Magnetic resonance (MR) imaging is a modality widely used to assess shoulder abnormalities in children. A thorough understanding of the development of the shoulder and adequate MR techniques are crucial in the radiologic evaluation. The immature skeleton is particularly vulnerable to insults such as trauma, infection, and inflammation, and responds in unique ways. The pediatric shoulder can also be affected by complex congenital deformities such as brachial plexus injuries. In addition, certain neoplasms can be seen specifically in the young patient. MR imaging plays a critical role in the initial diagnostic evaluation and in assessing posttreatment responses.
The pediatric shoulder
Growth and development of the shoulder is complex. Appropriate interpretation of magnetic resonance (MR) images of the shoulder in children requires an understanding of normal skeletal maturation and how it results in different patterns of injury. The ability of MR imaging to depict cartilage, marrow, and soft tissues without using ionizing radiation makes it extremely useful in children. This article describes the MR appearance of normal developmental changes, common injuries, and unique conditions that affect the shoulder throughout childhood.
General developmental principles
The development of the shoulder starts during the fourth week of embryonic life. At this time, mesenchymal cells derived from somatic mesoderm condense and form the upper limb bud. These cells will eventually give origin to bone, cartilage, and other soft tissues of the upper extremity. By the eighth week of gestation, all structural components of the shoulder girdle are present. Ossification of the diaphysis of the humerus starts between the seventh and ninth weeks of gestation, and is followed by the formation of the scapula and midportion of the clavicle. Vascular invasion of the humeral cartilaginous epiphysis, development of the marrow cavity, and somatic growth will continue to shape the shoulder throughout the remainder of fetal life.
At birth, the proximal humeral epiphysis, acromion, coracoid, and lateral epiphysis of the clavicle are composed of hyaline cartilage, whereas the humeral diaphysis, midportion of the clavicle, and body of the scapula are ossified. The primary physes of the clavicle and humerus are responsible for the longitudinal growth of these bones. The proximal physis of the humerus is responsible for approximately 80% of its overall elongation, whereas the lateral physis of the clavicle contributes little to the final length of the bone. Appositional growth of the diaphysis and metaphysis of the humerus and clavicle, and body of the scapula occurs by intramembranous ossification that originates from the periosteum and perichondrium.
Throughout childhood, the cartilaginous epiphyses and apophyses of the shoulder develop secondary ossification centers. These centers enlarge by endochondral ossification from a secondary physis. The age at which each epiphysis or apophysis begins to ossify and grow varies between sites, which in turn results in the changing appearance of the shoulder at different stages of skeletal maturation. The subchondral marrow of a developing ossification center and its adjacent secondary physis is similar in architecture, composition, and MR imaging characteristics to the metaphysis and primary physis of long bones. By the time skeletal maturity is reached, all epiphyseal cartilage has been replaced by mineralized bone, with the exception of articular cartilage.
The growth of bones results in increased tension on the soft tissues of the shoulder girdle. The muscles, ligaments, tendons, and joint capsule, including the labroligamentous complex, grow in response to the traction exerted on them by the growing skeleton. The signal intensity (SI) on MR images of the subcutaneous tissues also changes during growth. In neonates and infants, there are prominent deposits of brown fat in the axillary, subscapular, and parascapular regions. These normal deposits of brown fat show a slightly heterogeneous SI on T1-weighted images and may demonstrate patchy enhancement after the administration of intravenous contrast ( Fig. 1 ), which can be a source of unnecessary concern.
General developmental principles
The development of the shoulder starts during the fourth week of embryonic life. At this time, mesenchymal cells derived from somatic mesoderm condense and form the upper limb bud. These cells will eventually give origin to bone, cartilage, and other soft tissues of the upper extremity. By the eighth week of gestation, all structural components of the shoulder girdle are present. Ossification of the diaphysis of the humerus starts between the seventh and ninth weeks of gestation, and is followed by the formation of the scapula and midportion of the clavicle. Vascular invasion of the humeral cartilaginous epiphysis, development of the marrow cavity, and somatic growth will continue to shape the shoulder throughout the remainder of fetal life.
At birth, the proximal humeral epiphysis, acromion, coracoid, and lateral epiphysis of the clavicle are composed of hyaline cartilage, whereas the humeral diaphysis, midportion of the clavicle, and body of the scapula are ossified. The primary physes of the clavicle and humerus are responsible for the longitudinal growth of these bones. The proximal physis of the humerus is responsible for approximately 80% of its overall elongation, whereas the lateral physis of the clavicle contributes little to the final length of the bone. Appositional growth of the diaphysis and metaphysis of the humerus and clavicle, and body of the scapula occurs by intramembranous ossification that originates from the periosteum and perichondrium.
Throughout childhood, the cartilaginous epiphyses and apophyses of the shoulder develop secondary ossification centers. These centers enlarge by endochondral ossification from a secondary physis. The age at which each epiphysis or apophysis begins to ossify and grow varies between sites, which in turn results in the changing appearance of the shoulder at different stages of skeletal maturation. The subchondral marrow of a developing ossification center and its adjacent secondary physis is similar in architecture, composition, and MR imaging characteristics to the metaphysis and primary physis of long bones. By the time skeletal maturity is reached, all epiphyseal cartilage has been replaced by mineralized bone, with the exception of articular cartilage.
The growth of bones results in increased tension on the soft tissues of the shoulder girdle. The muscles, ligaments, tendons, and joint capsule, including the labroligamentous complex, grow in response to the traction exerted on them by the growing skeleton. The signal intensity (SI) on MR images of the subcutaneous tissues also changes during growth. In neonates and infants, there are prominent deposits of brown fat in the axillary, subscapular, and parascapular regions. These normal deposits of brown fat show a slightly heterogeneous SI on T1-weighted images and may demonstrate patchy enhancement after the administration of intravenous contrast ( Fig. 1 ), which can be a source of unnecessary concern.
Technique
MR imaging of the pediatric shoulder is best performed with the patient in a supine position. Children younger than 7 years generally require sedation, whereas older patients are much more likely to tolerate the MR imaging examination without medication. The imaging protocol and the choice of appropriate coils depend on the size of the child and the clinical concern. In a young patient with a congenital or developmental abnormality, both shoulders should be imaged so that comparison can be made with the contralateral normal shoulder, as in the case of brachial plexus palsy. In these cases, a cardiac phased-array coil that covers both shoulder girdles is recommended. 3.0-T imaging is optimal. For a unilateral shoulder examination, infants and small children can be imaged using a small 4-channel multiflex coil. Older children (preteens) and adolescents are imaged using a small or large shoulder-array coil, respectively. A small field of view (FOV), such as 120 mm, is optimal for the very young patient. Older patients can be imaged adequately with a FOV ranging from 140 to 160 mm, depending on body size. When imaging a smaller child in a larger-diameter MR imaging system, it is useful to position the patient‘s body off midline thus bringing the shoulder closer to the center of the bore, to maximize the signal-to-noise ratio.
Signal characteristics of the immature skeleton
Cartilage and Marrow
Transformation from red or hematopoietic to yellow or fatty marrow starts during the first year of life. Differences in marrow composition are depicted well on T1-weighted images, as red marrow is of intermediate to low SI and yellow marrow is of high SI. On fat-suppressed fluid-sensitive sequences, red marrow is of high SI and yellow marrow is of low SI. In the upper extremity, marrow transformation proceeds from distal to proximal (ie, from the fingers toward the shoulder). In an individual bone, this transformation begins in the epiphyses, continues in the diaphysis, and ends in the metaphyses. Marrow transformation in the epiphysis of the proximal humerus begins during the first year of life, soon after its radiographic appearance. Residual foci of red marrow frequently can be seen in the metaphysis and epiphysis of the proximal humerus in older children and adolescents, even after skeletal maturity is reached. In the proximal humeral metaphysis, these foci of residual red marrow tend to be vertically oriented and have sharp margins, whereas in the epiphysis they tend to have a curvilinear configuration along the humeral head ( Fig. 2 ). In the axial skeleton, marrow transformation occurs gradually and continuously throughout life. Marrow transformation in the clavicle starts between 6 and 10 years of age, and continues into the second and third decades of life.
Hyaline cartilage of the epiphyses and apophyses is of intermediate SI on T1-weighted images and is of high SI on intermediate-weighted images ( Fig. 3 ). On fluid-sensitive sequences (short-tau inversion recovery [STIR] and T2-weighted images), the SI of epiphyseal cartilage is relatively low whereas that of the physis and articular cartilage remains high, thus providing contrast between the different forms of hyaline cartilage based on the relative content of free and bound water ( Fig. 4 ). The zone of provisional calcification can be appreciated as a thin band of very low SI on all pulse sequences, separating the physis from the metaphysis. On gradient-echo (GRE) images, all forms of hyaline cartilage are of homogeneous intermediate or high SI, and the bone is of very low SI. As in the adult, the articular cartilage of the glenoid in children is of high SI, whereas the fibrocartilaginous labrum is of homogeneous low SI on all pulse sequences.
Anatomy
Humerus
The proximal humeral epiphysis is cartilaginous at birth, and with growth develops 3 separate ossification centers: the head, the greater tuberosity, and the lesser tuberosity. The ossification center of the humeral head forms within the first months of life, but occasionally is present at birth in a full-term infant. The ossification centers of the greater and lesser tuberosities develop between 9 and 12 months of age and 12 and 16 months of age, respectively. Eventually the 3 ossification centers coalesce between 3 and 5 years of age, forming a single epiphyseal ossification center. Initially the osseous contour of the proximal humeral epiphysis can be irregular, appearing bilobed or fragmented on coronal images and demonstrating a posterior notch on axial images. As the child grows, the ossification center develops a smoother contour, becomes more hemispheric, and abuts the primary proximal humeral physis ( Fig. 5 ).
In infants and younger children, the primary physis of the proximal humerus is smooth and gently arched. With growth, it becomes increasingly undulated and multiplanar, and develops a characteristic tenting in the lateral aspect ( Fig. 6 ). Closure of the proximal humeral physis occurs at approximately 14 to 16 years of age in girls and 15 to 17 years of age in boys. Because of the substantial contribution of the proximal humeral physis to the final length of the bone, growth disturbances in this location can lead to marked deformity.
Scapula
Coracoid
In the neonatal period, the body of the scapula is ossified, but the coracoid and the acromion still are cartilaginous. During the first 3 months of life, a secondary ossification center develops in the coracoid. With time, this spherical ossification center assumes a bipolar configuration with fronts of ossification advancing toward the body of the scapula and the distal end of the coracoid. Around the age of 10 years, the proximal physis of the coracoid converges toward its base and, because of its orientation, irregular contour, and proximity to the joint, may mimic an avulsion fracture or an injury to the glenoid labrum ( Fig. 7 ).
Acromion
Three distinct ossification centers merge to form the acromion: the pre-acromion, which is located more anteriorly; the meso-acromion, which is located in the middle portion; and the meta-acromion, which is more posterior and forms the acromial angle ( Fig. 8 ). These ossification centers form during adolescence and fuse between 17 and 22 years of age. At times, the variable pattern and rate of ossification in the acromion can simulate fractures in this location. Failure of the different ossification centers to fuse appropriately has been associated with the development of an os acromiale.
Glenoid
Early in life, the subchondral bone of the glenoid appears flattened or even convex on conventional radiography; however, on MR images the cartilaginous glenoid already demonstrates its typical concave configuration and conforms to the shape of the humeral head. The bony glenoid develops from the fusion of 2 ossification centers. The first center appears at approximately 10 years of age in close proximity to the base of the coracoid, and the second one, which has a horseshoe configuration, appears at approximately 15 years of age. These ossification centers fuse, undergo transformation to fatty marrow, and fuse with the subchondral bone plate. The articular surface of the glenoid remains cartilaginous and can be readily identified as a smooth rim of high SI on MR imaging fluid-sensitive sequences. Occasionally a focal well-marginated defect in the articular cartilage can be seen in the center of the glenoid fossa on MR images. This focal thinning, also known as the bare spot of the glenoid, is less commonly seen in children than in adults.
During childhood, there is a change in the orientation of the glenoid relative to the angle of the scapula, termed the glenoid version. On MR imaging, the mean glenoid version in children younger than 2 years is −6°, or 6° of retroversion. Throughout childhood this value steadily increases, reaching adult standards of −1° by the end of the first decade of life. However, there is substantial variability in the normal values of glenoid version; approximately 68% of children have slightly retroverted glenoids, with the remaining 32% demonstrating mild anteversion.
Congenital
Brachial Plexus Palsy
Neonatal brachial plexus palsy is caused by traction on the brachial plexus (C5-T1) during labor, which results in injury to 1 or more nerve levels. The prevalence of this complication has been reported as 1 to 1.5 per 1000 live births. Predisposing factors for a brachial plexus injury include shoulder dystocia, instrumented delivery, breech delivery, and fetal macrosomia. Cesarean section has a significant protective effect. The diagnosis is made by observing arm weakness in a distribution consistent with a brachial plexus injury at birth.
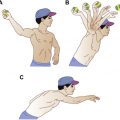
Shoulder dysfunction represents a major source of disability in infants with brachial plexus injuries. Most patients with brachial plexus birth palsy who begin to recover in the first 3 months of life can be expected to have improvement to nearly normal function. Although most infants recover, up to one-third have residual dysfunction. The most common deficit involves weakness of the external rotators of the shoulder, namely the infraspinatus and teres minor muscles, which are innervated by nerves (supraspinatus and axillary nerves, respectively) that originate from the C5 to C6 nerve roots. This weakness leads to an internal rotation contracture of the shoulder. With long-standing internal rotation, significant periarticular capsuloligamentous tightness may develop. In turn, this can lead to a posteriorly directed force on the humeral head, causing a hypoplastic humeral head and posterior humeral head displacement. On rare occasion only the C7, C8, and first thoracic nerve roots are affected, giving rise to paralysis of the lower arm. If left untreated, brachial plexus palsy can lead ultimately to shoulder dislocation and even a fixed articular deformity of both the glenoid and humeral head, with overgrowth of the coracoid.
Treatment options for neonatal brachial plexus palsy depend on the time of recognition and age at diagnosis, the degree of glenohumeral dysplasia, and the reducibility of the subluxation or dislocation if present. The goals of intervention include achieving full passive range of motion, maintenance of a stable glenohumeral articulation, and muscle rebalancing to facilitate glenoid remodeling. Early treatments include physical therapy, abduction and external rotation splints and spica casts, and injections of botulinum toxin type A to prevent contracture and to maintain full passive range of motion. Early microneurosurgical reconstruction of the brachial plexus may improve functional outcomes in children younger than 2 years. In the older child, capsular release, glenoid osteotomy, and extra-articular tendon transfers are used to restore active external rotation. Salvage options in the older child with advanced glenohumeral dysplasia include a humeral external derotational osteotomy.
Characterization of glenohumeral deformities with conventional radiographs is not possible, as the glenohumeral joint does not completely ossify until puberty. Ultrasonography has been shown to be an effective screening modality for depiction of posterior subluxation of the humeral head in infants, with optimal imaging performed at 3 and 6 months of age. As the humeral head and glenoid are largely cartilaginous, MR imaging is the preferred method of evaluation in the young child (<5 years), whereas computed tomography scans generally are reserved for the older child. The optimum protocol should include images of both shoulders to allow for comparison with the normal, unaffected shoulder. GRE sequences best demonstrate the hyaline cartilage of the humeral epiphysis and glenoid fossa, as well as the glenoid labrum in young infants. High-resolution, 3-mm thick, axial and oblique coronal GRE images are obtained to assess the presence and the degree of incongruity of the glenohumeral joint, the shape of the humeral head, the degree of glenoid hypoplasia, and the glenoid version angle. In children younger than 5 years, the cartilaginous normal glenoid shows increased SI on GRE sequences. The physis of the glenoid also will be of high SI and the labrum will be of low SI (similar to adults).The glenocapsular angle can be measured from the axial images to determine the degree of glenoid version. In the abnormal shoulder, there is thinning of the posterior aspect of the glenoid. With more severe dysplasia, the glenoid cavity often is poorly developed posteriorly, and the posterior labrum and humeral head are displaced posteriorly ( Fig. 9 ). In addition, severely affected patients will show thinning of the superior aspect of the glenoid cartilage as well as atrophy of the muscles of the shoulder girdle. The degree of rotator cuff muscle atrophy and fatty deposition, particularly the subscapularis muscle, directly correlates with development of secondary deformation of the glenohumeral joint. Given its ability to assess the cartilaginous structures and soft tissues, MR imaging is an essential tool in the initial assessment, surveillance, presurgical planning, and postsurgical evaluation of skeletally immature children with a brachial plexus injury.