After initial evaluation with radiography, magnetic resonance (MR) imaging is the most common modality used to establish the diagnosis and characterize osseous and soft tissue tumors of the hip. Tumors involving the proximal femur are often benign, and MR imaging can be specific in diagnosing solitary bone cyst, osteochondroma, and chondroblastoma. Benign and malignant soft tissue tumors about the hip are often nonspecific in their MR imaging appearances, but knowledge of the patient’s age may direct a more limited differential diagnosis. In the setting of malignancy, MR imaging is commonly used to stage tumors and follow patients postoperatively.
Key Points
- •
After initial evaluation with radiography, magnetic resonance (MR) imaging is the most common modality used to establish the diagnosis and characterize osseous and soft tissue tumors of the hip.
- •
Tumors involving the proximal femur are often benign, and MR imaging can be specific in diagnosing solitary bone cyst, osteochondroma, and chondroblastoma.
- •
Osseous metastases and myeloma are the most common causes of malignancy in patients older than 40 years, with metastases being 25 to 30 times more common than primary malignancy of bone.
- •
Benign and malignant soft tissue tumors about the hip are often nonspecific in their MR imaging appearances, but knowledge of the patient’s age may direct a more limited differential diagnosis.
- •
Fibrosarcoma and rhabdomyosarcoma are common in young children, and liposarcoma and undifferentiated pleomorphic sarcoma are more common in middle-aged and elderly populations.
Introduction
Magnetic resonance (MR) imaging of hip tumors is often obtained for imaging finding discovered on radiographs or for further evaluation of a soft tissue mass found on clinical examination. MR imaging is the most common modality used to establish the diagnosis and characterize osseous and soft tissue tumors of the hip. Tumors involving the proximal femur are often benign, and MR imaging can be fairly specific in diagnosing lesions such as solitary bone cyst, osteochondroma, and chondroblastoma. Osseous metastases and myeloma are the most common causes of malignancy in patients older than 40 years of age, and should be suspected when multiple lesions are present. Benign and malignant soft tissue tumors about the hip vary according to age, and their MR imaging features are often times nonspecific. This report will provide an MR imaging pictorial for some of the more common tumors of the hip.
Introduction
Magnetic resonance (MR) imaging of hip tumors is often obtained for imaging finding discovered on radiographs or for further evaluation of a soft tissue mass found on clinical examination. MR imaging is the most common modality used to establish the diagnosis and characterize osseous and soft tissue tumors of the hip. Tumors involving the proximal femur are often benign, and MR imaging can be fairly specific in diagnosing lesions such as solitary bone cyst, osteochondroma, and chondroblastoma. Osseous metastases and myeloma are the most common causes of malignancy in patients older than 40 years of age, and should be suspected when multiple lesions are present. Benign and malignant soft tissue tumors about the hip vary according to age, and their MR imaging features are often times nonspecific. This report will provide an MR imaging pictorial for some of the more common tumors of the hip.
Imaging protocol
MR imaging has emerged as the preferred modality for evaluating both osseous and soft tissue masses of the hip by providing information for both diagnosis and staging. Lesions should be imaged in at least 2 orthogonal planes, using fast spin echo T1-weighted and fluid-sensitive MR pulse sequences in at least 1 of these planes. Fat suppression on T2-weighted images is useful to increase lesion-to-background signal intensity differences for high signal intensity lesions that are located within the marrow or fatty soft-tissue. Fat suppression imaging is also useful in decreasing or eliminating the MR signal from fat, allowing increased conspicuity of lesions containing paramagnetic substances (eg, methemoglobin) on T1-weighted images, and in identifying contrast enhancement. Gradient-echo imaging in a single plane may be a useful adjunct in demonstrating hemosiderin in lesions that have hemorrhaged.
In general, a small field of view is preferred; however, imaging of the entire pelvis in at least 1 plane is advised for appropriate staging. It is useful to place a marker over the area of clinical concern to ensure that it is appropriately imaged, especially in cases of suspected subcutaneous lipoma or lipomatosis, in which case the lesion may not be appreciated as distinct from the adjacent adipose tissue. Contrast enhancement is often not required; however, we find it useful in the detection of underlying tumors in the presence of hemorrhage.
Benign osseous tumors
Most tumors involving the proximal femur are benign. The most common primary tumors and pseudotumors of the hip include fibrous dysplasia, solitary bone cyst, osteoid osteoma, chondroblastoma, giant cell tumor, osteochondroma, aneurysmal bone cyst, and Langerhans cell histiocytosis.
Solitary Bone Cyst
Solitary (or unicameral) bone cyst is most commonly found in the proximal humerus but is located in the proximal femur in up to 21% of cases. Solitary bone cysts are nonaggressive, unilocular lesions that have a predilection for the metaphyses of long bones. Lesions can have associated cortical thinning; mild expansile remodeling; well-defined or sclerotic margins on radiography, computed tomography (CT), or MR imaging; and absent internal matrix on radiography ( Fig. 1 ). In the proximal femur, it may be difficult to differentiate from the cystic variant of fibrous dysplasia on both imaging and pathologic evaluation.
Osteochondroma/Multiple Hereditary Exostosis
Osteochondroma is the most common bone tumor and is categorized as a developmental lesion as opposed to a true neoplasm. Osteochondroma accounts for 20% to 50% of all benign bone tumors and 10% to 15% of all bone tumors. Osteochondromas are composed of cortical and medullary bone with an overlying hyaline cartilage cap, have medullary and cortical continuity with the parent bone, and may be sessile or penduculated. The femur is the most commonly affected bone (30% of cases), with the distal femur affected 3 times more often than the proximal femur.
MR imaging confirms the cortical and medullary continuity with the parent bone, and the medullary component will closely approximate the signal of the adjacent marrow on all sequences ( Fig. 2 ). The hypointense cortical margin can be variable in thickness. The cartilaginous cap is variable in signal depending on its water content, mineralization, and age of the patient; young patients with active growth may demonstrate marked heterogeneity of the cartilaginous cap on all sequences. Because malignant transformation can occur in 1% of solitary osteochondromas and in 3% to 5% of patients with hereditary multiple exostoses, MR imaging can be helpful in assessing malignant features. Continued lesion growth and a hyaline cartilage cap greater than 2 cm in thickness after skeletal maturity is suggestive of malignant transformation. MR imaging has 100% sensitivity and 98% specificity for differentiating osteochondromas and chondrosarcoma when cartilage cap thickness of 2 cm was used as a threshold. MR imaging is also helpful in assessing complications such as fractured stalk of a pendunculated osteochondroma, neurovascular compromise by mechanical compression, and overlying bursitis.
Hereditary multiple exostoses (HMEs) (also known as diaphyseal aclasis or familial ostechondromatosis) is an autosomal dominant disorder in which multiple osteochodromas are present. Osseous deformities involving the proximal femur are relatively common, with a 25% prevalence rate of coxa valga deformity. Axial T1-weighted imaging will show the characteristic MR imaging features of osteochondromas (as discussed previously) but with multiplicity and often deformity of the involved and adjacent bones ( Fig. 3 ).
Chondroblastoma
Chondroblastoma accounts for less than 2% of benign primary bone tumors and usually involves the epiphyseal or apophyseal regions in skeletally immature patients. Chondroblastoma occurs twice as often in male patients, and most lesions occur between the ages of 5 and 25 years. The most common clinical presentation is protracted pain, and some patients may have some loss of joint function. The most common anatomic location of this tumor is in the proximal femur, followed by the distal femur, proximal tibia, proximal humerus, hands, and feet ( Fig. 4 A). Chondroblastoma presents on radiographs as a lucent lesion in the epiphysis or apophyseal equivalent and may have subtle chondroid matrix, adjacent periosteal reaction and expansile remodeling if secondary aneurysmal bone cyst is present (which can occur in 15% of cases) (see Fig. 4 A). MR imaging accurately demonstrates the extent of the actual tumor and the classic, adjacent marrow edema-like signal changes (see Fig. 4 B–D). Rarely, the lesion may extend extraosseously into the hip joint, resulting in reactive synovitis. The differential diagnosis of chondroblastoma includes giant cell tumor. Patients are often treated with curettage and bone grafting, although there is a report in the literature about further supplementation with vascularized fibular graft.
Malignant osseous tumors
Metastases and myeloma are the most common causes of malignancy in the proximal femur in patient older than 40 years of age, because the proximal femurs contain hematopoietic marrow. However, the most common primary malignant osseous tumors are chondrosarcoma (24%), Ewing sarcoma (16%), osteosarcoma (9%), and fibrosarcoma/malignant fibrous histiocytoma (5%).
Metastasis
Osseous metastasis is the most common bone malignancy, occurring 25 to 30 times more frequently than primary malignant tumors of bone. In children younger than 2 years, neuroblastoma should be highly considered. It will appear as multifocal lytic lesions on radiographs and marrow-replacing lesions on MR imaging, and it may simulate the appearance of osteomyelitis. Whole-body MR imaging can substitute for skeletal scintigraphy in detecting skeletal metastases in children and is helpful in evaluating initial tumor staging and early treatment response, but it has only a complementary role with conventional oncologic imaging methods for the detection of extraskeletal metastases. In the adult population, the MR imaging characteristics of multiple marrow-replacing lesions are often nonspecific, and correlation with the primary source of malignancy should be sought ( Fig. 5 ).
Myeloma
Plasma cell myeloma (more commonly known as myeloma) is the most common primary bone malignancy. It is a malignant clonal neoplasm of plasma cells of B-lymphocyte origin, resulting in the overproduction of monoclonal immunoglobulins. Myeloma is characterized by osteolytic lesions, bone pain, hypercalcemia, monoclonal gammopathy, and disorders caused by amyloid deposition. Plasma cell myeloma most commonly presents in the 6th and 7th decades, and men and women are affected equally. The diagnosis is made in a clinical setting of symptomatic and progressive disease using a combination of bone marrow biopsy, serum IgG and IgA levels, urine immunoglobulin levels, and lytic bone lesions.
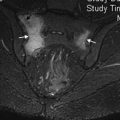
Imaging can detect the extent of intramedullary disease, any extramedullary myelomatous foci, complications, and treatment response. Bones containing red marrow are most frequently involved, such as the vertebrae, ribs, skull, pelvis, femur, clavicle, and scapula. Imaging findings of multiple myeloma include osteopenia, lytic lesions, and pathologic fracture. The lytic lesions are typically “punched out” but can exhibit expansile remodeling of the adjacent bone. In the sclerotic form of myeloma, there is usually a mixed pattern of lytic and sclerotic lesions; the number of sclerotic foci is usually limited but can be extensive. Osteosclerotic myeloma can also be associated with POEMS (polyneuropathy, organomegaly, endocrinopathy, monoclonal gammopathy, skin changes) syndrome. On MR imaging, myeloma can have several patterns – focal lesions (localized), complete replacement of the marrow (diffuse), or innumerable small marrow-replacing lesions (variegated) ( Fig. 6 ). Plasmacytoma is a solitary myelomatous lesion that is typically isointense to skeletal muscle on T1-weighted imaging and hyperintense to muscle on T2-weighted imaging. Isolated reports of a “mini-brain” MR appearance of plasmacytoma in the spine and proximal femur describe the enhancing, radial distribution of tumor separated by thickened bony trabeculae.