• The testis is normally drawn caudad towards the inguinal canal by the gubernaculum, which is attached to its lower pole – differential growth between the gubernaculum and abdominal wall may account for this migration • 80% are found within the inguinal region and are usually palpable • It can be an isolated abnormality or in association with other abnormalities (e.g. prune-belly syndrome, Beckwith–Wiedemann syndrome, congenital rubella, renal agenesis) • Its prevalence parallels the gestational age: it is found in 100% of premature male infants weighing < 900g, 3–4% of infants > 2.5kg, < 1% of infants by 1 year (as most testes spontaneously descend) • It is a risk factor for subfertility (even if unilateral) and subsequent testicular tumour development (usually a seminoma) • Orchidopexy: this does not reduce the risk of malignancy within the ipsilateral or contralateral testis (however it does allow for earlier detection) • An abnormal twist of the spermatic cord as a result of testicular rotation • It is commonly seen during the 1st year of life or during adolescence (when the testicle is rapidly enlarging) • Gonadal stromal tumours (non-germ cell) (1%): these are of Leydig, Sertoli or theca cell origin: they are usually benign but endocrinologically active • Nodes are considered abnormal if they are > 1cm in size (however the usual issues regarding false-negative examinations and enlarged nodes due to reactive hyperplasia remain) • Testicular tumours typically spread via the lymphatics: this is initially to the para-aortic nodes (up to the level of the renal hila) • Contralateral nodal disease and inferior spread to the inguinal nodes only occurs following well-established ipsilateral disease (e.g. nodes > 2cm)
Male reproductive system
CRYPTORCHIDISM AND TESTICULAR TORSION
CRYPTORCHIDISM (UNDESCENDED TESTES)
Definition
 An undescended testis may be found anywhere along its normal course of descent from the retroperitoneum to the inguinal canal
An undescended testis may be found anywhere along its normal course of descent from the retroperitoneum to the inguinal canal
 the condition is bilateral in 10–25% of cases
the condition is bilateral in 10–25% of cases
Pearls
TESTICULAR TORSION
Definition
 Normally the tunica vaginalis converges posteriorly, fixing the testis to the scrotal wall
Normally the tunica vaginalis converges posteriorly, fixing the testis to the scrotal wall  this attachment may be deficient or patulous, allowing the testis to rotate (a ‘bell-clapper’ deformity)
this attachment may be deficient or patulous, allowing the testis to rotate (a ‘bell-clapper’ deformity)
 It can be complete (at least 360° of rotation) or incomplete
It can be complete (at least 360° of rotation) or incomplete  the degree of torsion determines the severity of testicular ischaemia and the rapidity of any irreversible changes
the degree of torsion determines the severity of testicular ischaemia and the rapidity of any irreversible changes
 Acute: lasting between 24 h and 10 days
Acute: lasting between 24 h and 10 days  subacute or chronic: > 10 days
subacute or chronic: > 10 days
PRIMARY TESTICULAR MALIGNANCIES
PRIMARY TESTICULAR MALIGNANCIES
DEFINITION
 Seminoma (40%): a peak incidence during the 4th and 5th decades
Seminoma (40%): a peak incidence during the 4th and 5th decades
 Non-seminomatous germ cell tumour (NSGCT) (60%): a peak incidence during the 3rd and 4th decades
Non-seminomatous germ cell tumour (NSGCT) (60%): a peak incidence during the 3rd and 4th decades
 there can be premature virilization (Leydig tumours secreting androgens) or gynaecomastia (Sertoli tumours secreting oestrogens)
there can be premature virilization (Leydig tumours secreting androgens) or gynaecomastia (Sertoli tumours secreting oestrogens)
RADIOLOGICAL FEATURES
CT
 inguinal nodes are not usually involved unless there is scrotal wall invasion
inguinal nodes are not usually involved unless there is scrotal wall invasion
 Left-sided lesions: these involve the upper left para-aortic chain, and are situated closer to the left renal vein than the aortic bifurcation
Left-sided lesions: these involve the upper left para-aortic chain, and are situated closer to the left renal vein than the aortic bifurcation
 Right-sided lesions: these involve the anterior inter-aorticocaval recess and paracaval nodes
Right-sided lesions: these involve the anterior inter-aorticocaval recess and paracaval nodes  deposits tend to be more caudad than left-sided metastases
deposits tend to be more caudad than left-sided metastases  they may potentially be located posterior to the 3rd part of the duodenum with an impact on surgical management
they may potentially be located posterior to the 3rd part of the duodenum with an impact on surgical management
 Distant nodal spread: para-aortic nodes
Distant nodal spread: para-aortic nodes  retrocrural nodes
retrocrural nodes  supraclavicular nodes (via the thoracic duct)
supraclavicular nodes (via the thoracic duct)  posterior mediastinal or subcarinal nodes (via direct spread through the diaphragm)
posterior mediastinal or subcarinal nodes (via direct spread through the diaphragm)
 isolated pelvic adenopathy may occur (but is more often seen with testicular maldescent or scrotal involvement)
isolated pelvic adenopathy may occur (but is more often seen with testicular maldescent or scrotal involvement)
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



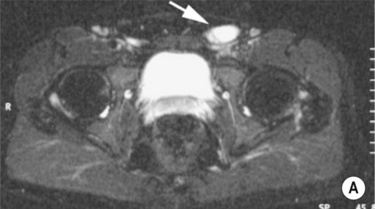
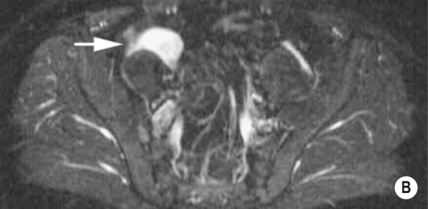
 the testis may be atrophic and difficult to locate
the testis may be atrophic and difficult to locate it is useful if an inguinal testis has not been demonstrated with US
it is useful if an inguinal testis has not been demonstrated with US T2WI and STIR: the testes are of high SI
T2WI and STIR: the testes are of high SI

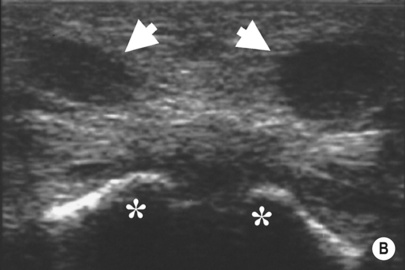
 the demonstration of normal blood flow does not exclude torsion (which can be intermittent)
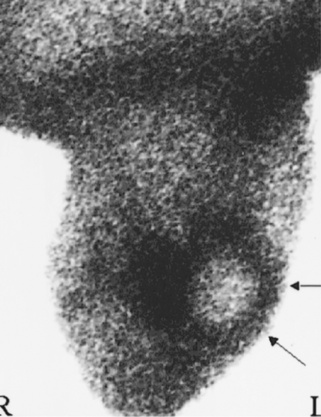
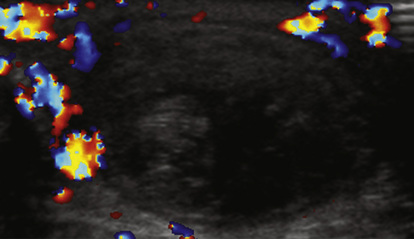
the demonstration of normal blood flow does not exclude torsion (which can be intermittent) it is often surrounded by a rim of increased activity (representing hyperaemia)
it is often surrounded by a rim of increased activity (representing hyperaemia) it demonstrates a central hypoechoic region and an associated hydrocele
it demonstrates a central hypoechoic region and an associated hydrocele  its appearances may be misleading, suggesting inflammatory change only
its appearances may be misleading, suggesting inflammatory change only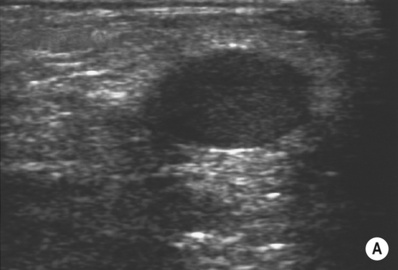

 acute pain due to haemorrhage (10% of cases)
acute pain due to haemorrhage (10% of cases) the approximate appearances:
the approximate appearances: it may be multifocal
it may be multifocal



