Traditionally, many diffuse diseases of the liver could only be diagnosed by liver biopsy. Although still considered the gold standard, liver biopsy is limited by its small sample size, invasive nature, and subjectivity of interpretation. There have been significant advances in functional magnetic resonance (MR) imaging of the liver. These advances now provide radiologists with the tools to evaluate the liver at the molecular level, allowing quantification of hepatic fat and iron, and enabling the identification of liver fibrosis at its earliest stages. These methods provide objective measures of diffuse liver processes and aid hepatologists in the diagnosis and management of liver disease.
Key points
- •
Liver biopsy is considered the gold standard for quantifying hepatic fat content, hepatic iron content, and degree of hepatic fibrosis; however, it is limited by small sample size, risk of complication, subjectivity in interpretation, and poor patient acceptance.
- •
Hepatic fat quantification can be determined by multiple MR imaging methods. MR spectroscopy is considered the most accurate but other methods are used more commonly because of their ease of use.
- •
There are two general strategies for determining liver iron content by MR imaging: signal intensity ratio and relaxometry.
- •
MR elastography is an emerging technique that uses a shear wave to determine the stiffness of the liver parenchyma and quantify fibrosis.
Over the past decade, there have been numerous advances in MR imaging techniques used to image the liver. In the past, MR imaging assessment of the liver relied primarily on noncontrast T1- and T2-weighted images along with dynamic postcontrast sequences to characterize the liver parenchyma and underlying lesions. Although these sequences can offer the radiologist a morphologic assessment of the liver, they are not able to provide the functional data required to diagnose and manage diffuse hepatic disease as they present in their earliest, and potentially reversible, stages. This article provides an overview of modern pediatric liver imaging techniques, including methods used for hepatic fat quantification, hepatic iron quantification, and detection of hepatic fibrosis.
Patient preparation and imaging
There are several unique considerations when preparing to image pediatric patients. The first step of any pediatric imaging procedure is describing what will happen in an age-appropriate manner to the patient and his or her family. Child life specialists can be instrumental in this task, explaining the procedure through play or demonstration. MR imaging is an ideal procedure for demonstration because the long scan times, relatively small scanner bore, and loud noises make it a difficult study for children to undergo without preparation. Mock scanners (scale or full-size models of the clinical scanners) have been used to prepare children for the experience of undergoing MR imaging.
Simulation is another method used to prepare older children for an examination and is a key component of preparing patients for MR elastography (MRE). Before the examination, child life specialists show and allow the child to touch the passive driver, explain what the child will feel during scanning, and then place the vibrating passive driver on the child. The prescan simulation helps prepare patients for the sensation they will feel during scanning and helps to reduce patient anxiety and sudden movements at the start of the actual MRE sequence.
Immobilization is important to obtain high-quality imaging. There are several techniques used to help children remain still. At the authors’ institution, general anesthesia is used for most children younger than 3 years of age, whereas conscious sedation is used for most children between the ages of 3 and 6. In these young patients, conscious sedation or anesthesia helps to ensure cooperation and allows for controlled breathing while at the same time minimizing fear and anxiety. Distraction is the primary technique used to help older children and adolescents remain still during imaging. Video goggles allow patients to watch a television show or movie of their choice while they are being imaged. Music can be listened to in lieu of video if the patient prefers.
Obtaining intravenous access can be difficult in children. Fortunately, the standard protocol for many of the functional imaging techniques of the liver does not require intravenous access. Typically, adult hepatobiliary imaging is performed after an overnight fast. In children who are not sedated, the authors ask that they take nothing by mouth for at least 4 hours before imaging. This helps to minimize artifacts from bowel peristalsis and ensures a full gallbladder.
During MR imaging, there are several factors that are modified for pediatric patients. The specific absorption rate is automatically maintained within acceptable limits by the scanner based on the patient’s weight. In addition, the scan field of view is set to a value depending on the size of the patient. Coils are also selected based on the size of the patient and the scanner. For most children, a cardiac coil is used for abdominal imaging. For larger patients, a torso coil can be used.
Patient preparation and imaging
There are several unique considerations when preparing to image pediatric patients. The first step of any pediatric imaging procedure is describing what will happen in an age-appropriate manner to the patient and his or her family. Child life specialists can be instrumental in this task, explaining the procedure through play or demonstration. MR imaging is an ideal procedure for demonstration because the long scan times, relatively small scanner bore, and loud noises make it a difficult study for children to undergo without preparation. Mock scanners (scale or full-size models of the clinical scanners) have been used to prepare children for the experience of undergoing MR imaging.
Simulation is another method used to prepare older children for an examination and is a key component of preparing patients for MR elastography (MRE). Before the examination, child life specialists show and allow the child to touch the passive driver, explain what the child will feel during scanning, and then place the vibrating passive driver on the child. The prescan simulation helps prepare patients for the sensation they will feel during scanning and helps to reduce patient anxiety and sudden movements at the start of the actual MRE sequence.
Immobilization is important to obtain high-quality imaging. There are several techniques used to help children remain still. At the authors’ institution, general anesthesia is used for most children younger than 3 years of age, whereas conscious sedation is used for most children between the ages of 3 and 6. In these young patients, conscious sedation or anesthesia helps to ensure cooperation and allows for controlled breathing while at the same time minimizing fear and anxiety. Distraction is the primary technique used to help older children and adolescents remain still during imaging. Video goggles allow patients to watch a television show or movie of their choice while they are being imaged. Music can be listened to in lieu of video if the patient prefers.
Obtaining intravenous access can be difficult in children. Fortunately, the standard protocol for many of the functional imaging techniques of the liver does not require intravenous access. Typically, adult hepatobiliary imaging is performed after an overnight fast. In children who are not sedated, the authors ask that they take nothing by mouth for at least 4 hours before imaging. This helps to minimize artifacts from bowel peristalsis and ensures a full gallbladder.
During MR imaging, there are several factors that are modified for pediatric patients. The specific absorption rate is automatically maintained within acceptable limits by the scanner based on the patient’s weight. In addition, the scan field of view is set to a value depending on the size of the patient. Coils are also selected based on the size of the patient and the scanner. For most children, a cardiac coil is used for abdominal imaging. For larger patients, a torso coil can be used.
Hepatic fat quantification
Hepatic fat quantification is most commonly used in the setting of nonalcoholic fatty liver disease (NAFLD). NAFLD is the most common cause of chronic liver disease in children, occurring with a prevalence of 8% to 9.6% of the general pediatric population. It is more common in older children; obese children; males; and children of Hispanic, Asian, or caucasian descent. Children typically present with protean symptoms including vague abdominal pain, irritability, fatigue, headache, and difficulty concentrating. On physical examination, many patients are obese and may also have hypertension, hepatomegaly, and acanthosis nigricans. Laboratory-based biomarkers of NAFLD include insulin sensitivity and elevated serum leptin. In addition to these biomarkers liver enzymes may be elevated.
Pathologically, NAFLD is a general term encompassing a broad spectrum of disease ranging from steatosis, to steatohepatitis, fibrosis, and cirrhosis. Traditionally, NAFLD has been diagnosed by liver biopsy. Although biopsy is able to distinguish NAFLD from nonalcoholic steatohepatitis and other causes of fatty liver infiltration, it is an invasive procedure with inherent risks and potential complications. The rate of complications can vary depending on the operator and the type of biopsy procedure. Prior studies have shown that 1% to 3% of patients undergoing liver biopsy require subsequent hospitalization. Other limitations of liver biopsy include its potential for sampling error, subjective interpretation/grading systems, and high amount of interobserver variation. Ultimately, the limitations of liver biopsy along with its poor patient acceptance make it suboptimal for serial assessment of liver disease.
MR imaging–based hepatic fat quantification offers several advantages over biopsy and pathologic assessment. These advantages include its reproducibility, low degree of variability in interpretation, the ability to perform quantitative and qualitative assessment of hepatic fat, and its ability to assess the entire liver. Perhaps the greatest advantage of imaging-based hepatic fat quantification is its noninvasive nature ( Box 1 ).
- •
Noninvasive
- •
Reproducible
- •
Objective measure
- •
Low degree of variability
- •
Ability to assess entire liver
- •
Ability to evaluate extrahepatic complications
Technique
MR imaging fat quantification can be performed using either MR spectroscopy or chemical shift imaging. MR spectroscopy is generally considered the gold standard for in vivo fat quantification because it is the most direct MR imaging method to separate liver signal into its water and fat components. MR spectroscopy has several advantages when compared with chemical shift imaging. First, it has a wide dynamic range allowing for quantification of any range of fat (0%–100%). Because MR spectroscopy is very sensitive, it is able to detect subtle changes in hepatic triglyceride content during treatment. The high sensitivity does not come at the cost of specificity. MR spectroscopy, unlike chemical shift imaging, is not susceptible to confounding effects from fibrosis, iron overload, or glycogen. Finally, MR spectroscopy is the only noninvasive method that is able to detect a necroinflammatory response.
Even though there are many advantages of MR spectroscopy, it is not widely used in clinical practice. Spectral analysis methods are complex and require commercial postprocessing software to analyze the raw data. This complexity can lead to variability in the results. In addition, the results can also vary depending on the MR imaging scanner, acquisition parameters, and method of analysis. This potential lack of reproducibility makes it difficult for hospitals with multiple MR imaging scanners, possibly from different manufacturers, to reliably track hepatic fat content over time.
Because of its ease of performance and rapid acquisition, chemical shift imaging has become the preferred method of performing hepatic fat quantification. There are several methods that can be used to perform chemical shift imaging, although each method relies on the difference between the precession frequencies of fat and water protons to quantify hepatic fat content. The frequency difference causes tissue voxels containing fat and water to lose signal in out-of-phase imaging. This signal loss can be compared with in-phase imaging, and the difference in signal is used to quantify the fat content.
The use of spin echo sequences for chemical shift imaging was first described in 1984. In this technique, termed the Dixon method, a modified dual echo spin echo sequence was designed such that the first echo image is acquired when water and fat are in-phase with each other and the next echo image is acquired with water and fat in opposed-phase. For a voxel containing only water or fat, its net signal is the same on in-phase and opposed-phase acquisitions, because one component’s signal is zero. In contrast, a voxel containing water and fat has different signals from the two acquisitions. Using this information, the in-phase and opposed-phase images are then added or subtracted to generate a water-only image and a fat-only image. A quantitative fat-fraction value can be calculated from the generated water-only and fat-only images by taking a ratio of fat versus water and fat.
This approach, termed the two-point Dixon method, is limited by its long acquisition times and sensitivity to magnetic field inhomogeneity. To overcome the sensitivity to magnetic field inhomogeneity, a three-point Dixon method was developed, adding a third echo series of images to correct for the phase shifts that occurred between echoes. Although this technique allowed the images to be corrected for field inhomogeneity, scan acquisition times remained long. The introduction of fast gradient echo sequences led to a modified Dixon technique. This method significantly reduces scan time to the point where both phases can be performed in a single breathhold.
The modified Dixon technique using gradient recalled echo (GRE) images is widely used because of its simplicity; however, it has several limitations. The dynamic range for the detection of fat is somewhat limited, ranging between 10% and 50%. In addition, in patients with increased liver iron content (cirrhosis, hemochromatosis), the increased iron has a paramagnetic effect causing local field inhomogeneity and signal loss from T2* relaxation. It is thus essential to make every effort to keep the TEs as short as possible to minimize the effects of T2* signal loss.
Complex chemical shift-based approaches, such as the iterative decomposition of water and fat with echo asymmetry and least-squares estimation technique, collect three images to separate fat and water signal. Iterative decomposition of water and fat with echo asymmetry and least-squares estimation provides uniform and reliable fat suppression with rapid image acquisition times. The addition of the third sequence helps account for field inhomogeneity and extends the range of fat quantification to 0% to 100%.
Proton density fat fractionation has been developed to address the confounding factors that introduce error into fat quantification seen with other traditional techniques. This method of hepatic fat quantification can be used on any MR imaging scanner, regardless of the vendor, and uses a spoiled gradient recalled echo sequence with the flip angle optimized to minimize T1 effects and multiple echoes to minimize T2* effects ( Fig. 1 ). With this technique, fat content can be measured throughout the entire dynamic range, 0% to 100% using the equation η = (100% * [SI In-phase – SI Opposed-phase ]/[2* SI In-phase ]) where η is the fat fraction, SI In-phase is the signal intensity of a region of interest from the liver on the in-phase images, and SI Opposed-phase is the signal intensity of a region of interest from the liver on the opposed-phase images. A recent study has shown that proton density fat fractionation significantly correlates with histologic steatosis grades. For these reasons, the authors have decided to use proton density fat fractionation at their institution. An example protocol for pediatric fat fractionation is included in Table 1 ( Box 2 ).
| Sequence | Plane | Approximate Scan Time (s) | TR (ms) | TE (ms) | Slice Thickness (mm) | Matrix Size |
|---|---|---|---|---|---|---|
| Opposed-phase | Axial | 20 (total for both sequences) | 7 | 2.2 | 3 | 320 × 192 |
| In-phase | Axial | 20 (total for both sequences) | 7 | 4.4 | 3 | 320 × 192 |
- •
Hepatic fat quantification is most commonly used for patients with NAFLD.
- •
MR spectroscopy is considered the imaging gold standard; however, it is a complex method and requires postprocessing software, limiting its general applicability.
- •
Because of its simplicity, chemical shift imaging has become the preferred method of performing hepatic fat quantification.
- •
There are multiple methods to determine the fat fraction using chemical shift imaging.
Hepatic iron quantification
Hepatic iron overload is the abnormal and excessive intracellular accumulation of iron in liver cells. Normally, excess iron is stored bound to the intracellular protein, ferritin. Increased and sustained systemic iron overwhelms the capacity of ferritin to collect and store iron, leading to accumulation of unbound iron in the cytoplasm of cells primarily in the liver, pancreas, spleen, and bone marrow. This is problematic, because free intracellular iron can react with hydrogen and lipid-generating free radicals that cause cellular damage. In the liver, this damage can lead to fibrosis and cirrhosis.
There are two basic mechanisms for iron overload: excess intestinal absorption or repeated blood transfusions. Hereditary (primary) hemochromatosis is the characteristic disorder of iron overload caused by excess intestinal absorption. It is more common in whites and most prevalent in Ireland, where it affects up to 1 in 150 to 250 people. Affected individuals are typically asymptomatic, particularly in early stages of the disease. If symptoms are present, they are vague and nonspecific and include weakness, lethargy, impotence, and arthralgias. The disease is more commonly symptomatic in males, because females are protected by blood loss during menstruation. Patients typically present later in life, although presentation in infancy and childhood does occur. In patients with hereditary hemochromatosis, iron deposition first occurs in the liver, heart, and pancreas.
Patients with syndromes that require repeated blood transfusions, such as thalassemia, are at risk to develop secondary hemochromatosis. Thalassemias are a group of hereditary blood disorders caused by a defect in the genes that produce globin leading to impaired erythropoiesis. Patients with β-thalassemia major are among the most severely affected. They present around 6 months of age with a severe microcytic hypochromatic anemia, irritability, poor growth, jaundice, hepatosplenomegaly, and high-output cardiac failure. These patients are treated with repeated blood transfusions; however, the transfusional iron overload is exacerbated by increased intestinal iron absorption caused by tissue hypoxia, apoptosis of defective precursors of erythropoiesis, and hemolysis of native and transfused red blood cells. Because of these factors, the iron overload can become severe in infancy or early childhood and lead to endocrine and cardiac dysfunction unless iron chelation therapy is provided. As with other patients with secondary hemochromatosis, iron accumulates in the reticuloendothelial cells of the liver, spleen, bone marrow, and lymph nodes. Once the reticuloendothelial system is saturated, the iron begins to deposit in the hepatocytes themselves, and within the pancreas, myocardium, and endocrine glands.
Technique
Liver iron quantification is an important technique used to help diagnose and manage patients with primary and secondary hemochromatosis. Although liver biopsy is the current gold standard for iron quantification, it shares the same limitations as liver biopsy for fat quantification and is not suitable for repeated measurements over time. Because of the limitations of biopsy, MR imaging has become the preferred method of determining liver iron content.
There are two main methods for determining liver iron content: signal intensity ratio and relaxometry. The signal intensity ratio method compares the signal intensity of the liver on spin echo or gradient echo sequences with the signal intensity of a reference tissue that does not concentrate iron, such as skeletal muscle. The most widely used method to determine the liver iron content by signal intensity ratio was developed by Gandon and colleagues. In this method, five breathhold gradient echo sequences are obtained while the TE and flip angle are varied. On each series, the mean liver signal is obtained by drawing three regions of interest in the right lobe of the liver. The mean liver signal is compared with the mean muscle signal obtained by drawing a region of interest on the right and left paraspinal muscles. The mean liver signal intensity is then divided by the mean muscle signal intensity to give the liver/muscle ratio. Gandon and colleagues have developed an online calculator to help estimate the liver iron content using the signal intensity values obtained from each region of interest on each sequence.
Gandon’s method is in use throughout the world because of its simplicity, accuracy, and ability to be performed on any scanner. However, there are limitations with this method. Perhaps the greatest limitation is that all of the sequences used to determine the liver iron content eventually saturate with very high iron content. The maximum value that can be obtained using this method is 350 μmol/g. Values above this level are reported as greater than 350 μmol/g. Another limitation is that biologic factors, such as steatosis or fatty infiltration of muscle, can change the mean signal intensity of liver and muscle. This is partially accounted for by fat saturation; however, fat saturation is often not homogeneous. Finally, the technique requires several breathholds, which makes it difficult for younger children to complete.
Relaxometry methods for the assessment of liver iron content rely on decreases in the T2 relaxation times because of the paramagnetic properties of the iron in the liver. In this approach, a series of spin echo or gradient echo images are obtained with increasing TE values. The signal intensity of the liver is then modeled across multiple TE values. Depending on whether spin echo or gradient echo images are used, the signal decay constants T2 or T2* are calculated, respectively. Recent reports have favored using the reciprocal values of T2 or T2*, defined as R2 or R2*. R2 or R2* values are preferred because they directly correlate with iron content; the larger the R2 or R2* value, the higher the iron content.
R2 and R2* are not equivalent; each variable has theoretical advantages and disadvantages. R2 measurements are less sensitive to confounding factors, such as scanner, voxel size, magnetic inhomogeneities, and artifacts. R2* measurements are more sensitive to detect low levels of iron content but they can become inaccurate in the setting of iron overload. In addition, R2* measurements are less sensitive to variation in the size and distribution of iron particles and the complications of liver disease. Perhaps the biggest advantage of using R2* is the significantly shorter acquisition time; R2* images can be performed in a single breathhold, whereas R2 measurements must be acquired over 2 to 20 minutes.
To address the complexity of performing and interpreting the data obtained in the relaxometry method, several commercial ventures have been created. FerriScan (Resonance Health, Claremont, Australia) is a US Food and Drug Administration–approved method used to measure liver iron content. This technique uses the St. Pierre method consisting of seven free-breathing spin echo sequences with increasing TE values to determine the iron content. A phantom with a long T2 value is placed in the field of view to help standardize values across sequences. Although this method is accurate and reproducible, it has several limitations, including a high cost; centralized image analysis; long image acquisition time (20 minutes); and 24–48 hours turnaround time for data analysis. Additionally, the method is insensitive to longitudinal changes in liver iron content in patients with severe iron overload.
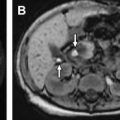
At the authors’ institution, we use two different relaxometry methods to measure liver iron content: the R2* method and St. Pierre method ( Fig. 2 ). The technique used for R2* relaxometry and the St. Pierre method are included in Table 2 . The most common indication for iron quantification in the authors’ institution is transfusional overload. Because of this, they often perform cardiac MR imaging and cardiac iron quantification in the same setting as they perform hepatic iron quantification ( Box 3 ).