LYMPHOMA
KEY POINTS
- Lymphoma is a common disease of the head and neck.
- Lymphoma most often presents as nodal disease.
- In its extranodal varieties, it takes on appearances that mimic other pathologies.
- Angiocentric and angiotropic lymphoma are forms that may commonly be mistaken for other pathology.
- Differentiation of lymphoma from reactive or proliferative but benign lymphoid processes is often difficult based on imaging findings.
INTRODUCTION
Prevalence and Etiology
Lymphoma is a relatively common malignancy of uncertain precise etiology. It has associations with disorders such as HIV and Epstein-Barr virus infection but no definitive causative relationship.1,2 The disease affects all age groups but is most common in young to middle-aged adults.3
In general, it is difficult to determine the frequency of lymphoma arising primarily in, or strictly limited to, the head and neck region. Often, head and neck lymphoma is part of systemic involvement. However, the head and neck region may be the site of presenting complaints in secondary as well as primary disease. The best known presentation is probably cervical adenopathy; however, lymphoma can mimic most infiltrating highly cellular malignancies at any particular site. It is probably best to also consider the chronic leukemias in this context from a morphologic and spread pattern perspective since their nodal presentation cannot be distinguished from lymphoma, but these are not lymphomas and not part of the classification. The nodal expression of this disease is considered in more detail in conjunction with reactive and lymphomatous lymphadenopathy in Chapter 158.
The patterns of disease spread described in the following material will apply across lymphoma that involves in all anatomic regions of the head and neck.
PATTERNS OF DISEASE AND PATHOLOGY
The debate of how to classify lymphomas is well beyond the scope of this text. For a simple and reasonable approach, the fundamental separation of types used by the Lukes-Collins Revised Classification and Revised European-American Lymphoma (REAL) Classification is used here. The non-Hodgkin types are separated into T-cell and B-cell groups. Hodgkin disease is then the third major group.
Almost all of these diseases express themselves in the head and neck region often just as nodal disease. Some, like the chronic leukemias and Hodgkin disease, present almost entirely as nodal disease. Many also involve extranodal sites. It is the extranodal disease that is often most challenging to diagnosis correctly since the variable sites, morphology, and propensity for perineural and perivascular spread of some types of lymphoma make its presentation at extranodal sites protean.4 For this reason, lymphoma should enter the differential diagnosis of an infiltrating process in the head and neck when the disease morphology appears “unusual” for want of a better term or the pattern is multifocal and possibly perineural and perivascular (Figs. 27.1 and 27.2).
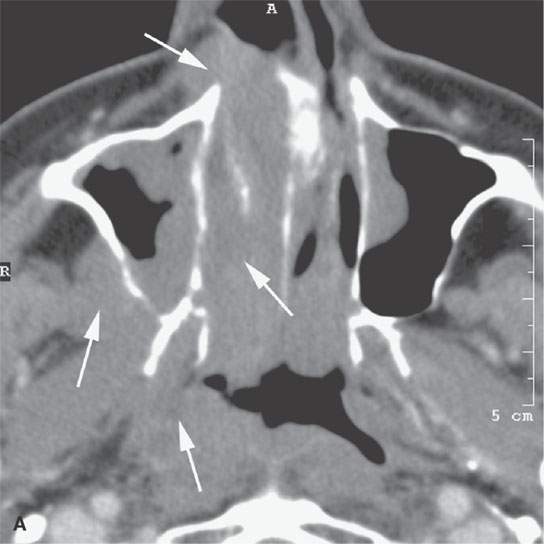
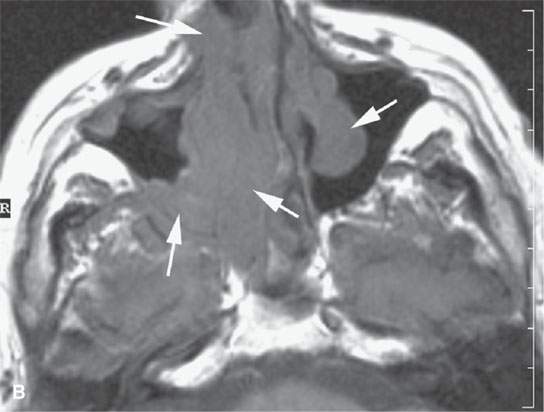
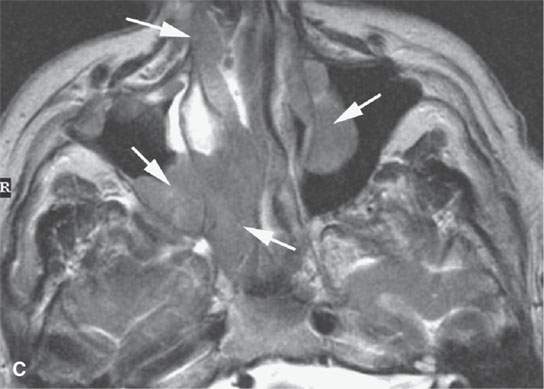

FIGURE 27.1. Contrast-enhanced computed tomography (CECT) and magnetic resonance imaging in a patient presenting with nasal stuffiness. Both studies show a multifocal, bilateral minimally enhancing mass not only of the sinuses and nasal cavity but also of the infratemporal fossa and nasopharynx (arrows). A: CECT. B: Non–contrast-enhanced T1-weighted (T1W) image. C: T2-weighted image. D: Contrast-enhanced T1W image.
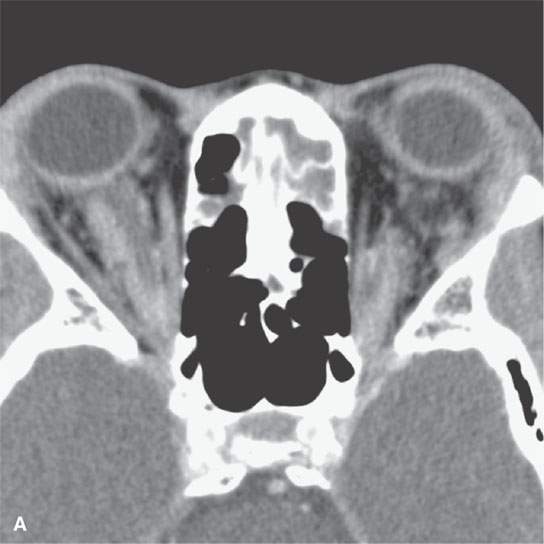
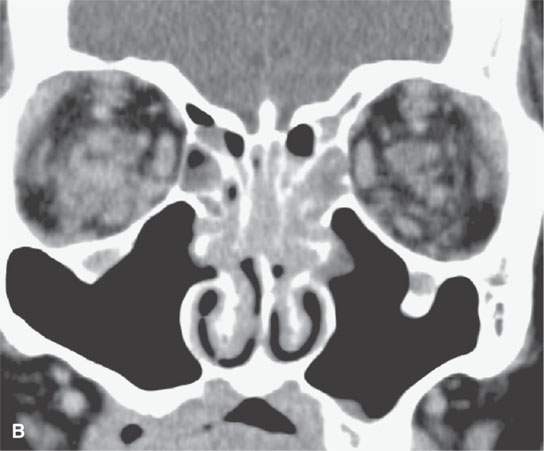
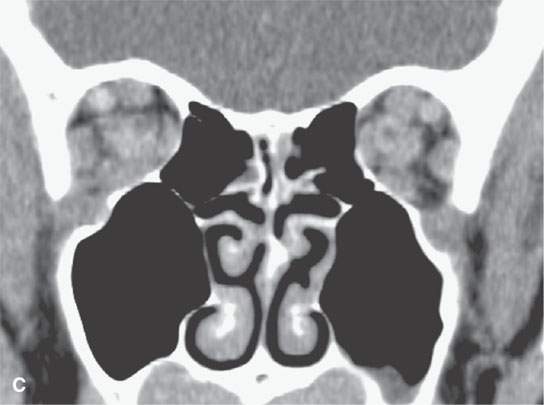
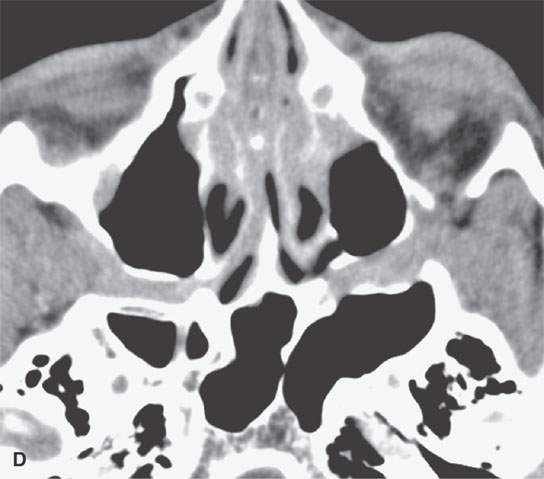
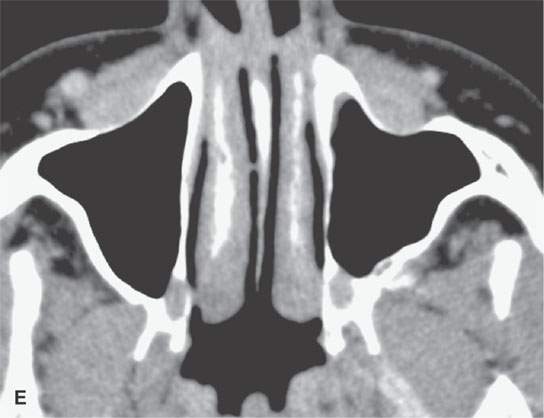
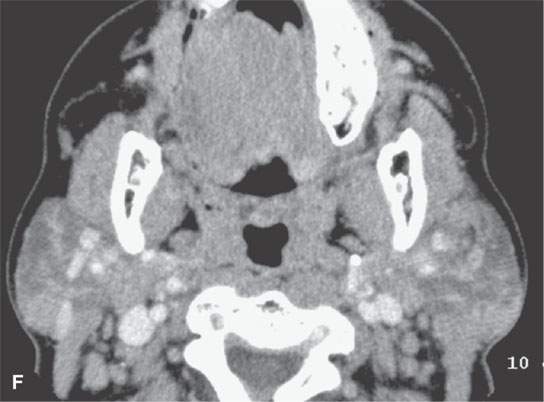
FIGURE 27.2. Contrast-enhanced computed tomography showing a minimally enhancing multifocal, bilateral infiltrating process in the orbits (A–C), nasal cavity (B), showing avidity for perineural spread along the infraorbital nerve canals (B, C), in the pterygopalatine fossa (D), and beneath the superficial musculoaponeurotic system (E). The parotid glands are involved bilaterally as well (F).
Immunocytochemical phenotyping and molecular genetics have altered the management of lymphoma and related necrotizing sinonasal diseases discussed in Chapter 92 as well as their differentiation from diseases such as Wegener granulomatosis or sarcoidosis. Terms like polymorphic reticulosis and lymphomatoid granulomatosis are also no longer used. The majority of these previously pathologically poorly understood entities are now known to be sinonasal lymphomas of B-cell lymphoma, T-cell lymphoma, and natural killer (NK)/T-cell lymphoma with a broad range of biologic activity depending on their immunophenotype. NK/T-cell lymphoma is strongly associated with the Epstein-Barr virus. The locoregional failure rates in these tumors are similar; however, distant failure is much more common in B-cell or NK/T-cell lymphoma than in T-cell lymphoma. T-cell lymphoma has the most favorable prognosis, and NK/T-cell has the worst.
Extranodal Disease Trends in B-Cell Lymphoma
In general, the extranodal sites of interest include the lacrimal glands (Fig. 27.3) and other contents of the orbits (Figs. 27.2 and 27.4), nasal cavity and sinuses (Fig. 27.5), the parotid glands (Figs. 27.6 and 27.7), the Waldeyer ring (Figs. 27.8 and 27.9), and thyroid gland (Fig. 27.10). Unusual sites of presentation include the canine fossa of the cheek, the buccal space, and the infratemporal fossa likely due to at least some relationship to the facial nodes and related lymphoid elements in these locations (Figs. 27.2 and 27.11), as discussed in Chapter 149. Disease in the larynx and trachea is rare (Figs. 27.12). As an example of potential uniqueness in an area where things tend to look the same, Burkitt lymphoma may be the most readily recognizable B-cell lymphoma due to its predilection for the facial bones and, particularly, the mandible (Fig. 27.13). Burkitt lymphoma also has both an extraordinary growth rate and an equally extraordinary tendency to respond quickly to chemotherapy.

FIGURE 27.3. Contrast-enhanced computed tomography of lacrimal gland lymphoma. At this time, the patient had no systemic disease.



FIGURE 27.4. Contrast-enhanced computed tomography of a patient with a particularly unusual pattern of orbital lymphoma (arrowheads) with ocular invasion (arrows).
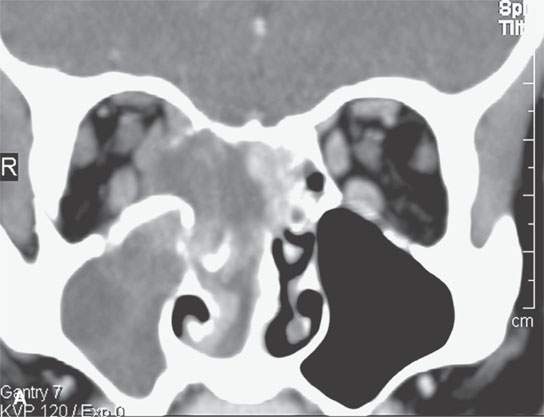

FIGURE 27.5. Contrast-enhanced computed tomography of primary sinonasal lymphoma with orbital invasion and spread to the orbital apex (arrow in B) threatening optic nerve function.
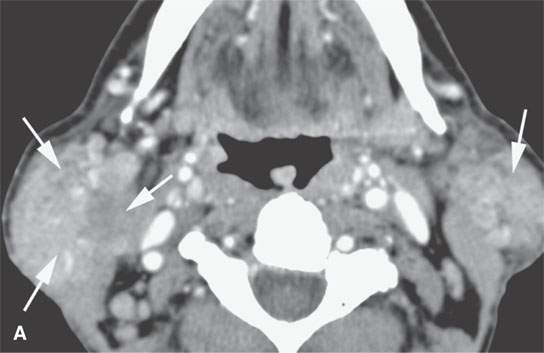
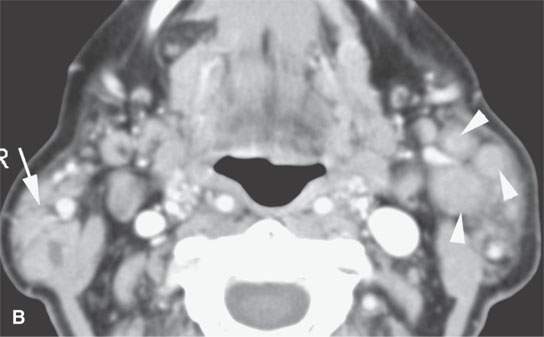
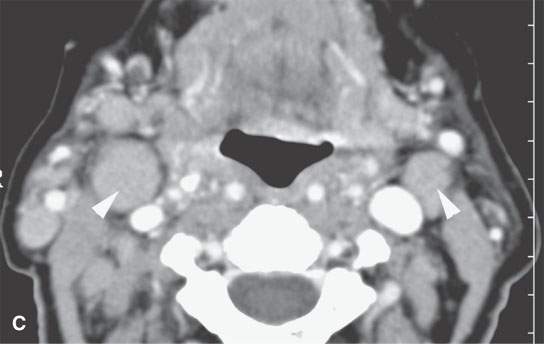
FIGURE 27.6. Contrast-enhanced computed tomography and magnetic resonance imaging studies of a patient with long-standing Sjögren disease with a secondary lymphoma. A–C: Confluent masses showed progressive enlargement on serial studies (arrows). Confluent masses are not necessarily due to lymphoma in this setting; however, the nodal enlargement (arrowheads) prompted biopsy to reveal lymphoma.

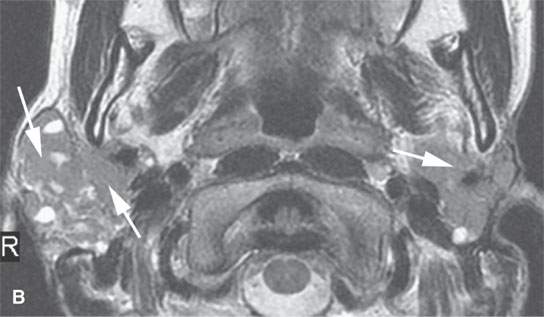
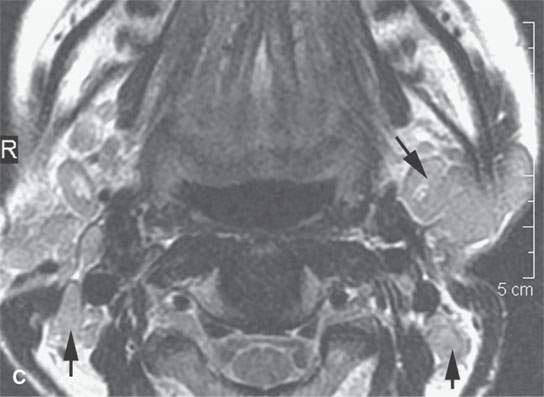
FIGURE 27.7. Magnetic resonance imaging studies of a patient with long-standing Sjögren disease with a secondary lymphoma. A–C: Confluent masses showed progressive enlargement on serial studies (arrows). Confluent masses are not necessarily due to lymphoma in this setting; however, their progressive enlargement (arrowheads) prompted biopsy to reveal lymphoma. A: Contrast-enhanced T1-weighted image. B, C: T2-weighted images.
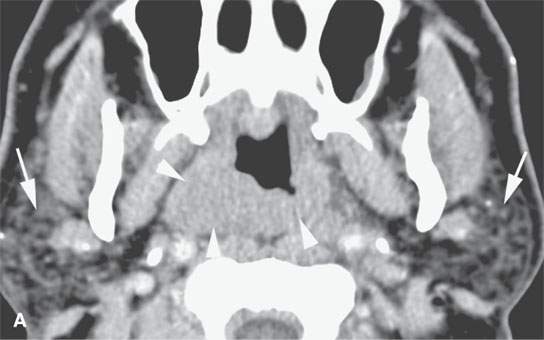
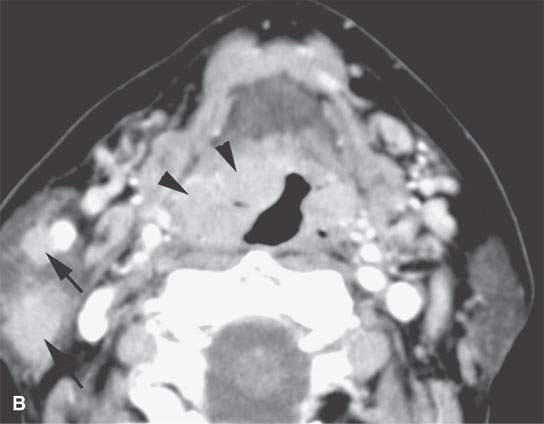
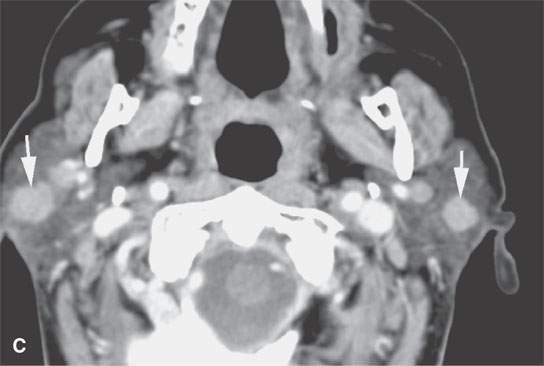
FIGURE 27.8. Contrast-enhanced computed tomography (CT) of a patient with long-standing Sjögren disease (arrows in A) with a secondary lymphoma. The patient developed some suspicious adenopathy clinically leading to this CT. A–C: CT showed an infiltrating mass in the nasopharynx (arrowheads in A) and oropharynx (B) in the lymphoid tissue of the Waldeyer ring (arrowheads). Enlargement of parotid nodes (arrowheads)was also present (arrows in B and C). The findings prompted biopsy that confirmed lymphoma.
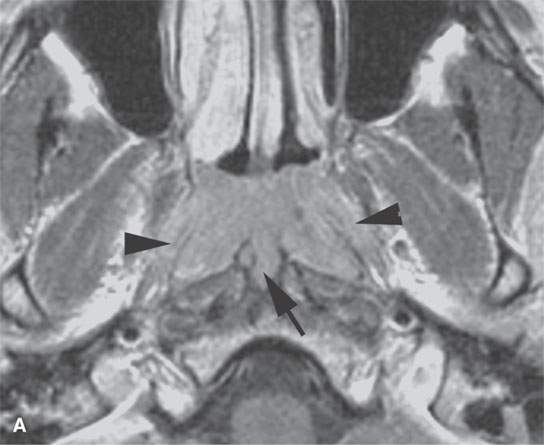

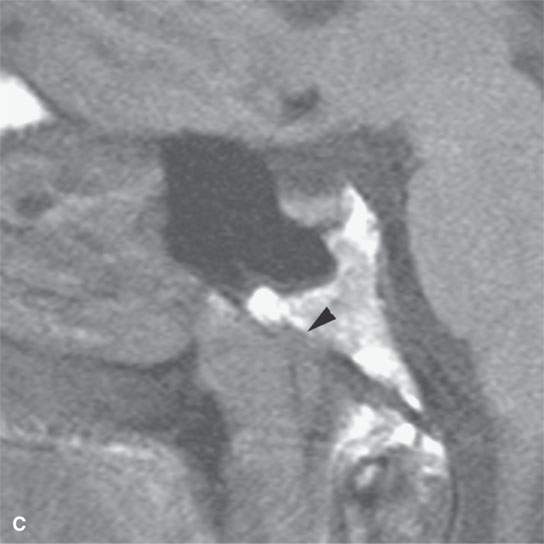
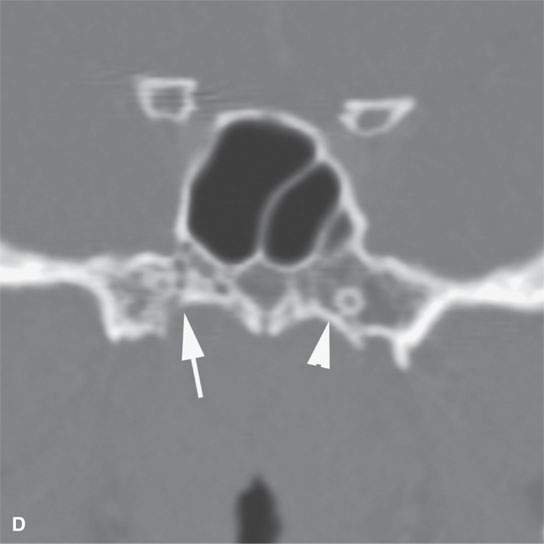
FIGURE 27.9. Contrast-enhanced magnetic resonance demonstrating early infiltrating lymphoma of the nasopharynx. A: Contrast-enhanced T1-weighted (T1W) image shows early infiltration of the parapharyngeal fat and palatal musculature (arrowheads) that border the nasopharynx, suggesting early clival invasion (arrow). B: T2-weighted image correlating with (A) confirms those findings. C: Non–contrast-enhancedT1W image suggest early clival erosions (arrow). D: Computed tomography confirms early cortical bone erosion just to the right of midline (arrow) compared to the normal cortex just to the left of midline (arrowhead).
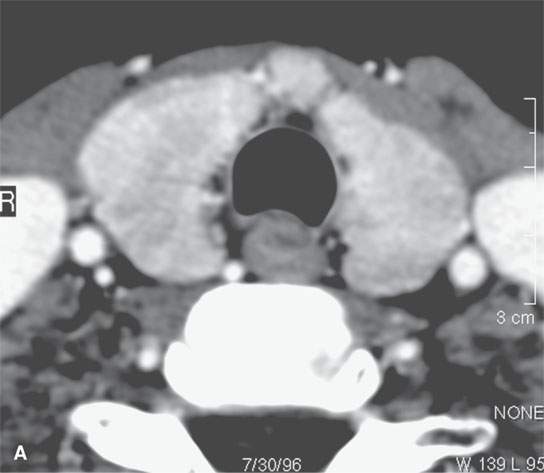
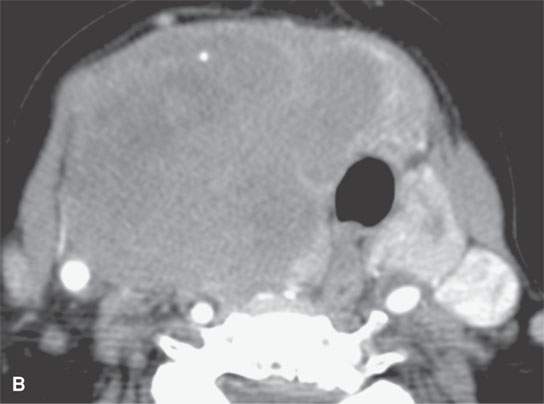
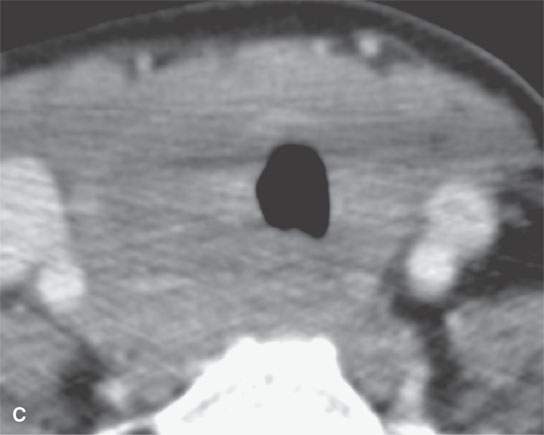
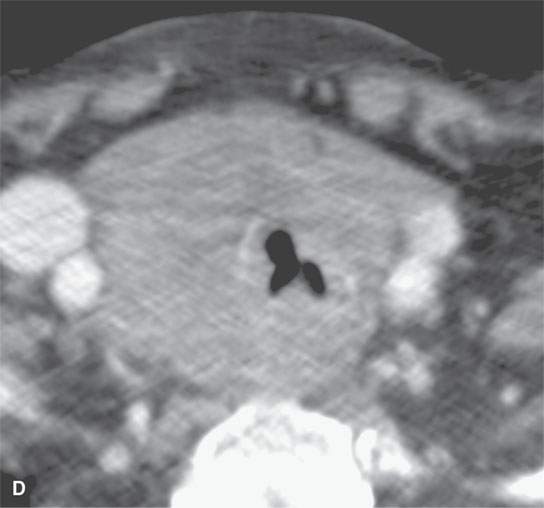
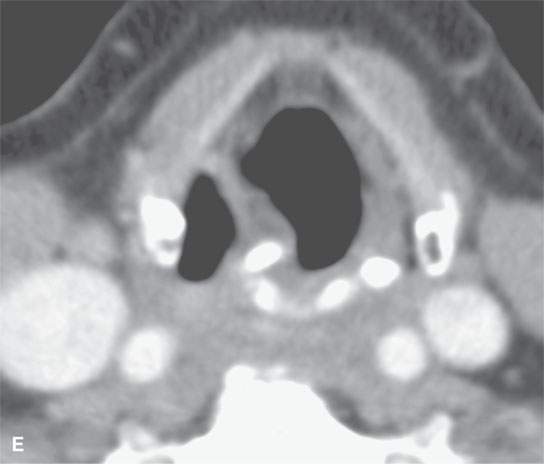
FIGURE 27.10. Contrast-enhanced computed tomography studies of four patients with thyroid lymphoma of various degrees of involvement of the gland and surrounding structures. A;: Bilateral symmetric gland enlargement essentially indistinguishable form other causes of generalized glandular hyperplasia. B: Unilateral enlargement with early spread beyond the gland capsule in a pattern that would also suggest anaplastic carcinoma. C : Diffuse enlargement with extensive spread beyond the gland capsule in a pattern that would also suggest anaplastic carcinoma. D, E: The potential for airway compromise (D) and compromise of adjacent nerves manifest here as true vocal cord weakness (E).
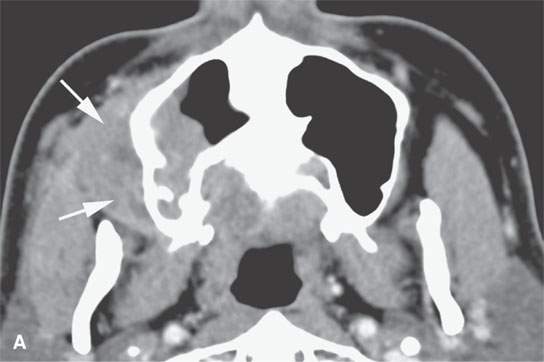
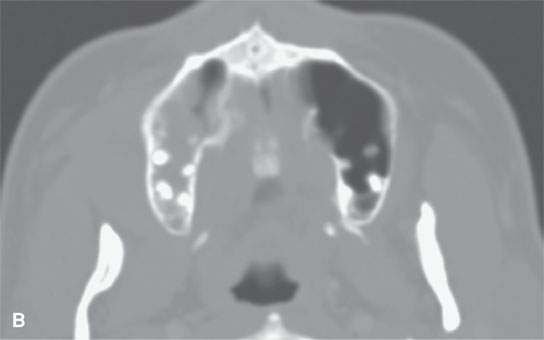
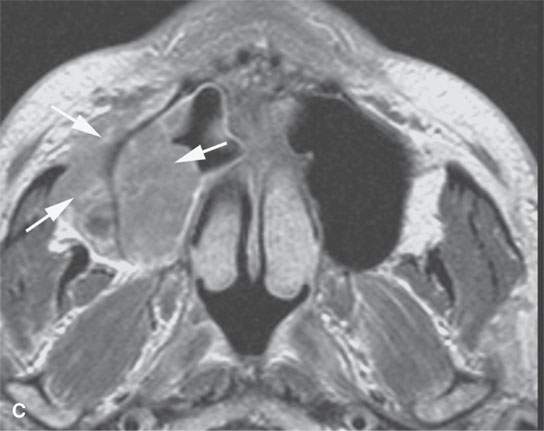
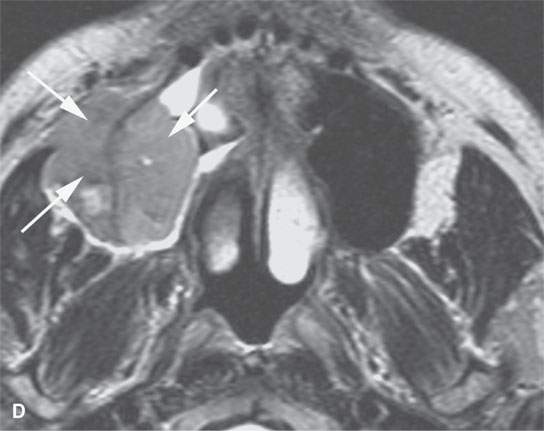
FIGURE 27.11. Contrast-enhanced computed tomography (CECT) and magnetic resonance imaging in a patient with MALT lymphoma. The tumor (arrows) was primary in the region of the maxillary infrastructure and upper gingival buccal sulcus. A, B: CECT. C: Contrast-enhancedT1-weighted image. D: T2-weighted image.
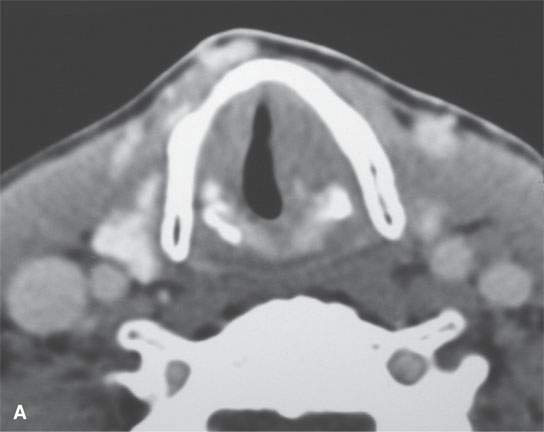
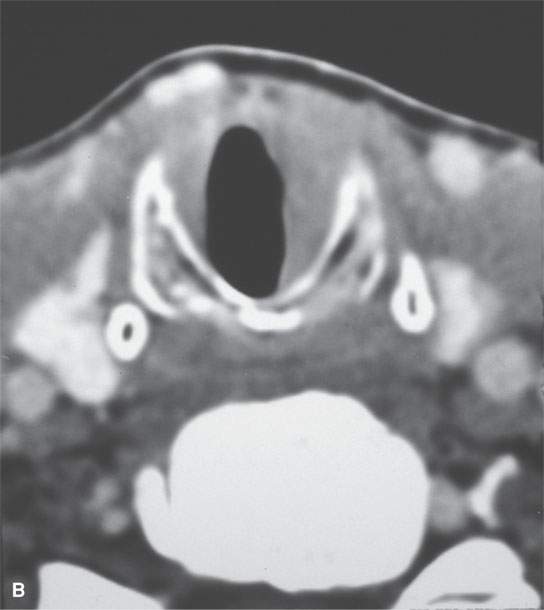
FIGURE 27.12. Contrast-enhanced computed tomography studies of two patients with laryngeal lymphoma. A, B: In the first patient, the lymphoma is confined to the glottic and subglottic levels and is indistinguishable from squamous cell carcinoma. C–E: The second patient had predominantly supraglottic disease with involvement of the false cord and aryepiglottic fold with generalized cervical adenopathy (E).
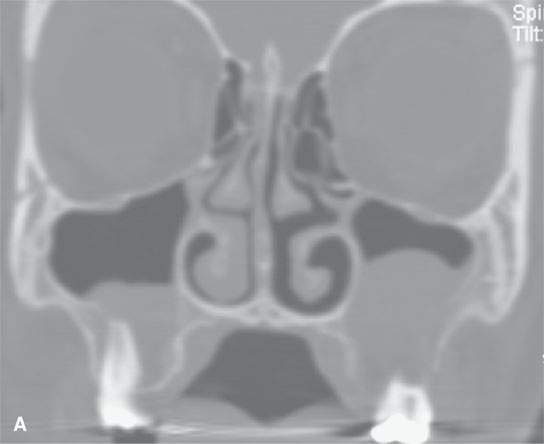

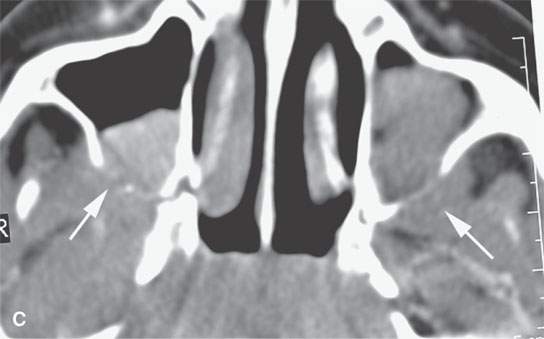
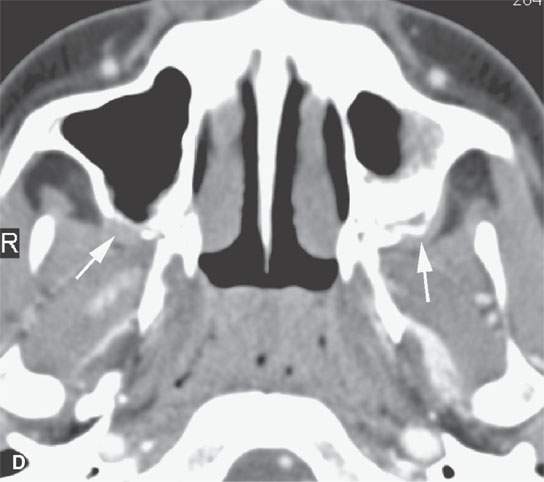
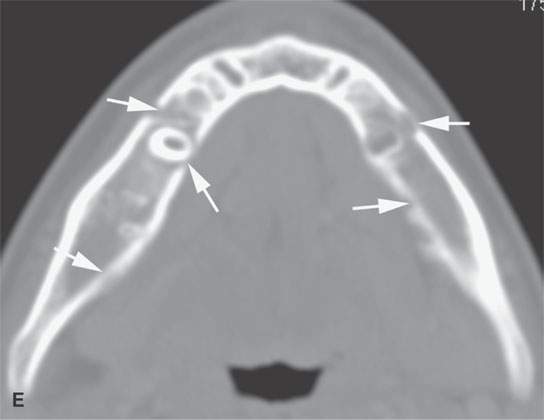
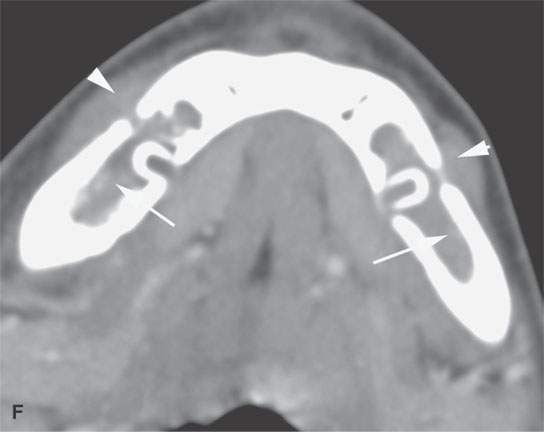
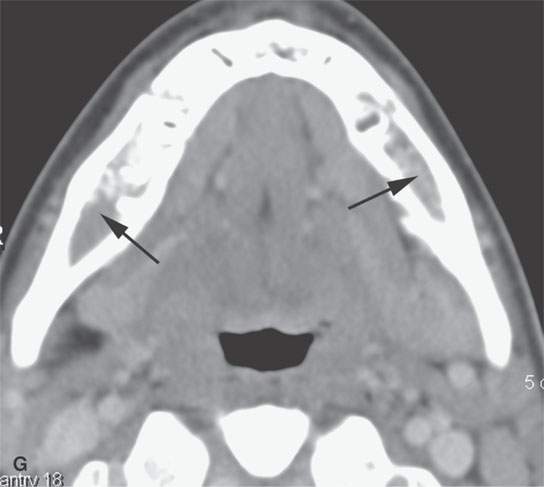

FIGURE 27.13. A 15-year-old male presenting with facial pain and loose teeth proven to be due to Burkitt lymphoma. A–D: Contrast-enhanced computed tomography showing masses involving both upper gingivobuccal sulci and maxillary sinuses with infiltration of the retroantral fat (arrows in C and D). E: Erosion of the lingual and buccal surfaces of the mandible (arrows). F, G:Soft tissue spread (arrowheads) via the mental foramina with tumor filling the mandibular marrow space (arrows) with continued filling of the marrow space (black arrows in G). H: Skull base, orbital, and dural invasion were present as well (arrows).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








