The long bones of the upper extremity are often overlooked in favor of addressing their intervening joints. However, there are a wide variety of pathologic processes that can involve these anatomic segments. To better understand the complex anatomy of the upper extremity, this article is divided into sections describing the osseous, muscular, and neurovascular anatomy of the arm and forearm using a compartmental approach. The discussion touches on a few common normal variants and their potential functional consequences. The upper extremity joints of the shoulder, elbow, and wrist are addressed separately.
The long bones of the upper extremity are often overlooked in favor of addressing their intervening joints. However, there are a wide variety of pathologic processes that can involve these anatomic segments. To better understand the complex anatomy of the upper extremity, the following discussion is divided into sections describing the osseous, muscular, and neurovascular anatomy of the arm and forearm using a compartmental approach. The discussion touches on a few common normal variants and their potential functional consequences. The upper extremity joints of the shoulder, elbow, and wrist are addressed separately.
Imaging
Applications of MR imaging of the musculoskeletal system have expanded enormously from the initial narrow indications of infection and tumor evaluation. Examinations are now routinely performed for the assessment of sports-related or other injury. Most musculoskeletal examinations at our institution are performed on a standard 1.5-Tesla scanner; however, higher-field (3.0T) imaging offers many potential advantages. The potential advantages include increased signal-to-noise ratio (SNR) and decreased imaging time. Higher field imaging shortens the time required for chemical fat saturation sequences but this advantage is offset by the higher field inhomogeneity that degrades chemically selected fat-saturation sequences. Various parameters need to be adjusted to optimize 3T imaging. Because T1 relaxation time is increased, TR needs to be increased to maintain contrast. Additionally, the decreased T2 relaxation time needs to be compensated by decreasing the TE. The TI for short tau inversion recovery (STIR) imaging also needs to be increased for 3T imaging.
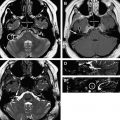
The images presented in this article were obtained of a 30-year-old asymptomatic healthy male volunteer on a 3T Verio Scanner (Siemens Medical, Erlangen, Germany). The pulse sequences obtained on the 3T are similar to those obtained with lower field strength. The examinations are obtained using a 6-channel standard body surface coil with the patient in anatomic position. T2 HASTE sequences are obtained in 3 orthogonal planes to act as a localizer. T1 fast spin-echo (FSE) images are obtained in all 3 orthogonal planes. Fluid-sensitive STIR images are obtained in the coronal and sagittal planes and intermediate TE T2 FSE fat-saturated images were obtained for the smaller field of view axial images. When indicated, contrast (Magnevist, gadopentetate dimeglumine, Bayer Schering Pharma AG, Berlin, Germany) is administered intravenously at a dose of 0.1 mmol/kg and saturated T1 FSE images are also obtained in the 3 orthogonal planes. Patients with compromised renal function (stage 4 or 5 renal failure) are informed of the risk of nephrogenic systemic fibrosis and consented before contrast administration if the examination is deemed clinically necessary and of favorable risk-benefit ratio. A complete examination of the arm or the forearm takes approximately 28 minutes to complete with contrasted sequences requiring another 12 minutes.
Advantages of sequences
MR can detect marrow abnormalities earlier than competing modalities including computed tomography (CT) and bone scan. STIR images are particularly useful for depiction of marrow pathology. Intermediate TE T2 FSE fat-saturated images offer better anatomic detail and similar sensitivity for fluid signal abnormalities when compared with STIR. However, T2 FSE images suffer from inhomogeneous fat suppression with larger fields of view, a problem that is compounded at higher field strength. T1 FSE images are useful in delineating muscles and other structures by their separating fat planes and are therefore the predominate sequence used in this pictorial essay. Post contrast images are useful in differentiating solid and cystic lesions and increase the sensitivity for abscess detection.
Advantages of sequences
MR can detect marrow abnormalities earlier than competing modalities including computed tomography (CT) and bone scan. STIR images are particularly useful for depiction of marrow pathology. Intermediate TE T2 FSE fat-saturated images offer better anatomic detail and similar sensitivity for fluid signal abnormalities when compared with STIR. However, T2 FSE images suffer from inhomogeneous fat suppression with larger fields of view, a problem that is compounded at higher field strength. T1 FSE images are useful in delineating muscles and other structures by their separating fat planes and are therefore the predominate sequence used in this pictorial essay. Post contrast images are useful in differentiating solid and cystic lesions and increase the sensitivity for abscess detection.
Normal MR signal
Bone marrow signal is variable among patients depending on age and hematopoietic stressors. Bone marrow is referred to as red or yellow according to its relative hematopoietic content. Red marrow is composed of 60% hematopoietic cells, whereas yellow marrow is almost entirely adiopocytic. Bone marrow converts to its mature distribution in an orderly and predictable manner. The epiphyses followed by the diaphyses and then the metaphyses convert from red to yellow marrow. The conversion of the appendicular skeleton to yellow marrow should be complete within the third decade of life. Marrow can reconvert at times of stress with re-conversion proceeding in the reverse order of the initial conversion. On MR imaging, the signal characteristics of yellow marrow are similar to those of fat. Red marrow demonstrates intermediate signal on both T1-weighted and T2-weighted sequences secondary to its lesser fat content and T1 shortening.
Tendons and ligaments are normally of homogeneously low signal on all pulse sequences. Some of the larger tendons, including the triceps, can normally demonstrate internal high signal striations.
Nerves in the arm and forearm demonstrate similar signal characteristics to other peripheral nerves. Nerves are normally intermediate in signal on both T1-weighted and T2-weighted images, similar to that of adjacent muscle. Nerves are made more conspicuous by peri-neural fat. Routine axial images with the elbow in full extension should allow consistent visualization of the major nerves. Specialized axial views with the elbow in flexion for ulnar nerve or pronation for the median and radial nerves may be helpful for further characterization or to assess for impingement.
Vessels have a variable appearance depending on their internal flow. High-flow vessels normally demonstrate signal voids, whereas smaller low-flow vessels demonstrate increased signal on T2-weighted images.
Normal anatomy
The upper limb consists of 4 segments, which are from proximal to distal: the pectoral girdle, the arm, the forearm, and the hand. These segments are separated by the joints of the shoulder, elbow, and wrist, respectively. In this article, we address the normal MR appearance of the arm and the forearm with the intervening joints being addressed separately.
Osseous anatomy
The humerus ( Fig. 1 ) is the largest bone of the upper limb. The proximal spherical humeral head articulates with the glenoid to form the scapulohumeral (shoulder joint). The anatomic neck of the humerus circumscribes the head and separates it from the tuberosities. The lesser and greater tuberosities project off the anterior and lateral aspects of the proximal humerus respectively and form the intervening intertubercular (bicipital) groove. The narrowing of the humerus just distal to the tubercles is referred to as the surgical neck, a common site of humeral fracture. The body of the humerus has 2 prominent features: the deltoid tuberosity and the radial groove. The deltoid tuberosity, located laterally, is the insertion site of the deltoid muscle. The radial groove, located posteriorly, accommodates the radial nerve and the deep brachial artery as they course between the medial and lateral heads of the triceps muscle. The distal humerus flares out forming the supracondylar ridges, which end distally as the epicondyles, the medial of which is more prominent. The distal end of the humerus, including the epicondyles and articular surfaces of the trochlea and the capitellum, is referred to as the condyle of the humerus. The lateral capitellum articulates with the radial head. The capitellum resembles a sphere with a distinct contour change where the anterior capitellum intersects the posterior lateral epicondyle. This normal appearance has been termed the “pseudodefect of the capitellum,” which may be confused for an osteochondral lesion ( Fig. 2 ). Superior to the capitellum anteriorly is the radial fossa, which accommodates the radial head in full flexion. The medial trochlea articulates with the trochlear notch of the proximal ulna. Superior to the trochlea anteriorly is the coronoid fossa, which accommodates the coronoid process of the ulna in full flexion. Posteriorly, the more prominent olecranon fossa accommodates the olecranon in full extension.
There is an osseous excrescence off the anterior humerus that can be seen as a normal variant. This is referred to as the “supracondylar process,” found approximately 7 cm proximal to the medial epicondyle in 0.3% to 2.7% of asymptomatic human subjects. The ligament of Struthers, a fibrous band passing from the supracondylar process to the medial epicondyle creates a fibro-osseous tunnel through which the brachial artery and median nerve pass. Compression of the median nerve at this location can cause numbness of the hand and weakness of the muscles of the anterior compartment of the forearm.
The ulna is the medial and longer of the 2 forearm bones. The proximal ulna has 2 prominent projections, the olecranon and the coronoid process coming off the posterior and anterior aspects of the proximal ulna, respectively, and forming the trochlear groove. Lateral to the coronoid process is the radial groove, which forms the articulation with the radial head. Inferior to the radial groove is the supinator groove and crest, the attachment site of the supinator muscle. The body of the ulna is thick and cylindrical and tapers distally. At its end it abruptly enlarges forming the discoid head with the styloid process medially. Ulnar variance denotes the length of the ulna relative to the adjacent radius. Negative ulnar variance indicates that the ulna is shorter than the radius and, conversely, positive ulnar variance indicates that it is longer. Typically, a 3-mm difference is required to denote significant ulnar variance.
The radius is the lateral and shorter of the 2 forearm bones. The proximal discoid radial head articulates with the capitellum and the radial notch of the ulna. The radial tuberosity serves as the insertion of the biceps muscle and separates the proximal head and neck from the distal body. The body of the radius has a lateral convexity and enlarges in width distally. The distal end of the radius is rectangular when viewed in axial sections. At its distal medial aspect, it forms the concave ulnar notch, which accommodates the head of the ulna. At its distal lateral aspect, it forms the radial styloid process, which is larger and distal to its ulnar counterpart. The dorsal tubercle (Lister tubercle) projects posteriorly forming grooves for the posterior compartment muscles ( Fig. 3 ).
Muscle anatomy, arm
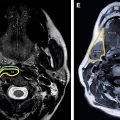
The arm can be divided into anterior and posterior compartments. The anterior compartment contains the flexors (biceps brachii, brachialis, and coracobrachialis) and is supplied by the musculocutaneous nerve ( Figs. 4–6 ). The posterior compartment contains the extensor triceps brachii and the lateral anconeus and is supplied by the radial nerve.
Anterior Compartment
The short and long heads of the biceps originate on the coracoid and supraglenoid tubercle respectively. The long head passes though the bicipital groove under the transverse humeral ligament. The biceps muscle bellies unite approximately 7 cm proximal to the elbow and insert on the radial tuberosity. The distal biceps tendon has no tendon sheath, like that of the Achilles tendon. There is a relatively hypovascular zone of the distal biceps tendon, which may subject to degeneration and tearing secondary to mechanical impingement between the radial tuberosity and the ulna. The biceps muscle serves as both a flexor and supinator of the forearm. Approximately 10% of the population has a third head of the biceps originating from the superomedial portion of the brachialis. This normal variant is of uncertain functional or clinical significance.
The brachialis is the main flexor of the forearm. It lies deep to the biceps originating from the distal half of the anterior humerus and inserting on the tuberosity of the ulna.
The coracobrachialis helps to flex and abduct the arm and stabilize the glenoid joint. The elongated muscle is located at the superomedial aspect of the arm originating from the coracoid tip and inserting on the mid medial humerus.
Posterior Compartment
The triceps is the main extensor of the elbow joint and has 3 heads. The long, lateral, and medial heads originate from the infraglenoid tubercle, superior posterior surface of the humerus, and inferior posterior surface of the humerus respectively. They insert as a common tendon on the proximal olecranon. This common tendon may normally have a striated appearance. Rarely, the medial triceps may insert on the medial epicondyle, potentially causing ulnar nerve compression.
The anconeus is a diminutive relatively unimportant muscle at the posterolateral aspect of the distal humerus. It originates from the posterior aspect of the lateral epicondyle and courses medially, inserting on the lateral olecranon. The anconeus is thought to help with extension and resist elbow abduction. The anconeus also serves as a landmark for the lateral aspect of the elbow.
The anconeus epitrochearis (accessory anconeus) is an anomalous accessory muscle, which arises from the medial humeral condyle, passes superficial to the ulnar nerve and inserts on the olecranon. This variant may occur in up to 11% of the population and is one of the potential causes of cubital tunnel syndrome owing to ulnar nerve compression. The small muscle is not palpable and requires imaging for its depiction. During elbow flexion, it can impinge on the underlying nerve and cause compression. Excision without anterior transposition of the ulnar nerve is the treatment in symptomatic patients.
Muscle anatomy, forearm
The forearm is separated into 2 compartments by the interosseous membrane ( Figs. 7–9 , Tables 1 and 2 ). The anteromedial (“anterior”) compartment contains the flexor-pronators and is supplied predominately by the median nerve (with the ulnar nerve supplying the remaining one and a half muscles as detailed later in this article). The deep muscles of the anterior compartment are supplied by a median nerve branch, the anterior interosseous nerve. The posterolateral (“posterior”) compartment contains the extensor-supinators and is supplied by the radial nerve and its branches.