondylosis is broadly defined as the degenerative destruction or remodeling of the spine, intervertebral discs, and facet joints. Facet arthrosis, decreased disc height, foraminal narrowing, and subchondral sclerosis are radiographic signs of degeneration. As the intervertebral disc degenerates, decreased disc height occurs. Decreased disc height alters the biomechanics of the facet joints which can lead to arthrosis, which is often a cause of radiculopathy. Facet arthrosis is best seen on MRI or CT but can also be visualized on standard oblique radiographs. Foraminal stenosis can also be caused by facet hypertrophy, which is indicative of facet arthrosis.
Contour lines
There is no literature regarding the use of contour lines in the lumbar spine radiography, but it is important to note the alignment of the anterior and posterior bodies in the lumbosacral spine. It is also important to note the spinolaminar line as well as the spinous process line. We will discuss pathologies related to contour lines later in this chapter.
Disc height/foraminal height
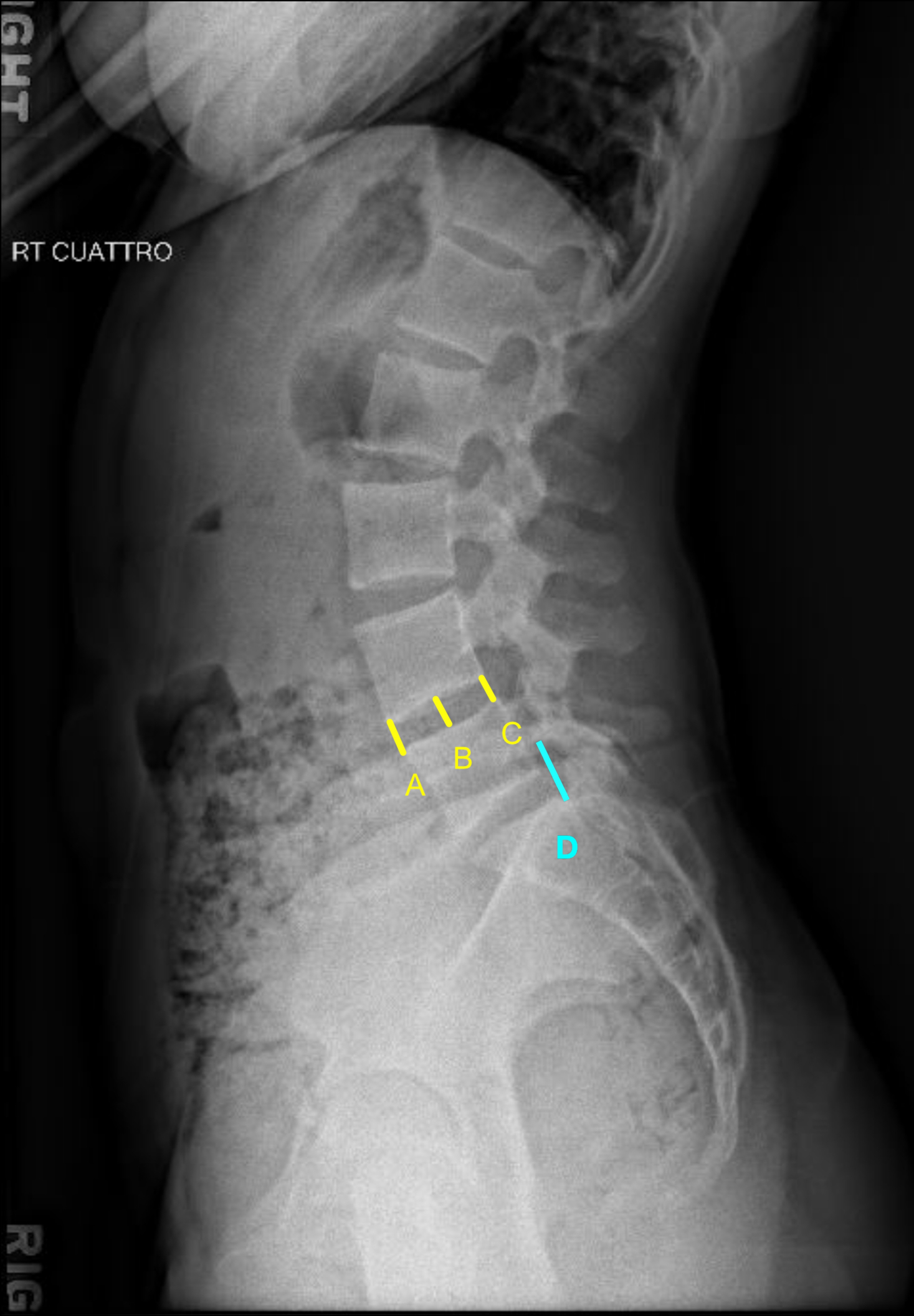
Disc height (DH) is an important parameter to evaluate the degenerative lumbar spine for both diagnostic purposes and surgical planning. Restoration of DH is a mainstay in lumbosacral spine surgery. Disc height and foraminal height are directly related to each other. The use of interbody cages allows for a change in disc height, which in turn affects foraminal height. Chapter 6 outlines a detailed explanation of DH measurement in the cervical spine that can be applicable to the lumbar spine. For our purposes in the lumbar spine, we will discuss a general measurement of DH and foraminal height used in diagnostic evaluations and surgical planning ( Fig. 5 ).
- •
Disc height
- •
Measure the distance from the superior endplate of the caudal vertebra to the interior endplate of the rostral vertebra at the most anterior aspect of the disc space
- •
Measure the distance as stated earlier at the midline of the disc space
- •
Measure the distance as stated earlier at the most posterior aspect of the disc space
- •
The average of these three measurements is defined as the disc height.
- •
- •
Foraminal height
- •
Measure the distance between the inferior pedicle wall and the superior pedicle wall of the inferior level.
- •