Chapter Outline
Protocols for Magnetic Resonance Imaging of the Gastrointestinal Tract
Patient Preparation and Intraluminal Contrast Material
Magnetic resonance imaging (MRI) of the gastrointestinal tract takes advantage of the inherent outstanding soft tissue contrast of MRI to provide excellent depiction of inflammatory, infectious, ischemic, and neoplastic gastrointestinal diseases. By combining fast imaging pulse sequences with intraluminal and intravenous (IV) contrast agents, MRI can show the normal and diseased bowel wall as well as adjacent inflammatory and neoplastic changes involving the mesentery, peritoneum, and omentum.
Imaging the gastrointestinal tract presents significant challenges that can be met with current MRI techniques. In the past, slower MR pulse sequences required several minutes to acquire, resulting in degraded image quality because of bowel peristalsis and respiratory motion. Current high-field MR scanning represents a confluence of hardware and software development that has resulted in fast MRI scans, obtained in a few seconds. Breath-hold precontrast and dynamic breath-hold, contrast-enhanced MRI of the abdomen and pelvis can easily be performed, with outstanding image quality.
Extracellular IV MR contrast agents are relatively inexpensive and have a long track record of safety and efficacy for evaluating abdominal diseases. Intraluminal contrast agents can be administered using over-the-counter (OTC) agents or commercially available oral contrast material.
Protocols for Magnetic Resonance Imaging of the Gastrointestinal Tract
MRI of the gastrointestinal (GI) tract uses rapid breath-hold acquisitions to minimize motion artifacts. Each manufacturer has pulse sequences available that can be optimized for MRI of the GI tract. Although they have different acronyms, similar pulse sequences and image types are available on scanners from all the major MR manufacturers. The specific pulse sequence parameters, however, will be vendor-specific.
For a general evaluation of the GI tract, we use breath-hold, single-shot (SS) rapid acquisition with relaxation enhancement (RARE) imaging in the axial and coronal planes. This pulse sequence is known by a number of different acronyms, including single-shot fast spin-echo (SSFSE), single-shot turbo spin-echo (SSTSE), and half-Fourier acquisition single-shot turbo SE (HASTE). These single-slice images are breathing-independent and are thus insensitive to respiratory or peristaltic motion. They provide heavily T2-weighted images and an excellent overall abdominal and pelvic survey. Water-soluble intraluminal contrast material demonstrates high signal intensity, whereas the bowel wall is depicted as a thin, intermediate signal intensity line surrounding the bowel contents. Intestinal mural thickening is depicted on single-shot RARE images when the bowel wall measures more than 3 mm. Single-shot images are obtained without fat suppression.
Unenhanced T1-weighted images depict anatomic structures. 2D or 3D spoiled gradient-echo T1 sequences can be obtained with simultaneous acquisition of in-phase and opposed-phase images. Newer Dixon T1 sequences apply Dixon fat and water separation to the 3D gradient echo images, providing in-phase, opposed-phase, fat-only, and water-only images in a single breath-hold. The Dixon water image provides a precontrast fat-suppressed image that can be compared to the dynamic postcontrast images to assess inflammatory or malignant bowel wall enhancement. Depending on the vendor, Dixon MR sequences are known by the acronyms LAVA-Flex, m-Dixon, and 2-point Dixon.
Fat-suppressed, T2-weighted, fast spin-echo (FSE) images are obtained to distinguish intestinal mural edema from fibrosis. This important distinction may assist in differentiating an acute inflammatory process with wall thickening from a thickened wall caused by a chronic fibrotic stricture. An acute inflammatory stricture will show high signal intensity edema in the thickened bowel wall, whereas the thickened fibrotic wall of a chronic stricture will demonstrate low signal intensity. Fat-suppressed, T2-weighted images may be obtained with breath-holding or with respiratory triggering.
Diffusion-weighted imaging (DWI) uses fast, single-shot echo planar sequences, which are sensitive to the microscopic movement of water protons. Many benign and malignant diseases are characterized by restriction of diffusion and are displayed as areas of altered signal on DWI. DWI has become an integral part of body MRI protocols and is essential for GI imaging. The DWI sequence may be obtained during breath-holding or free breathing, or may be combined with respiratory triggering. For GI imaging, an intermediate B value of 400 to 500 s/m 2 provides images with a good balance between adequate diffusion weighting and reasonable anatomic depiction. Higher B values will increase diffusion weighting at the expense of the image signal-to-noise ratio (SNR) and anatomic depiction. DW images are characterized by a high target to background signal, so that diseased bowel is seen with high contrast and conspicuity compared with the relatively suppressed background tissue and intraluminal contents.
Diffusion-weighted images may be displayed as a magnitude image, which is a combination of diffusion signal and T2-shine through, or as an apparent diffusion coefficient (ADC) map. On the ADC map, the T2 component of the image signal is removed so that only areas of true restricted diffusion are displayed. Quantitative measurements of ADC values on these images requires obtaining two or more different B values. I currently acquire three B values, at 20, 500, and 800 s/m 2 . Quantitative measurements of ADC values may be useful to characterize GI masses and monitor the response of tumors to therapy.
Another sequence commonly used for GI tract imaging is balanced, steady-state free precession (SSFP) sequences. The image contrast is determined by T2* and T1 properties, depending heavily on repetition time (TR). The speed and relative motion insensitivity of this acquisition are useful features for GI imaging. On the balanced SSFP images, water-soluble intraluminal contrast material, blood, bile, ascites, and urine will all demonstrate high signal intensity.
Vendor acronyms for this pulse sequence include balanced turbo field-echo (b-TFE), and fast imaging employing steady-state acquisition (FIESTA), and true fast imaging with steady-state precession (true FISP). The balanced SSFP images show excellent homogeneity of luminal signal and visualization of the normal and diseased bowel wall. Compared to 3D gradient-echo images, the balanced SSFP images are less sensitive to motion artifact but show increased sensitivity to chemical shift and susceptibility artifacts.
Following the IV injection of gadolinium, two sets of axial, fat-suppressed, gradient-echo MR images are obtained through the abdomen and pelvis. One may use 2D or 3D gradient-echo imaging. The 2D gradient-echo images use a thicker slice thickness of 8 to 10 mm but are typically sharper and have a greater range of contrast than 3D gradient-echo images. The 3D images have a thinner slice thickness and provide more efficient coverage of the abdomen and pelvis. A typical slice thickness for 3D images is 4 mm. Some 3D acquisitions incorporate a fixed or variable slice overlap. The newer 3D Dixon sequences may be used for dynamic postcontrast imaging. The Dixon water image provides very homogeneous fat suppression, with higher SNR and reduced susceptibility artifact.
Water-soluble intraluminal contrast material demonstrates low signal intensity on the fat-suppressed, gadolinium-enhanced (GE) MR images. The bowel wall is shown as rings or lines surrounding the bowel lumen. The thickness of the normal bowel wall is 3 mm or less. The normal bowel wall will show gadolinium enhancement equal to or less than that of the liver parenchyma. Abnormal mural thickening or enhancement can be evaluated as signs of inflammatory or neoplastic intestinal disease.
Important features of the optimized GE MR image include fat suppression, image homogeneity, high-n plane resolution, and breath-hold imaging. In practice, we combine dynamic 3D gradient-echo imaging in the axial plane followed by coronal and sagittal 3D GE imaging and delayed 2D gradient-echo imaging. The delayed 2D gradient-echo images are often most useful for depicting intestinal mural disease and adjacent disease of the peritoneum, showing excellent image sharpness and contrast conspicuity. The 2D images are also less susceptible to breathing artifacts, which may be more common at the end of the examination.
This MR examination of the GI tract can be performed in 20 to 25 minutes. Specific imaging parameters are listed in Table 6-1 .
| Sequence | SSFSE | T1 GE | T2 SSFSE | DWI | Gad 3D GE | Gad 3D GE | Gad 3D GE | Delayed 2D GE |
|---|---|---|---|---|---|---|---|---|
| Plane | Coronal | Axial | Axial | Axial | Axial | Coronal | Sagittal | Axial |
| Anatomy | A & P | A & P | A & P | A & P | A & P | A & P | A & P | A & P |
| Scan time(s) | 0.12 | 0.22 | 0.24 | 0.24 | 0.24 | 0.24 | 0.24 | 0.22 |
| COIL: PHASED-ARRAY SURFACE COIL | ||||||||
| FOV (cm) | 44 | 38 | 38 | 38 | 38 | 44 | 44 | 38 |
| Phase FOV | 0.8 | 0.8 | 1 | 0.8 | 1 | 0.8 | 0.8 | |
| TR (msec) | Min | 172 | Min | 3750 | 4 | 4.4 | 4.4 | 100 |
| TE (msec) | 80 | 4.4/2.2 | 90 | Min | 1.7 | 1.7 | 1.7 | Min full |
| Matrix | 352 × 224 | 320 × 224 | 320 × 224 | 192 × 224 | 320 × 256 | 320 × 224 | 320 × 224 | 256 × 192 |
| Nex | 0.6 | 1 | 1 | 2 | 1 | 1 | 1 | 1 |
| Slice thickness (mm) | 8 | 4 | 8 | 8 | 4 | 4.4 | 4 | 8 |
| Overlap | 2 | 2 | 2.2 | 2.2 | ||||
| Flip angle (degrees) | 90 | 80 | 90 | 90 | 12 | 12 | 12 | 70 |
| ASSET | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| Fat suppression | No | No | Yes | SPIR | Yes | Yes | Yes | Yes |
| B value (s/m 2 ) | 20, 500 | |||||||
| ETL | ||||||||
| BW | 83.3 | 83.3 | 83.3 | 125 | 125 | 83.3 | 31.25 | |
| Options | Pure | Pure | Pure | Pure 3 in 1 | Pure | Pure | Pure | Pure, ZIP 512 |
Coil Selection
Coil selection will depend on the availability of surface coils for a specific MR scanner. Dedicated surface coils, with larger areas of anatomic coverage, are now routinely available from all vendors. I typically require 48-cm coverage in the craniocaudal direction when imaging the abdomen and pelvis. There are now surface coils available that provide this extensive coverage, allowing for combined abdominal and pelvic imaging. One should be careful not to sacrifice image homogeneity when using a dedicated surface coil. Inhomogeneous images can create problems when assessing subtle GI tract or peritoneal disease. Some form of intensity correction algorithm should be used to maximize the homogeneity of the images. Ultimately, phased-array surface coils combined with parallel imaging provides optimal signal and speed of image acquisition.
Patient Preparation and Intraluminal Contrast Material
Contrast Agents
All patients are asked not to eat or drink for the 4 hours prior to their MRI appointment. If rectal water is to be administered, patients administer a Fleet’s enema prior to the examination. If more thorough bowel cleansing is desired, patients are also asked to have a clear liquid diet starting for 12 hours prior to the MRI examination and to take four bisacodyl tablets orally the evening prior to the appointment.
The use of intraluminal contrast material is an essential element of the MRI protocol for GI tract imaging. Oral and or rectal contrast material will distend the stomach, small intestines, and colon, improving the depiction of inflammatory or neoplastic mural disease. Subtle mural thickening can be easily masked by collapsed segments of bowel. Alternatively, incompletely distended bowel can mimic diseased bowel with apparent mural thickening, which will disappear when the bowel is adequately distended. In addition, well-distended bowel facilitates the depiction of an adjacent peritoneal, serosal, or omental tumor.
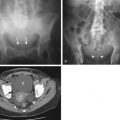
In my experience, a biphasic intraluminal contrast agent is optimal for GI tract imaging ( Fig. 6-1 ). Water is the classic biphasic MR intraluminal agent, showing high signal intensity on T2-weighted images and low signal intensity on T1-weighted images. On fat-suppressed, GE T1-weighted spoiled gradient-echo (SGE) images, the water-soluble contrast material is low in signal intensity. This allows one to depict the normal bowel wall as a thin, linear, mildly enhancing structure surrounding the dark bowel lumen. Water can be used as an oral contrast agent. However, because water is absorbed through the small intestinal wall, its use as an oral agent for MRI often results in unpredictable distention of the distal small bowel. For this reason, water-soluble contrast agents that are iso-osmolar are preferred because the ingested contrast will remain in the intestinal tract. In my practice, I have used different intraluminal agents for MRI. All the agents produce a biphasic appearance on MR images; they are readily available and relatively inexpensive. Other commercially available oral agents for MRI containing iron oxides and manganese have been described, but are not currently used in my practice.

Dilute Barium Sulfate
Barium sulfate solution (Readi-CAT 2, Bracco Diagnostics, Monroe Township, NJ) is composed of 98% water and 2% barium and other additives. On MR images, dilute barium sulfate has a biphasic appearance, with low signal on T1-weighted images and high signal on T2-weighted images. Readi-CAT 2 is commonly used for helical CT scans of the abdomen and pelvis. Dilute barium sulfate will remain within the intestines and is very effective in distending the small bowel and colon. Patients ingest 300 to 400 mL dilute barium, starting 1 hour before the MRI examination. Flavored versions of dilute barium sulfate (Readi-CAT 2 Smoothie, Bracco Diagnostics) are available and may be preferred by some patients.
Psyllium Fiber Mixed with Water
This is another water-soluble contrast agent that produces a biphasic appearance on T1-wieghted and T2-weighted images (see Fig. 6-1 ). Metamucil (Proctor & Gamble, Cincinnati) is composed of psyllium fiber with orange flavoring. It is a dietary fiber supplement that can be purchased over the counter. Its active ingredient is psyllium husk, a natural plant fiber with a high percentage of soluble fiber. Because Metamucil is orange-flavored, it is typically preferred by patients and better tolerated than dilute barium sulfate. A total dose of 0.8 mg/kg body weight Metamucil is mixed in 1 to 1.5 L of water. I mix a half-scoop of Metamucil per 8-ounce glass of water and have patients ingest four or five glasses over 1 hour prior to the examination. To improve filling of the distal small bowel, I have patients drink two of the glasses of Metamucil at home before leaving for their appointment. Unlike the Readi-CAT 2, some of the water in the Metamucil is absorbed in the small intestine and will be excreted via the kidney.
VoLumen
VoLumen (Bracco Diagnostics) is a low-density barium sulfate contrast agent especially designed for MDCT (multidetector computed tomography), positron emission tomography (PET), and CT examinations to mark the bowel as a negative intraluminal contrast agent. It is an ultra–low-dose barium sulfate agent with only 10% of the barium sulfate of conventional CT barium oral contrast agents. With VoLumen, 0.1% with barium is combined with 3% sorbitol, a nonabsorbable sugar alcohol that promotes luminal distention and limits the resorption of water across the length of the small bowel. VoLumen can be used for MRI of the GI tract, providing a biphasic appearance similar to that obtained with dilute barium sulfate. Theoretical advantages of VoLumen might include better bowel distention and more rapid bowel transit because of the sorbitol.
I am unaware of any direct comparisons. In my experience, the degree of bowel distention is related more to the volume and timing of the administration of the oral contrast material.
Mannitol 2.5% Mixed with 2% Locust Bean Gum
This has been proposed as an effective iso-osmolar, water-soluble oral agent for MRI. Mannitol is a white, crystalline, water-soluble, slightly sweet alcohol, C 6 H 8 (OH) 6 , used as a dietary supplement and dietetic sweetener. Mannitol comes in 500-mL bags mixed to a concentration of 20%. Mannitol 2.5% can be prepared by mixing 187.5 mL of 20% mannitol with enough tap water to achieve a volume of 1.5 L, and 3 g of locust bean gum (2%) is added to the mannitol solution to slow down the transit time through the intestinal tract. Locust bean gum, also called carob bean gum and Carubin, is extracted from the seed of the carob tree. It is used in ice cream, cultured dairy products, and cream cheese. The locust bean gum has been reported to decrease the diarrhea produced by orally ingested mannitol. The 1.5-L, 2.5% mannitol solution with locust bean gum is ingested over 1 hour prior to the MR examination. Sorbitol 2% can be used as an alternative to mannitol.
Rectal Water
This can be administered to distend the rectum and colon. I administer 500 to 1000 mL of tap water through a balloon-tipped barium enema catheter. Slow administration will help maximize the amount of fluid tolerated by the patient. The balloon at the tip of the catheter should be filled with water to avoid the susceptibility artifact caused by air in the balloon.
Routes of Contrast Administration
Intraluminal contrast material can be administered orally, with patients drinking 1 to 1.5 L of contrast material over 1 hour prior to the examination. Alternatively, contrast may be administered via a nasojejunal tube, as has been described for CT and MR enteroclysis. The enteroclysis technique has the advantage of more controlled and consistent small bowel distention but obviously requires nasojejunal intubation. Oral administration of intraluminal contrast material is effective in cooperative patients and can be combined with rectally administered water for simultaneous evaluation of the small bowel and colon.
Antiperistaltic Agents
Contrast-enhanced 3D GE images can be degraded by motion artifact related to bowel peristalsis. An antiperistaltic drug can markedly improve image quality. Glucagon, 1 mg, can be administered IV at the time of gadolinium injection. An alternative approach is to administer 0.25 mg hyoscyamine (Levsin) IV prior to the start of the examination. Levsin has a slower onset of action and longer duration compared with glucagon. In Europe, butylscopolamine (Buscopan) is commonly used to reduce bowel peristalsis. Users should consult the package insert to review contraindications prior to drug administration.
Clinical Applications
Inflammatory Bowel Disease
Crohn’s Disease
MRI provides many unique advantages when evaluating the mural changes of Crohn’s disease. Distending the bowel lumen with water-soluble contrast material allows one to depict the diseased bowel wall in the patient with active Crohn’s disease. On MR images, one may assess the thickness of the bowel wall, its degree and pattern of enhancement, and presence of adjacent mesenteric inflammation. MDCT is equally effective in assessing bowel wall thickening but is more limited in its assessment of mural enhancement. Compared with MDCT, the degree of bowel wall enhancement is much more conspicuous on GE MRI. This marked enhancement of inflamed bowel segments on 2D or 3D GE MR images facilitates the detection of subtle Crohn’s disease. A wall thickness greater than 3 mm is abnormal in a well-distended segment of bowel. Bowel wall thickening can be assessed on SS RARE images or fat-suppressed GE images.
Crohn’s Disease Activity.
Determining the activity of Crohn’s disease has important clinical implications that affect the selection of appropriate treatment options. Patients with recurrent abdominal pain because of active Crohn’s disease require treatment. However, patients commonly present with symptoms that may be unrelated to reactivation of their Crohn’s disease. This latter group of patients requires entirely different management. The activity of Crohn’s disease may be determined from clinical parameters, including the Crohn’s disease activity index, an assessment of acute-phase reactants (e.g., white blood cells [WBCs], erythrocyte sedimentation rate, C-reactive protein, orosomucoids), or clinical symptoms and physical findings. In practice, these clinical parameters may be misleading or inconclusive. The results of endoscopy and imaging studies can play an important role in determining the activity and extent of Crohn’s disease.
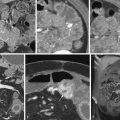
The activity of Crohn’s disease can be assessed by a number of different MRI parameters, including degree of bowel wall enhancement, pattern of enhancement, thickness and length of the involved diseased segment, and presence of edema in the bowel wall on T2-weighted images. Restricted diffusion within the diseased segments of bowel also indicates active inflammation. Perienteric changes, including enhancing lymph nodes, infiltration of mesenteric fat, and increased mesenteric vascularity, can also reflect active Crohn’s disease.
Degree of Bowel Wall Enhancement.
The degree of mural enhancement with IV gadolinium correlates with the activity of Crohn’s disease. Enhancement of the thickened bowel wall can be assessed on the first set of GE images by comparing the bowel wall enhancement to the liver and intravascular gadolinium. The normal bowel wall enhances less than the liver parenchyma. Mural enhancement of thickened bowel greater than that of the liver is abnormal, and mural enhancement equal to that of intravascular gadolinium is markedly abnormal. In chronic inactive Crohn’s disease, the thickened bowel wall will show no enhancement or only mild enhancement ( Fig. 6-2 ). Chronic fibrotic strictures will show a thickened bowel wall with minimal enhancement. Active Crohn’s disease shows moderate to marked bowel wall enhancement ( Fig. 6-3 ). In patients with a layered pattern of enhancement (see later), the enhancing mucosa should show moderate to marked enhancement.