• A malignant cartilage-producing tumour – it generally has a better prognosis than an osteosarcoma (due to late metastases) • A major consideration is the differentiation between a chondroma and a low-grade chondrosarcoma • Slow growth: this allows reactive change with periosteal new bone + bone expansion + endosteal resorption (endosteal scalloping > ⅔ of the cortical width suggests a chondrosarcoma rather than a chondroma) • More aggressive tumours: cortical destruction • A malignant osteoid-producing tumour • It is the 2nd commonest primary malignant bone lesion after myeloma • Pain or a palpable mass (usually > 6cm at presentation) • 80% of cases present between 10 and 30 years • It is a highly vascular tumour with early haematogenous metastases to the lung (with a subpleural location, possible calcification and potential pneumothorax formation) • Synchronous: multiple osteoblastic metaphyseal lesions occurring in children or adolescents • Metachronous: this affects older patients, presenting with a solitary lytic or sclerotic lesion within a long or flat bone
Malignant bone tumours
CHONDROID ORIGIN
CHONDROSARCOMA
DEFINITION
 Central (intramedullary) vs peripheral
Central (intramedullary) vs peripheral
 Primary vs secondary (e.g. arising in a pre-existing bone lesion such as a central enchondroma or a peripheral osteochondroma)
Primary vs secondary (e.g. arising in a pre-existing bone lesion such as a central enchondroma or a peripheral osteochondroma)
 Grade I: low grade
Grade I: low grade  Grade II: myxoid
Grade II: myxoid  Grade III: high grade
Grade III: high grade  dedifferentiated: this refers to the development of an adjacent non-chondroid tumour (e.g. an osteosarcoma, fibrosarcoma, or MFH)
dedifferentiated: this refers to the development of an adjacent non-chondroid tumour (e.g. an osteosarcoma, fibrosarcoma, or MFH)
RADIOLOGICAL FEATURES
XR
 an increased cortical thickness (if the periosteal reaction outweighs the cortical scalloping)
an increased cortical thickness (if the periosteal reaction outweighs the cortical scalloping)
 one should consider dedifferentiation to a more malignant type
one should consider dedifferentiation to a more malignant type
PEARLS
OSTEOSARCOMA
OSTEOSARCOMA
DEFINITION
 it is commonly a primary central osteosarcoma (75%)
it is commonly a primary central osteosarcoma (75%)
CLINICAL PRESENTATION
 pathological fracture
pathological fracture
 there is a 2nd smaller peak occurring above the age of 40 years which is seen commonly within the flat bones and vertebrae and usually secondary to a pre-existing disorder (e.g. Paget’s disease)
there is a 2nd smaller peak occurring above the age of 40 years which is seen commonly within the flat bones and vertebrae and usually secondary to a pre-existing disorder (e.g. Paget’s disease)
PEARLS
 occasionally there are lymphatic metastases
occasionally there are lymphatic metastases
Primary multicentric osteosarcoma
 it has a poor prognosis
it has a poor prognosis
 multiple lesions are seen after more than 5 months
multiple lesions are seen after more than 5 months  this has a better prognosis than a synchronous lesion
this has a better prognosis than a synchronous lesion
Malignant bone tumours

 it can present with insidious pain, a palpable mass or a pathological fracture
it can present with insidious pain, a palpable mass or a pathological fracture it is found within the metaphysis (± epiphyseal extension)
it is found within the metaphysis (± epiphyseal extension) there is a narrow zone of transition
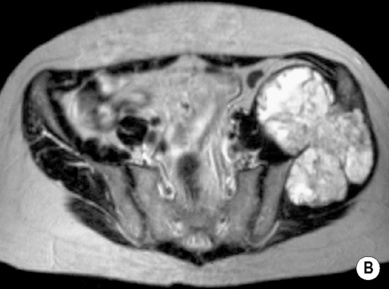
there is a narrow zone of transition T2WI: multilobulated high SI lesion
T2WI: multilobulated high SI lesion  matrix mineralization appears as foci of signal void
matrix mineralization appears as foci of signal void  T1WI + Gad: minimal peripheral or septal enhancement (as it is poorly vascularized)
T1WI + Gad: minimal peripheral or septal enhancement (as it is poorly vascularized)


 it involves the long bones (usually the distal femoral or proximal humeral metaphyses)
it involves the long bones (usually the distal femoral or proximal humeral metaphyses)  there is a good prognosis after resection
there is a good prognosis after resection it has a very much more cellular malignant matrix than a normal chondrosarcoma
it has a very much more cellular malignant matrix than a normal chondrosarcoma there is often chondroid calcification
there is often chondroid calcification  there is a predilection for the ribs and mandible
there is a predilection for the ribs and mandible it is a low-grade tumour with a better prognosis
it is a low-grade tumour with a better prognosis it has a lytic appearance (± a loculated or ‘soap bubble’ appearance)
it has a lytic appearance (± a loculated or ‘soap bubble’ appearance)






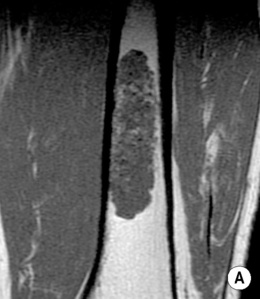





 it can cross the growth plate with epiphyseal extension seen in 75% of cases
it can cross the growth plate with epiphyseal extension seen in 75% of cases there is a wide zone of transition
there is a wide zone of transition  there can be cortical destruction with an extraosseous mass and cloud-like matrix mineralization
there can be cortical destruction with an extraosseous mass and cloud-like matrix mineralization reactive Codman’s triangles are seen at the margins of the lesion
reactive Codman’s triangles are seen at the margins of the lesion
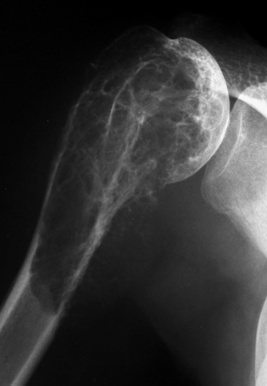
 malignant change is reported in up to 14% of cases of Paget’s disease (M:F, 2:1)
malignant change is reported in up to 14% of cases of Paget’s disease (M:F, 2:1)  it should be suspected if there is a change in pain or a pathological fracture
it should be suspected if there is a change in pain or a pathological fracture  it has a very poor prognosis
it has a very poor prognosis the spine is usually spared
the spine is usually spared it is usually an osteosarcoma with a mean latency period of 15 years
it is usually an osteosarcoma with a mean latency period of 15 years  it commonly occurs within the pelvis and shoulder girdle and has a poor prognosis
it commonly occurs within the pelvis and shoulder girdle and has a poor prognosis a > 3 year latency
a > 3 year latency  a histology different from the original tumour
a histology different from the original tumour






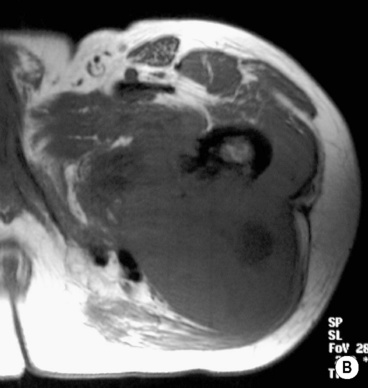
 it is slow growing with a good prognosis (which may dedifferentiate)
it is slow growing with a good prognosis (which may dedifferentiate)  it has an equal sex incidence
it has an equal sex incidence it may wrap around the bone
it may wrap around the bone  satellite bony masses can be seen in the adjacent soft tissue
satellite bony masses can be seen in the adjacent soft tissue T2WI: high SI at the periphery may indicate higher grade or dedifferentiation
T2WI: high SI at the periphery may indicate higher grade or dedifferentiation juxtacortical myositis ossificans
juxtacortical myositis ossificans there is a slight male preponderance
there is a slight male preponderance there is rarely nodular matrix calcification
there is rarely nodular matrix calcification






