Clinical Correlation
Patients who present with undifferentiated shortness of breath can be challenging due to the broad differential diagnosis, which encompasses pulmonary, cardiac, mixed cardiopulmonary, and noncardiopulmonary etiologies. Lung ultrasound has revolutionized the approach to the undifferentiated dyspneic patient. What makes lung ultrasound somewhat unique is that whereas other ultrasound applications use traditional grayscale images of the patient’s anatomy to answer focused questions, lung ultrasound looks at changes in expected artifacts, as the pleural interfaces and air-to-water ratio change in the lung during different pathologic processes.
Normal Anatomy
The ultrasound image should include at least two hyperechoic ribs with acoustic shadowing beneath them. The intercostal muscles have a mixed echogenicity, and deep to this is the hyperechoic line that represents the parietal and visceral pleural interface. As the patient breathes, the visceral and parietal pleural move up on one another in opposite directions. The ultrasound representation of this is a “sliding,” or movement, artifact at the hyperechoic pleural line. Deep to the pleural interface there are horizontal hyperechoic lines called A-lines that are a reverberation artifact between the transducer and the parietal pleural interface and are displayed at equidistant depth intervals in the lung ( Fig. 8.1 ). In addition to A-lines, there is an occasional hyperechoic vertical line that starts at the pleural interface, moves dynamically with lung sliding, and then quickly diminishes or fades. These are referred to as comet tail artifact (a type of reverberation artifact). Like lung sliding, comet tail artifacts are an indication that the parietal and visceral pleura are in contact with each other. Lung pulse is a rhythmic shimmering that occurs at the pleural interface due to normal cardiac oscillation when the patient is either breath-holding or poorly ventilating a lung (e.g., mainstem intubation). The M-mode is used to evaluate the lung. M-mode is a focused sector of sound with a display of the reflected images along a time axis. Normal lung where the visceral and parietal pleura are in contact with one another creates a granular artifact at the pleural interface on M-mode that has been described as a sandy beach , with the other structures above the pleural interface appearing as a beach and sky , making the whole image a seashore sign ( Fig. 8.2 ).


Imaging
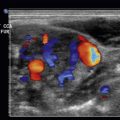
Imaging of the lung parenchyma is performed with a low-frequency phased array transducer (microconvex or curvilinear transducers can also be used) with a preset depth range of 12 to 16 cm. In trauma patients who present supine and evaluation for pneumothorax is the primary indication for lung ultrasound, some providers prefer to use a high-frequency linear transducer at 4 to 8 cm depth (depending on the patient’s body habitus) for increased resolution of the pleural interface. Each hemithorax is divided into four lung zones ( Fig. 8.3 ). A complete lung exam involves looking at each of the four zones on both hemithoraces with the patient typically reclined at 30 to 45 degrees.

To start the exam, place the transducer in the second to third intercostal space in the midclavicular line. This is lung zone 1. Direct the probe indicator cephalad. In trauma patients with concern for pneumothorax, place the transducer on the most anterior portion of the chest wall, as this is the most likely spot for air to accumulate.
Pathology
Pneumothorax
A pneumothorax occurs when the visceral surface of the lung separates from the parietal pleura and air occupies the space in between the two interfaces. This lack of contact between the pleural surfaces leads to the absence of lung “sliding.” The absence of expected artifact is a chief indicator of the presence of the pneumothorax. Other criteria that help make the diagnosis of pneumothorax are the absence of comet tail artifact and the absence of lung pulse.
The use of M-mode has also been described in the diagnosis of pneumothorax. When a pneumothorax is present and the transducer is placed over a section of lung where there is no lung sliding, the sandy beach of the seashore sign will be absent and replaced by horizontal lines similar to the artifact above the pleural interface. This image of a pneumothorax using M-mode is called the bar code sign or stratosphere sign ( Fig. 8.4 ). In evaluating for a pneumothorax, one can achieve 100% specificity by identifying a “lung point.” A lung point is the precise site where the visceral and parietal pleura transition from being in contact with one another to having air between them. The dynamic ultrasound image of this will show an area of lung sliding that abruptly stops. One can liken this image to a curtain that slides across the lung window image but does not make it all the way across ( Fig. 8.5 ). This exact spot where the sliding stops is the edge of the pneumothorax. By following the lung point on the chest wall, one can estimate the size of the pneumothorax. Identifying a lung point rules in the diagnosis of a pneumothorax. Of note, some anatomic sites can mimic the presence of a lung point. These lung point mimics are termed false lung points and occur where the pleural interface ends and either diaphragm or pericardium begins. A false lung point image includes lung sliding that appears to stop; however, when examined closely, the hyperechoic parietal pleura ends and is replaced by the more hypoechoic presence of the pericardium or diaphragm ( Fig. 8.6 ). In a true lung point, the hyperechoic pleural line remains visible. False lung points are normal anatomic interactions that occur in expected places (left side of chest, lower chest wall).