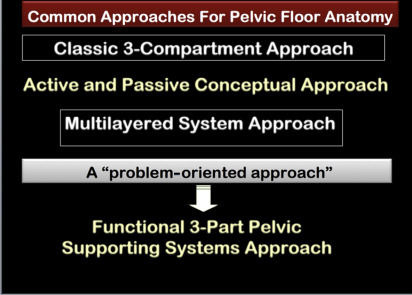
This article reviews different approaches for describing pelvic floor anatomy; “Classic 3-Compartment Approach”, “Active and Passive Conceptual Approach” and “Multilayered System Approach”. However, these approaches cannot explain pathogenesis of various dysfunctions. “Functional 3-Part Pelvic Supporting Systems Approach” a new, more function-based classification of the pelvic floor support system is introduced in which all structures that contribute to same function are grouped under 1 system. Indications for MR imaging of pelvic floor dysfunction, patients’ preparation, static, dynamic and MR Defecography imaging protocols are detailed according to the concordance of experts in two recently published consensus papers.
Key points
- •
The “classic 3-compartment approach,” “active and passive conceptual approach,” and the “multilayered system approach” are established different approaches for description of pelvic floor anatomy.
- •
The “functional 3-part pelvic supporting systems approach,” a new, more function-based classification of pelvic floor support system, is discussed in detail.
- •
Indications, patients’ preparation, and hardware requirements for MR imaging of pelvic floor dysfunction and MR-defecography are included.
- •
The MR imaging protocols define the most important prerequisites for a diagnostic MR examination according to the concordance of experts from European Society of Urogenital Radiology, European Society of Gastrointestinal and Abdominal Radiology, and Society of Abdominal Radiology societies.
Introduction
Pelvic floor disorders are often complex with symptoms ranging from vague low back pain to major fecal incontinence and urinary incontinence.
Symptoms are divided arbitrarily into different areas: urinary disorders, fecal disorders, sexual dysfunction, and pelvic discomfort, although symptoms of all types often coexist in the same individual.
When a patient presents for evaluation, she may be unaware that many of her symptoms may be related to pelvic floor dysfunction (PFD). The clinician should elicit a comprehensive history encompassing all pertinent areas. Obtaining a comprehensive history is a particular challenge in reconstructive pelvic surgery, in which anatomic aberrations are often striking, but understanding the symptoms related to them is inadequate. The reoperation rate after initial pelvic floor surgery is reported to be approximately 29%. The commonness of the need for reoperation indicates that better treatments are necessary; however, clinicians specialized in this field affirmed that such improvement will be possible only if research clarifies the causative mechanisms and the reasons that surgery fails.
Magnetic resonance (MR) imaging has been effectively used to evaluate PFD, with very good reported sensitivity, specificity, and positive predictive value. The modality relies on (a) static sequences with a high spatial resolution to delineate the passive and active elements of the pelvic organ support system and (b) fast imaging dynamic (cine) sequences during straining and evacuation to detect functional abnormalities. This article reviews in detail the basic essential anatomic information the radiologist needs to know to become competently capable not only of writing a full report based on solid scientific information but also of providing state-of-the art care for patients who present for MR imaging for PFD. Full competence means that the radiologist will know the steps for taking a full relevant medical history, can confidently determine which radiologic studies to order to allow for a detailed diagnostic report, to know the mandatory steps for patient preparation, and to assemble the MR imaging findings in a schematic to best meet the needs of the urologist, gynecologist, and proctologist who will treat the patients.
Overview of Pelvic Floor Normal Anatomy
There are several approaches for functional description of pelvic floor ( Fig. 1 ):
- A.
Classic 3-compartment approach
- •
The pelvic floor is divided into the following 3 major compartments:
Anterior : Includes urinary bladder, urethra, and urethral support system
Middle : Includes vagina (anterior and posterior wall) and uterocervical support
Posterior: Contains rectum and supporting structure
- •
Patients with abnormalities in 1 compartment often have disorders in another
- •
- B.
Active and passive conceptual approach
- •
Pelvic floor components are divided into passive and active structures
- ○
Passive structures
- ▪
Pelvic bones
- ▪
Supportive connective tissue
- ▪
- ○
Active structures
- ▪
Pelvic floor muscles
- ▪
- ○
- •
This classification cannot precisely explain pathogenesis of various dysfunctions.
- •
- C.
Multilayered system approach
- •
Considers passive and active components of pelvic floor as an integrated multilayer system , organized from cranial to caudal into the following:
- ○
First layer: Endopelvic fascia
- ○
Second layer: Pelvic diaphragm
- ○
Third layer: Urogenital diaphragm
- ○
Fourth layer: Perineum
- ○
- •
- D.
Functional 3-part pelvic supporting systems approach ( Fig. 2 )
- •
The components of this functional approach are described in full detail in the later discussion, “Static MR Images” of the pelvic floor examination.
- •
It is a new, more function-based classification of pelvic floor support system.
- •
This approach is based on fact that each passive and active structural component of the pelvic floor plays a role in urinary and fecal continence, preventing pelvic organ prolapse. In this approach, all structures that contribute to the same function are grouped under 1 system.
- ○
Urethral support system
- ▪
Structures that maintain urinary continence:
- •
Urethral support ligaments
- •
Level III endopelvic fascia
- •
Puborectalis muscle
- •
- ▪
- ○
Vaginal support system:
- ▪
Supporting elements that prevent prolapse:
- •
Level I and II endopelvic fascial
- •
Iliococcygeus muscle
- •
- ▪
- ○
Anal sphincter complex:
- ▪
Anal sphincter muscles together with other supporting elements maintain fecal continence
- ▪
- ○

Fig. 2
The Functional 3-Part pelvic support system approach and the components of each system. ( A ) Urethral support system. ( B ) Vaginal support system. ( C ) The anal sphincter complex. Arrow points to internal anal sphincter. Arrowhead points to submucosal smooth muscle. U, urethra; V, vagina; UB, urinary bladder.
- •
Multilayered System Approach
Essential anatomic and functional information to understand the concept of the “Multilayered system approach” includes the following:
Supportive connective tissue
Supportive connective tissue is a complex network of connective tissue, and variations occur between the main components according to the type of the supportive structures :
- A.
Ligaments:
- •
Form a well-defined layer composed of specialized aggregation of connective tissue and have well-organized fibrous collagen
- •
Include arcus tendineus levator ani (ATLA) and arcus tendineus fascia pelvis ligaments, which are dense, obliquely oriented linear pure connective tissue structures at the pelvic sidewall
- •
- B.
Endopelvic fascia:
- •
Forms a diffuse layer that consists of less well-defined connective tissue
- •
Has a functional correlation, whereby it envelops pelvic organs, including parametrium and paracolpium, giving support to the uterus and upper vagina, respectively ,
- •
Layers of pelvic support
(a) First layer: Endopelvic fascia
- •
Parametria includes broad, cardinal, and uterosacral ligaments
- •
Paracolpium refers to connective tissue that attaches vagina to pelvic walls ( Fig. 3 )
- ○
Anteriorly, pubocervical fascia and ligaments extend from the posterior surface of the pubis to the cervix, giving support to the bladder
- ○
Posteriorly, rectovaginal fascia inserts into the perineal body, levator plate, and uterosacral ligament. It support the rectum and forms a restraining layer that prevents the rectum from protruding forward, blocking formation of a rectocele ( Fig. 3 A)

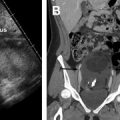
Fig. 3
( A ) Overview of the pelvis shows the fascia with the bladder, cervix, and rectum cut away. Endopelvic fascia is a continuous adventitial layer, covering the pelvic diaphragm and viscera. It is a complex network of connective tissue composed of collagen, fibroblasts, elastin, smooth muscle cells, and neurovascular bundles. Ligaments are a more well-defined aggregate of connective tissue. ( B ) The type of support the vagina receives at each level (uterus removed). In level I (suspension), the paracolpium suspends the vagina from the lateral pelvic walls. Fibers of level I extend both vertically and posteriorly toward the sacrum. In level II (attachment), the vagina is attached to the arcus tendineus fasciae pelvis and the superior fascia of levator ani. In level III (fusion), the vagina, near the introitus, is fused laterally to the levator ani. ( C ) Axial oblique T2WI TSE MR image shows the arcus tendineus fascia pelvis (ATFP) ( arrows ) on either side of the symphysis pubis.
( From [(El Sayed RF . Overview of the Pelvic Floor. In: Shaaban AM, Editor. Diagnostic Imaging: Gynecology 2nd Edition. Philadelphia: Elsevier-Amirsys; 2015. 8/2 -8/28 ; with permission.)
- ○
- •
Levels of vaginal support
Pubocervical fascia is divided into 3 levels ( Fig. 3 B, C)
- •
Level I (suspension)
- ○
Upper portion of the vagina adjacent to the cervix (cephalic 2 to 3 cm of the vagina)
- ○
Suspended from above by relatively long connective tissue fibers of the upper paracolpium
- ○
Functional significance: it provides upper vaginal support
- ○
- •
Level II (attachment)
- ○
Is a midportion of the vagina
- ○
The paracolpium becomes shorter at this level
- ○
Attaches the vaginal wall more directly to arcus tendineus fascia pelvis
- ○
Stretches the vagina transversely between the bladder and rectum
- ○
- •
Level III (Fusion)
- ○
Corresponds to the region of the vagina that extends from the introitus to 2 to 3 cm above the hymenal ring
- ○
Near introitus, the vagina is fused laterally to levator ani
- ○
Posteriorly, attaches to perineal body
- ○
Anteriorly, blends with the urethra
- ○
At this level, there is no intervening paracolpium between the vagina and the adjacent structures, as opposed to levels I and II
- ○
- •
(b) Second layer: Pelvic diaphragm
- •
Definition : Formed by coccygeus and levator ani muscles and acts as a shelf to support pelvic organs ( Fig. 4 )