Malignant Bone and Soft Tissue Tumors
Clyde A. Helms
Radiographic Findings
Malignant bone tumors, thankfully, are not very common. Nevertheless, every radiologist should be able to recognize them and give a useful differential diagnosis. First, how does one recognize a malignant tumor and differentiate it from a benign process? This can be difficult and often impossible. Recognizing that it is aggressive is usually easy, but stating that it is malignant is another matter altogether. Processes such as infection and eosinophilic granuloma can mimic malignant tumors and are, of course, benign. They will often be included in the differential diagnosis of an aggressive lesion along with malignant tumors. What radiologic plain film criteria are useful for determining malignant versus benign? Standard textbooks give four aspects of a lesion to be examined: (1) cortical destruction, (2) periostitis, (3) orientation or axis of the lesion, and (4) zone of transition. Let me discuss each of these criteria and show why only the last one—the zone of transition—is accurate to a 90% plus rate. It is important to recognize that these are plain film criteria and do not apply to CT or MR imaging in many instances.
Cortical Destruction
Benign fibro-osseous lesions and cartilaginous lesions often have part of their noncalcified matrix (fibrous matrix or chondroid matrix, both of which are radiolucent on plain films) replacing cortical bone, which can give the false impression of cortical destruction on plain films (Fig. 41.1) or CT. Also, benign processes such as infection and eosinophilic granuloma can cause extensive cortical destruction and mimic a malignant tumor. It is well known that aneurysmal bone cysts cause such thinning of the cortex as to make the cortex radiographically undetectable (Fig. 41.2). For these reasons, cortical destruction can occasionally be misleading. Cortical destruction always makes one think of a malignant lesion when using the “gestalt approach,” but the lesion must also have other criteria for a malignant process, such as a wide zone of transition.
Periostitis
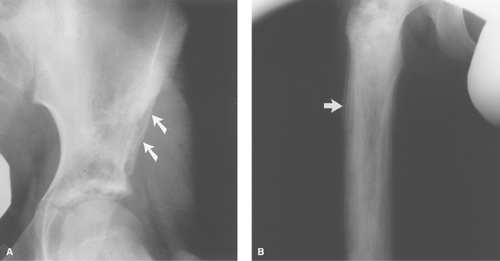
Periosteal reaction occurs in a nonspecific manner whenever the periosteum is irritated, whether it is irritated by a malignant tumor, a benign tumor, infection, or trauma. Callus formation in a fracture is actually just periosteal reaction of the most benign type. Periosteal reaction occurs in two types: benign or aggressive, based more on the timing of the irritation than on whether it is a malignant or benign process causing the periostitis. For example, a slow-growing benign tumor will cause thick, wavy, uniform, or dense periostitis (Fig. 41.3A) because it is a low-grade chronic irritation that gives the periosteum time to lay down thick new bone and remodel into more normal cortex. A malignant tumor causes a periosteal reaction that is high grade and more acute; hence, the periosteum does not have time to consolidate. It appears lamellated (onion-skinned) (Fig. 41.3B) or amorphous or even sunburst-like. If the irritation stops or diminishes, the aggressive periostitis will solidify and appear benign. Therefore, when periostitis is seen, the radiologist should try to characterize it into either a benign (thick, dense, wavy) type or an aggressive (lamellated, amorphous, sunburst) type. Unfortunately, judging the lesion by its periostitis can be very misleading. First, it takes considerable experience to characterize periostitis accurately because many times the reaction is not clearly benign or aggressive. Second, many benign lesions cause aggressive periostitis, such as infection, eosinophilic granuloma, aneurysmal bone cysts, osteoid osteomas, and even trauma. Seeing benign periostitis, however, can be very helpful because malignant lesions will not cause benign periostitis. Some investigators with great experience in dealing with malignant bone tumors state that the only way benign periostitis can occur in a malignant lesion is if there is a
concomitant fracture or infection. Exceptions to this are extremely uncommon.
concomitant fracture or infection. Exceptions to this are extremely uncommon.
Orientation or Axis of the Lesion
This is a very poor determinant of benign versus aggressive lesions and rarely helps determine into which category the
lesion should be placed. It has been said that if a lesion grows in the long axis of a long bone, rather than being circular, it is benign. There are simply too many exceptions for this to be helpful. For example, Ewing sarcoma, an extremely malignant lesion, usually has its axis along the shaft of a long bone. Conversely, many fibrous cortical defects are circular, yet totally benign. Thus, the axis of the lesion is not helpful in assessing benignity versus malignancy.
lesion should be placed. It has been said that if a lesion grows in the long axis of a long bone, rather than being circular, it is benign. There are simply too many exceptions for this to be helpful. For example, Ewing sarcoma, an extremely malignant lesion, usually has its axis along the shaft of a long bone. Conversely, many fibrous cortical defects are circular, yet totally benign. Thus, the axis of the lesion is not helpful in assessing benignity versus malignancy.
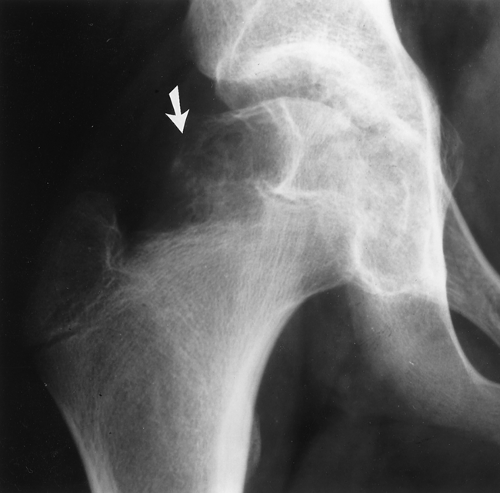
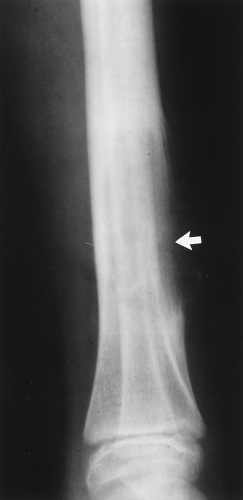 Figure 41.2. Aneurysmal Bone Cyst. This benign lesion has thinned the cortex to such a degree as to make it imperceptible (arrow). As in Figure 41.1, this could be misconstrued as cortical destruction, giving the false impression of a malignant or very aggressive lesion. |
Zone of Transition
This is without question the most reliable plain film indicator for benign versus malignant lesions. Unfortunately, it also has some drawbacks. The zone of transition is the border of the lesion with the normal bone. It is said to be “narrow” if it is so well defined that it can be drawn with a fine-point pen (Fig. 41.4). If it is imperceptible and cannot be clearly drawn at all, it is said to be “wide” (Fig. 41.5). Obviously, all shades of gray lie in between, but most lesions can be characterized as having either a narrow or wide zone of transition. If the lesion has a sclerotic border, it, of course, has a narrow zone of transition. If a lesion has a narrow zone of transition, a benign process should be considered as the most likely possibility.
The exceptions to this are rare. If a lesion has a wide zone of transition, it is aggressive, although not necessarily malignant. As with aggressive periostitis, many benign lesions as well as malignant lesions can cause a wide zone of transition. A few of the same processes that can cause aggressive periostitis and thereby mimic a malignant tumor can have a wide zone of transition (i.e., infection and eosinophilic granuloma). They are aggressive in their radiographic appearance because they are usually fast-acting, aggressive lesions. The zone of transition is usually easier to characterize than the periostitis, plus it is always present to evaluate, whereas many lesions, benign or malignant, have no periostitis. For these reasons, the zone of transition is the most useful indicator of whether a lesion is benign or malignant.
A lesion consisting of multiple small holes is said to be “permeative” (see Chapter 45 for discussion of the difference between a permeative lesion and a pseudopermeative lesion). It has no perceptible border and therefore has a wide zone of transition. Round cell tumors such as multiple myeloma, primary lymphoma of bone (reticulum cell sarcoma), and Ewing sarcoma are typical of this type of lesion. Infection and eosinophilic granuloma also can have this same appearance.
Once it is decided that a particular lesion is most likely malignant, the differential is fairly straightforward. First, the list of malignant tumors is relatively short, and, second, most tumors follow somewhat strict age groupings. Jack Edeiken, one of the preeminent bone radiologists of our era, evaluated 4000 malignant bone tumors and found that they could be diagnosed correctly 80% of the time just by using the patient’s age. He basically divides the tumors into decades of when they usually affect a patient. For example, osteosarcoma and Ewing sarcoma are the only childhood primary malignant tumors of bone, and after the age of 40, only metastatic disease, myeloma, and chondrosarcoma are common (Table 41.1). Although there are certainly outliers that are uncommon, these age guidelines are extremely useful. It is inappropriate to mention Ewing sarcoma in a 40-year-old patient or metastatic disease in a 15-year-old patient, unless there is a known primary tumor. In fact, any bone lesion, regardless of its appearance, could be a metastatic lesion and would be suspicious in a patient with a known primary tumor.
Table 41.1 Age of Patients with Malignant Bone Tumors | ||||||
|---|---|---|---|---|---|---|
|
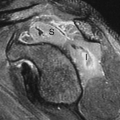
Magnetic Resonance Imaging
Although plain films are the best modality for characterizing a bony lesion, that is, being able to distinguish benign from malignant and generating a differential diagnosis, MR is without question the imaging procedure of choice for determining the extent of a lesion, both in the skeleton and in the soft tissues.
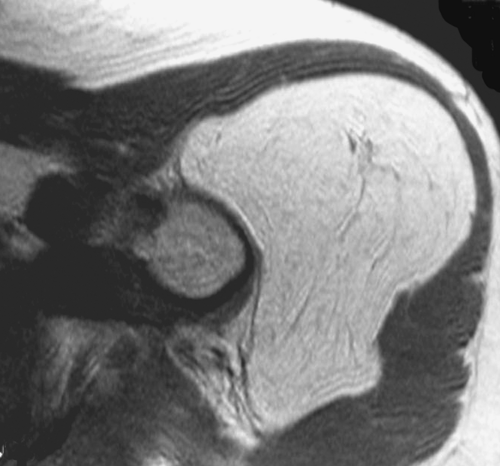
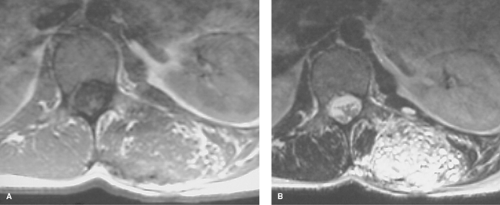
In assessing benignity versus malignancy, MR is somewhat controversial (1). Benign lesions tend to be well marginated, to have uniform and homogeneous signal, not to encase neurovascular structures, and not to invade bone. Malignant lesions tend to have irregular margins, inhomogeneous signal, and may encase neurovascular structures or invade bone.
Although almost all tumors will have low signal on T1WIs, which become very high in signal intensity with T2 weighting (as will fluid collections), there are a few exceptions. Malignant fibrous histiocytomas (MFH) and desmoid tumors can occasionally demonstrate low signal on both T1-weighted and T2-weighted sequences. Any tumor with calcification will be low in signal on both T1 and T2 sequences.
In some instances, MR will characterize the lesion better than plain films and enable a specific diagnosis to be made. Lipomas are easily diagnosed with MR by their homogeneous high signal on T1WIs and sharp margins, whether they are intraosseous or in the soft tissues (Fig. 41.6). Hemangiomas and arteriovenous malformations most commonly have mixed high and low signals on both sequences because of the combination of fatty elements and blood (Fig. 41.7). They characteristically have low-signal serpiginous vessels visible.
The finding of a low-signal mass on T1WIs that is high in signal on T2WIs is suspicious for a tumor, but this is a very nonspecific finding and needs to be correlated clinically.
Intramuscular injection sites can mimic soft tissue tumors, as can any area of soft tissue trauma. Many malignant tumors exhibit high signal radiating from involved bone, which is soft tissue edema and virtually indistinguishable from tumor spread.
Intramuscular injection sites can mimic soft tissue tumors, as can any area of soft tissue trauma. Many malignant tumors exhibit high signal radiating from involved bone, which is soft tissue edema and virtually indistinguishable from tumor spread.
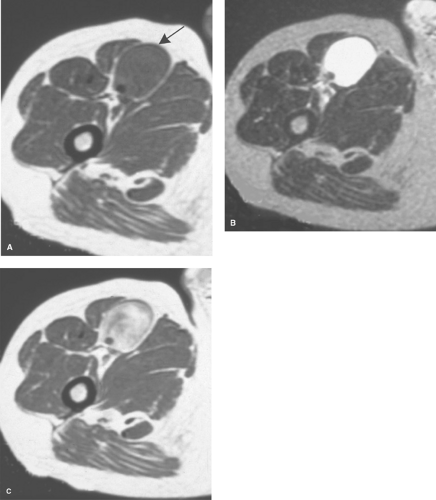 Figure 41.8. Schwannoma. A. A T1-weighted axial image shows a mass (arrow) in the anterior thigh. B. A T2WI shows homogeneous high signal identical to that seen in a fluid collection. C. A T1WI taken after administration of gadolinium shows diffuse enhancement of the mass, indicating that this is a solid tumor. Biopsy revealed this to be a schwannoma.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|