Chapter Outline
Intrahepatic Cholangiocarcinoma
Cystadenoma and Cystadenocarcinoma
Undifferentiated (Embryonal) Sarcoma
Epithelial Hemangioendothelioma
Other Mesenchymal Sarcomas (Leiomyosarcoma, Malignant Fibrous Histiocytoma)
Differential Diagnosis—Incidental Mass
Primary malignant neoplasms of the liver are classified by the cell of origin ( Box 87-1 ). Secondary malignant liver tumors are metastases and lymphomas. Overall, metastases are the most frequent malignant tumors of the liver, except in patients with preexisting cirrhosis, in whom primary malignant neoplasms are more frequent.
Hepatocellular Origin
Hepatocellular carcinoma
Atypical hepatocellular carcinoma
Clear cell carcinoma
Giant cell carcinoma
Childhood hepatocellular carcinoma
Carcinosarcoma
Fibrolamellar carcinoma
Hepatoblastoma
Sclerosing hepatic carcinoma
Cholangiocellular Origin
Cholangiocarcinoma
Cystadenocarcinoma
Mesenchymal Origin
Angiosarcoma
Epithelioid hemangioendothelioma
Leiomyosarcoma
Fibrosarcoma
Malignant fibrous histiocytoma
Primary lymphoma
Primary hepatic osteosarcoma
In this chapter, primary malignant liver tumors of hepatocyte origin are discussed first: hepatocellular carcinoma, fibrolamellar carcinoma, and hepatoblastoma. Intrahepatic carcinoma and cystadenocarcinoma that arise from biliary cells are then considered. Angiosarcoma, undifferentiated (embryonal) sarcoma, epithelial hemangioendothelioma, and other mesenchymal sarcomas that originate in the mesenchymal tissue are reviewed. Finally, the secondary liver tumors, lymphomas and metastases, are discussed.
Hepatocellular Carcinoma
Pathologic Findings
Hepatocellular carcinoma (HCC) is the most common primary hepatic tumor and one of the most common visceral malignant neoplasms worldwide. Terms such as hepatoma and primary liver cancer are often used synonymously with HCC, but they should be avoided in the interest of clarity and the term hepatocellular carcinoma should be encouraged.
HCC is a malignant lesion composed of cells that attempt to differentiate into normal liver, mimicking hepatocyte cords. However, their abnormal growth prevents the malignant hepatocytes from forming normal hepatic acini. Several clinical and histologic patterns occur, and the prognosis differs according to the associated condition (e.g., cirrhosis) and the extent of the tumor at diagnosis.
In gross appearance, there are three major patterns of growth ( Fig. 87-1 ): single or massive HCC characterized by the presence of a solitary, often large, mass; nodular or multifocal HCC, in which multiple well-separated nodules are seen throughout the liver, mimicking the appearance of metastases; and diffuse or cirrhotomimetic HCC, in which multiple small foci are seen throughout the liver in a diffuse manner.

A gross variant, encapsulated HCC, has a better prognosis because of its greater resectability ( Fig. 87-2 ). Regardless of its gross appearance, HCC is a soft tumor that frequently undergoes necroses and hemorrhages because of lack of stroma. Vascular invasion of perihepatic vessels is common. Conversely, biliary invasion is uncommon.

On microscopic examination, the cells of HCC resemble normal liver cells, and it is often difficult to distinguish normal hepatocytes from cells of HCC or hepatocellular adenoma. This is of considerable importance in planning an aspiration biopsy of a focal liver lesion. In some cases, the malignant hepatocytes are so well differentiated that they even produce bile, which is seen in tumor cells and in biliary canaliculi. A variety of products can be produced by the abnormal hepatocytes of HCC: Mallory bodies, α-fetoprotein, α 1 -antitrypsin, and other serum proteins. Fat and glycogen are often present in the cytoplasm of HCC hepatocytes. If there are large amounts of fat, the tumor is called clear cell carcinoma of the liver.
The most frequent HCC histologic growth pattern is trabecular, in which the tumor cells attempt to recapitulate the cords seen in normal liver. The trabeculae are separated by vascular spaces with no stroma or supportive connective tissue. On occasion, the center of the trabeculae contains tumor secretions, giving the tumor a pseudoglandular or acinar pattern. In other cases, the trabeculae grow together, producing a solid pattern ( Fig. 87-3 ).

These microscopic variations are important for the radiologist to appreciate because cellular HCCs may appear similar to normal liver, so that only subtle changes in density or echogenicity may be present. However, if there is fat deposition or pseudogland formation, the HCC may appear hyperechoic on ultrasound studies, hypodense on computed tomography (CT) scans, and hyperintense on magnetic resonance imaging (MRI).
The radiologic correlates of the pathology of HCCs are listed in Box 87-2 .
To Assess Vascularity
Contrast-enhanced computed tomography
Gadolinium-enhanced magnetic resonance imaging
Contrast-enhanced ultrasound
Angiography
Blood pool studies ( 99m Tc-labeled red blood cells)
To Assess Hepatocyte Function or Biliary Excretion
Magnetic resonance imaging enhanced with hepatocyte-specific contrast agents
To Assess Metabolic Activity of Neoplasms
18 F-FDG positron emission tomography
To Assess Kupffer Cell Activity
Magnetic resonance imaging enhanced with intravenous superparamagnetic iron oxide
To Assess Tumoral Calcification
Computed tomography
Ultrasound
Plain radiography
To Assess Capsule Presence
Computed tomography (enhanced or unenhanced)
Ultrasound (enhanced or unenhanced)
Magnetic resonance imaging (enhanced or unenhanced)
To Assess Internal Nature of Neoplasms (e.g., solid versus cystic, hemorrhage, fibrosis)
Computed tomography
Magnetic resonance imaging
Ultrasound
An important challenge for radiologists and pathologists lies in the early diagnosis of HCC, particularly within a cirrhotic liver. Successful treatment of HCCs with any of the available therapies, such as surgical resection, liver transplantation, percutaneous ethanol injection, and transcatheter embolization, is most likely if the lesion is small, so early detection is critical. With this aim, an attempt has been made to standardize the terminology of nodular liver lesions, thereby clarifying the pathogenesis of HCC in the cirrhotic liver and enhancing the early diagnosis of premalignant nodules and small HCCs. A cirrhotic nodule is defined as a regenerative nodule composed of hepatocytes and is largely or completely surrounded by fibrous septa. A “dysplastic” nodule, which is an intermediate stage between a cirrhotic nodule and HCC, is at least 1 mm in diameter and contains areas of dysplasia but no histologic evidence of malignancy. Synonyms for dysplastic nodule include adenomatous hyperplasia and macroregenerative nodule. Dysplastic nodules are subdivided into low-grade and high-grade types on the basis of findings at light microscopy. It is widely accepted that dysplastic nodules are premalignant, although the exact mechanisms of transformation of cirrhotic nodule to dysplastic nodule to HCC have yet to be defined.
Incidence and Clinical Presentation
Although HCC has a similar histologic appearance worldwide, it has a bimodal geographic distribution in terms of incidence and clinical presentation. It is rare in the Western hemisphere (low-incidence areas) and relatively frequent in sub-Saharan Africa and Asia (high-incidence areas).
Even in the United States, the incidence varies. According to the World Health Organization, the incidence ranges from 0.9 per 100,000 in women in New York to 30.9 per 100,000 in men of Chinese origin in San Francisco. Worldwide, the highest incidence is in Japan, where it is reported to be as high as 4.8%.
Clinically, in the low-incidence areas, symptoms are insidious in onset and include malaise, fever, and abdominal pain. Jaundice is rare. Liver function test results are normal and indistinguishable from those in cirrhosis, except for elevation of the α-fetoprotein level. Other proteins produced by HCC may give rise to numerous paraneoplastic syndromes, such as erythrocytosis, hypercalcemia, hypoglycemia, hypercholesterolemia, and hirsutism. The usual age at presentation in the low-incidence areas is 70 to 80 years, and the male/female ratio is 2.5 : 1. Most patients have a long history of alcoholic cirrhosis, hemochromatosis, or steroid use.
In the high-incidence areas, the age at presentation is younger (30-45 years), and men are affected eight times more frequently than women. The primary etiologic factors in high-incidence areas are hepatitis B and C viruses and exposure to aflatoxins. In these areas, HCC is aggressive and may be manifested with hepatic rupture and massive hemoperitoneum.
Radiologic Findings
Plain Radiography
When it is sufficiently large, HCC may appear as a nonspecific upper abdominal mass on plain abdominal radiographs. Calcification is rare in the typical HCC but more common in other hepatocellular neoplasms, such as fibrolamellar carcinoma. In patients with hemochromatosis, plain radiographs of the extremities demonstrate degenerative changes with calcium pyrophosphate deposition disease in cartilages.
Nuclear Medicine
Nuclear medicine is only occasionally used for the detection of HCC. On sulfur colloid studies of Western patients, HCC is manifested as a defect in a cirrhotic liver. Hepatomegaly with heterogeneous uptake of the radionuclide and colloid shift to the spleen and bone marrow are frequently noted. It is reported that 30% to 50% of HCCs are not 18 F-fluorodeoxyglucose ( 18 F-FDG) avid or are only mildly avid because of the abundant amount of the enzyme glucose-6-phosphatase in certain types of HCC. Glucose-6-phosphatase dephosphorylates FDG-6-phosphatase, and as a result of this, FDG “leaks back” into the circulation. However, the use of 11 C-acetate as a positron emission tomography (PET) tracer for detection of kinetics and uptake characteristics of fatty acid synthesis in HCC has shown promising results. Well-differentiated HCC, which tends to show negative uptake for FDG because of glucose-6-phosphatase, has uptake of 11 C. Unfortunately, 11 C has a short half-life of 20 minutes, which leads to the need for an on-site cyclotron. Therefore, in routine situations, there is little role of PET or PET/CT in the diagnosis or staging of HCC.
The soft tissue contrast of liver MRI is far more superior to that of PET for the detection of small primary HCC (<2 cm), especially when liver-specific contrast agents are used. Furthermore, functional MRI techniques, such as diffusion-weighted MRI, have been demonstrated to significantly improve the detection rate of subcentimeter-sized intrahepatic metastasis of HCC compared with conventional MRI alone. If the high sensitivity of liver MRI and the potential of functional MRI can be transferred to combined PET/MRI, it can show a performance no less than that of MRI for the primary diagnosis of HCC. The major advantage of PET/MRI scanners is that MRI evaluation of primary tumor extent and PET evaluation for whole body staging can be performed with a single examination.
PET/MRI unites the high soft tissue contrast of MRI, the data of functional MRI, and the metabolic information of PET in the evaluation of tumor volume and viability. PET can serve as a tool for differentiating HCCs with low biologic behavior and highly aggressive biologic behavior by measuring tumor 18 F-FDG uptake (standardized uptake value). The aggressiveness of biologic behavior is related to the volume doubling time of HCC and thus is predictive for survival rate, with an inverse relation between the standardized uptake value and survival rate.
Furthermore, 18 F-FDG PET imaging has been proved to be useful for the detection of tumor recurrence in HCC patients after liver transplantation and interventional therapy. Although there are studies outlining the high potential of functional MRI techniques, such as dynamic contrast-enhanced MRI and diffusion-weighted MRI, as partners in combination with PET, the exact sensitivity and specificity of PET/MRI for tumor recurrence are still in question.
Ultrasound
The sonographic appearance of HCC is varied ( Fig. 87-4 ). These lesions are frequently hyperechoic, particularly if there is fatty change or marked sinusoidal dilation. Ultrasonography can detect extremely small tumors and, in combination with serum α-fetoprotein assays, serves as an excellent screening method for high-risk patients with long-standing cirrhosis. This approach to patients has been successful in Asia but has been found to be far less accurate in the United States because of differences in patient body habitus and sonography expertise.







Some authors explain the varied sonographic appearance of HCC on the basis of size. Small HCCs (<3 cm) often appear hypoechoic and are associated with posterior acoustic enhancement; tumors larger than 3 cm more often have a mosaic or mixed pattern. Ultrasound is also capable of demonstrating the capsule in encapsulated HCC, which appears as a thin, hypoechoic band.
Sonography, in conjunction with color and duplex Doppler imaging, can diagnose tumor thrombus in the portal and hepatic veins as well as in the inferior vena cava.
Color Doppler ultrasound has been used to assess the vascularity of HCC. These data plus the resistive index of tumor vessels have been used to differentiate HCC from other tumors. Color Doppler ultrasound demonstrates an intralesional tangle of vessels, the “basket” pattern, in up to 15% of cases, indicating hypervascularity and tumor shunting. Power Doppler has also been assessed in the characterization of HCCs. Although most HCCs show a central pattern of vascularity, so do some hemangiomas and metastases, and the clinical usefulness of this technique is therefore limited.
The introduction of intravascular contrast agents has improved the ability of ultrasound to diagnose HCC. An HCC typically demonstrates an early hyperperfusion compared with the adjacent normal liver tissue. A chaotic vessel dysmorphology and washout during the portal venous phase are the other characteristics of the tumor.
Computed Tomography
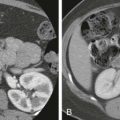
Unenhanced CT scans demonstrate a large, hypodense mass with central areas of lower attenuation that correspond to the tumor necrosis frequently seen in HCC ( Figs. 87-5 and 87-6 ). In North American and European patients, the remainder of the liver shows cirrhosis (60%) or hemochromatosis (20%) ( Fig. 87-7 ).



Multiphasic multidetector computed tomography (MDCT) including nonenhanced, hepatic arterial, portal venous, and delayed phase images is an efficient technique for determination of HCC and preoperative staging of HCC. Because HCC derives most of its blood supply from the hepatic artery, the tumor demonstrates early enhancement during arterial phase and is relatively hypodense on the delayed phase images because of the early washout of contrast medium by arterial blood (see Figs. 87-5 and 87-6 ). The tumor has a variable appearance on the portal phase images. Small tumors may appear as lesions of different attenuation, whereas larger ones almost always demonstrate central necrosis (see Fig. 87-7 ). The capsule appears isodense or hypodense relative to the liver during the hepatic arterial phase and enhances on delayed CT images (see Fig. 87-7 ).
HCC has a tendency to invade the portal and hepatic veins so that an enlarged venous segment that exhibits intraluminal low attenuation is highly suggestive of tumor thrombus. Differential diagnosis of tumor thrombus can be made through demonstration of the expansion of the main portal vein diameter (≥23 mm) and intrathrombus neovascularity on arterial phase images. Hepatic venous tumor thrombus may extend into the inferior vena cava and even to the right atrium in some cases. CT can also depict complications of HCC, such as hemoperitoneum associated with rupture of HCC and vascular invasion. Ruptured tumors tend to be located in the periphery of the liver and have a protruding contour. On arterial phase images, a ruptured tumor appears as a nonenhancing hypodense lesion with focal discontinuity and peripheral rim enhancement. This finding is termed the enucleation sign because of its similarity to an enucleated orbital globe with the remaining intact sclera.
An additional role for CT lies in the noninvasive evaluation of hepatic arterial anatomy in potential candidates for liver transplantation. In the majority of cases, three-dimensional (3D) CT arteriography is comparable to conventional arteriography and surgical findings in the delineation of the major hepatic arteries. The technique of 3D CT angiography is safe, convenient, and less invasive than conventional arteriography ( Fig. 87-8 ).

In patients with underlying hemochromatosis, a dense liver resulting from iron deposition is identified on unenhanced CT scans.
Angiography
On angiography, HCC is a hypervascular tumor with marked neovascularity and arteriovenous shunting. A large hepatic artery, abnormal vessels, and vascular invasion are usually present. Avascular or hypovascular areas may be present as a result of necrosis or hemorrhage. Extension of the tumor into the porta hepatis and other perihepatic veins is frequently detected. Hepatic venous tumor thrombus has been described in 6% of cases. The presence of the “threads and streaks” sign is characteristic of this intravenous tumor thrombus.
Although biliary invasion by HCC is rare, percutaneous or retrograde cholangiography and magnetic resonance cholangiopancreatography (MRCP) may occasionally demonstrate that the tumor is causing obstruction or a mass within the biliary tree.
Magnetic Resonance Imaging
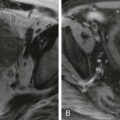
On MRI, HCC has a variable appearance ( Figs. 87-9 to 87-11 ) with low-intensity, isointensity, and high-intensity patterns seen on T1-weighted images, depending on the degree of fatty change, the presence of internal fibrosis, and the dominant histologic pattern. The capsule of encapsulated HCCs is visualized as a hypointense rim in T1-weighted images.



MRI has also been used to differentiate small HCCs from regenerative nodules of cirrhosis. Cirrhotic nodules are usually of high signal intensity on T1-weighted images. On T2-weighted images, cirrhotic nodules are isodense or hypointense to the liver. The relative hypointensity is due to greater accumulation of iron within the nodule than in surrounding liver. Also, the inflammatory fibrous septa within the liver demonstrate increased signal on T2-weighted images, and consequently cirrhotic nodules appear relatively hypointense. In contrast, HCCs are often hyperintense on T2-weighted images and can be distinguished from hypointense nodules. However, some well-differentiated HCCs have signal characteristics similar to cirrhotic nodules, and diagnosis is less straightforward. HCC arising within a siderotic nodule has a characteristic “nodule within a nodule” appearance on MRI. The HCC appears as a small focus of high signal intensity within the low signal intensity nodule. These lesions are often demonstrated only at MRI, and MR-guided biopsy is now being performed at many centers. However, biopsy may be technically difficult because the lesions are small; direct referral for surgery may be a better option if the patient is a good surgical candidate.
As with CT, HCC during dynamic gadolinium-enhanced MRI ( Fig. 87-12 ; see also Fig. 87-9 ) shows early enhancement in the hepatic arterial phase. In the portal venous phase, the tumor is usually isointense; in delayed phase, it becomes hypointense because of the washout of contrast medium. However, some tumors may show progressive enhancement in the dynamic imaging. HCCs larger than 1.5 cm tend to have a fibrous capsule that may be demonstrated as a hypointense band on delayed phase images. MRI depicts vascular invasion, which is seen in 30% to 50% of patients, as a lack of signal void on multislice T1-weighted gradient recalled echo and flow-compensated T2-weighted fast spin-echo images. On gadolinium-enhanced images, the tumor thrombus shows a typical early arterial enhancement.

Intravenous administration of superparamagnetic iron oxide (SPIO) also increases the detection sensitivity of MRI. MRI with SPIO is especially helpful in the detection of small HCCs in cirrhotic livers. In a study, more HCCs were detected on images acquired with SPIO-enhanced fast low-angle shot and long repetition time sequences (2000/70 and 2000/28) than on unenhanced scans. A potential limitation of this technique is that early HCCs may accumulate iron because of the presence of reticuloendothelial cells and will therefore mimic normal liver parenchyma on SPIO-enhanced sequences. In these cases, unenhanced MR images may provide valuable information concerning the internal morphology of these lesions, enabling the correct diagnosis of HCCs. Hepatobiliary contrast agents such as gadoxetate (Gd-EOB-DTPA) may be useful in the characterization of questionable lesions. Use of hepatobiliary contrast agents may allow differentiation of hepatocellular tumors such as HCC from nonhepatocellular tumors.
Preliminary studies suggest that on delayed images with a hepatobiliary contrast agent, well-differentiated HCCs often behave like hepatocytes, appearing isointense or sometimes hyperintense, whereas poorly differentiated HCCs typically do not accumulate the contrast agent and appear relatively hypointense. Although accumulation of contrast material in a lesion does not exclude HCC, if HCC accumulates a hepatobiliary contrast agent, it is postulated to be well differentiated.
Approximately 15 to 20 minutes after the injection Gd-EOB-DTPA, in the hepatocytic phase, hepatocytes take up contrast agent by transporter of organic anion-transporting polypeptides 1B3 (OATP1B3). Gd-EOB-DTPA works as a T1-shortening agent at the hepatocytic phase, and malignant liver lesions, such as HCC and metastases, are spared from the uptake of contrast material that occurs in the background liver parenchyma.
HCC usually appears hypointense relative to background liver signal intensity in the hepatocellular phase, probably owing to impaired expression of the membrane cotransporters necessary for uptake of the contrast agent. A minority of HCCs appear isointense or hyperintense relative to the background liver signal intensity, demonstrating hepatocellular phase uptake. It is reported that there is a significant correlation between the level of expression of OATP1B3 and the enhancement ratio within the tumors. On the basis of the data published to date, it appears that HCCs with uniform signal hyperintensity in the hepatocellular phase may be well or moderately differentiated but are rarely if ever poorly differentiated.
Many small hypovascular HCCs can be detected only on hepatocytic phase images, showing no arterial enhancement and only mild washout in the portal venous and equilibrium phases of dynamic MDCT and dynamic MRI with Gd-DTPA ( Fig. 87-13 ).

Gd-EOB-DTPA–enhanced MRI can reveal HCC as a nodule appearing hypointense relative to the background liver parenchyma regardless of its histologic differentiation ( Figs. 87-14 and 87-15 ). Gd-EOB-DTPA–enhanced MRI has higher sensitivity for detection of hypovascular and hypervascular HCCs compared with either dynamic MDCT or dynamic MRI with Gd-DTPA. Gd-EOB-DTPA–enhanced MRI also has higher sensitivity for detection of hypovascular HCC or hypervascular HCC compared with SPIO-enhanced MRI.


Regenerative nodules and dysplastic nodules are the two key cirrhotic nodular lesions that are important to identify and differentiate from HCC. Regenerative nodules have primarily portal venous blood supply with mild contribution from hepatic artery blood. Therefore, they typically do not show early enhancement during the arterial phase of dynamic MRI while enhancing with the rest of the liver in the portal phase. Regenerative nodules are usually isointense on both T1- and T2-weighted images, with the exception of some “siderotic” nodules that contain iron and therefore have a low signal intensity on T1- and T2-weighted MRI.
Dysplastic nodules develop from regenerative nodules and are present in 15% to 25% of cirrhotic livers. Although they contain atypical hepatocytes, they do not have definite features of malignancy on histology. Depending on the degree of differentiation, they are histologically classified as low grade or high grade. Although high-grade ones may develop arterial hypervascularity, dysplastic nodules receive their blood supply mainly from the portal vein. High-grade dysplastic nodules are considered premalignant and can undergo malignant transformation within a short time like 4 months ( Fig. 87-16 ). Nevertheless, the clinical significance of dysplastic nodules is unclear, and current management guidelines do not advocate aggressive workup of suspected dysplastic nodules.

Their usual MR appearance is that of homogeneous hyperintensity on T1-weighted images and hypointensity on T2-weighted images. A high signal intensity focus within a low signal intensity nodule on T2-weighted images is the nodule within a nodule appearance of a dysplastic nodule with a focus of HCC.
After administration of Gd-EOB-DTPA, in the hepatocyte phase, regenerative nodules generally take up and excrete contrast material because of preserved hepatocellular function and intact organic ion transporters, showing signal intensity similar to liver parenchyma. The number of expressed organic ion transporters decreases with progression of atypia in dysplastic nodules, reducing their ability to take up Gd-EOB-DTPA. Dysplastic nodules that retain their ability to take up but not to excrete the contrast media appear homogeneously or heterogeneously hyperintense because of intracellular cholestasis, whereas nodules that lost their ability to take up contrast media appear hypointense in the hepatocyte phase of Gd-EOB-DTPA. Such hypointense nodules can be mistaken for HCCs in the hepatocyte phase, and their interpretation is not fully understood.
Studies have shown that diffusion-weighted imaging can be helpful in differentiating cysts and hemangiomas from solid lesions, but differentiation among different solid lesions such as HCC, focal nodular hyperplasia (FNH), and adenoma may be challenging on the basis of apparent diffusion coefficient (ADC) values alone. A mass in a cirrhotic liver that shows restricted diffusion favors a solid lesion and is more likely to be HCC, especially when other supporting MRI features are present. Conversely, not all HCCs show restricted diffusion on diffusion-weighted imaging. A hepatic mass demonstrating MRI features of hepatoma even with the absence of restricted diffusion can still be HCC. Diffusion-weighted imaging has also been used for monitoring of response to therapies such as transarterial chemoembolization and radioembolization; however, the utility of diffusion-weighted imaging in differentiation of tumor grades is not clearly established.
Fibrolamellar Carcinoma
Pathologic Findings
Fibrolamellar carcinoma (FLC) is a slow-growing tumor that arises in normal liver. It is composed of neoplastic hepatocytes separated into cords by lamellar fibrous strands. These lesions have a distinctive microscopic pattern with eosinophilic, malignant hepatocytes containing prominent nuclei ( Fig. 87-17 ). Some of the markers usually present in typical HCC, such as inclusions of α-fetoprotein bodies, are not present. The fibrous component accounts for half of the tumor distributed in multilamellate strands, except in larger tumors containing large central scars.

FLC usually arises in a normal liver, with only 20% of patients having underlying cirrhosis. Satellite nodules are often present. The gross appearance of FLC is somewhat similar to that of FNH in that both tumors have a central scar and multiple fibrous septa. Hemorrhage and necrosis are rare. Radiologic-pathologic correlates are given in Table 87-1 .
| Pathologic Features | Radiologic Features |
|---|---|
| Lamellar fibrosis (septa), “true scar” | Hypovascular: CT, angiography |
| Hypointense: T2-weighted MRI | |
| Calcification: CT, plain radiography, ultrasound | |
| No necrosis or hemorrhage | Homogeneous mass: CT, ultrasound, MRI |
| No underlying cirrhosis | Normal hepatic morphology except for mass: CT, ultrasound, MRI |
Incidence and Clinical Presentation
There is some confusion in the literature about the incidence and clinical presentation of FLC because it was not recognized as a biologic entity until the 1980s. FLC usually occurs in adolescents and adults younger than 40 years and without underlying cirrhosis or other predisposing risk factors. There is no sex predominance, and the mean survival is considerably better than that for other types of HCC (45-60 months vs. 6 months), with a high likelihood of cure (40%) if the tumor is surgically resectable.
Clinically, patients with HCC usually present with pain, malaise, and weight loss; jaundice occurs only occasionally, when FLC invades the biliary tree. A palpable mass is seen in two thirds of patients. α-Fetoprotein levels are usually normal.
Radiologic Findings
Plain Radiography
On plain abdominal radiographs, FLC frequently appears as a partially calcified upper abdominal mass.
Nuclear Medicine
Nuclear medicine is no longer routinely used in the detection of FLC. Sulfur colloid scintiscans usually demonstrate a defect in a liver that has no evidence of underlying cirrhosis. Multiple defects can be seen in cases of multifocal FLC.
Ultrasound
Sonography typically demonstrates a large, well-defined, lobulated mass ( Fig. 87-18 ) with variable echotexture. FLC usually is of mixed echogenicity (60% of cases) and predominantly contains hyperechoic or isoechoic components. If the central scar is present, it may be visualized as a central area of hyperechogenicity.

Computed Tomography
On unenhanced CT scans, FLC appears as a hypodense mass with a well-defined contour ( Figs. 87-19 and 87-20 ). Areas of decreased density within the tumor correspond to the central scar or necrosis and hemorrhage. Stellate calcification within the central scar can also occur. During the arterial and portal phases of dynamic enhanced CT, the “nonscar” portion of FLC enhances heterogeneously. This heterogeneous enhancement pattern during the arterial and portal phases probably corresponds to the more vascular, cellular portions of the tumor in comparison with the fibrous (lamellae and scar) and necrotic portions. On the other hand, the relative delayed phase homogeneity of the tumor probably reflects the washout of the contrast material from its more vascular portions together with delayed enhancement of the fibrous lamellae. In some cases, central scar may also demonstrate delayed enhancement, and the appearance of the tumor, on delayed images, may closely simulate that of FNH. Although FLC is a tumor not characteristically encapsulated, the compressed liver tissue adjacent to it may demonstrate delayed enhancement. Features that determine the resectability of FLCs, such as portal vein invasion and lymphadenopathy, are well seen on CT scans.


Angiography
On angiography, FLC is a hypervascular tumor with compartmentalization in the capillary phase resulting from multiple fibrous septa. Daughter nodules or secondary lesions may be noted in the capillary phase of arteriography.
Magnetic Resonance Imaging
FLC is hypointense or isointense with normal liver on T1-weighted images and isointense or slightly hyperintense on T2-weighted images. Because of its purely fibrous nature, the scar is hypointense on both T1- and T2-weighted images ( Fig. 87-21 ). However, hyperintensity of the central scar on T2-weighted images has been described in a biopsy-proved FLC that was initially diagnosed as FNH on the basis of imaging findings alone. The enhancement pattern of FLC seen with gadolinium-enhanced dynamic MRI parallels the enhancement seen with dynamic contrast-enhanced CT. The tumor demonstrates heterogeneous enhancement in the arterial and portal phases and progressively becomes more homogeneous on delayed images ( Fig. 87-22 ).


On hepatocyte phase images, fibrolamellar HCC appears predominantly hypointense, but components of the tumor may show some uptake of Gd-EOB-DTPA, indicative of a primary liver lesion. FNH, on the other hand, shows intense uptake of hepatocyte-specific (hepatobiliary) contrast agents during the hepatobiliary phase.
Differential Diagnosis
The major differential diagnosis with FLC is FNH. FNH can be differentiated from FLC in the majority of cases because the central scar of FNH is hyperintense on T2-weighted images. FNH rarely has calcification within the scar (<1.5% of cases compared with up to 55% of FLC). FNH is usually asymptomatic, whereas patients with FLC usually present with some symptoms. FNH shows strong uptake of hepatobiliary contrast agents. Biopsy demonstrates malignant, eosinophilic hepatocytes in FLC and normal hepatocytes with bile ductules in FNH ( Table 87-2 ).
| Features | Focal Nodular Hyperplasia | Fibrolamellar Carcinoma |
|---|---|---|
| Hepatobiliary | Shows uptake of contrast agent | No uptake |
| Scar |
|
|
| Calcification | No | Frequent |
| Symptoms | No (usually incidental finding) | Symptomatic |
| Biopsy |
|
|
Hepatoblastoma
Pathologic Findings
Hepatoblastoma is a malignant tumor of hepatocyte origin that often contains mesenchymal elements. On microscopic examination, it can be classified as epithelial or mixed (epithelial-mesenchymal).
Epithelial hepatoblastoma consists of fetal or embryonal malignant hepatocytes. Mixed hepatoblastoma has both an epithelial (hepatocyte) component and a mesenchymal component consisting of primitive mesenchymal tissue and osteoid material or cartilage ( Fig. 87-23 ). This histologic classification has prognostic implications; the epithelial type, particularly if it has fetal hepatocyte predominance, has a better prognosis than the other forms. Embryonal epithelial cells are more primitive than fetal epithelial and mesenchymal cells, and tumors with this histologic type have a worse prognosis. A rare anaplastic form of hepatoblastoma has an even poorer prognosis than the mixed form of hepatoblastoma.

In gross appearance, hepatoblastoma is usually a large, well-circumscribed solitary mass that has a nodular or lobulated surface; 20% are multifocal. On cut section, the appearance varies according to the histologic type. Epithelial hepatoblastomas are more homogeneous; mixed hepatoblastomas with osteoid and cartilage have large calcifications, fibrotic bands, and overall a more heterogeneous appearance.
Incidence and Clinical Presentation
Hepatoblastoma is the most common primary liver neoplasm in childhood. It usually develops in the first 3 years of life. Although it may be present at birth or develop in adolescents and young adults, this tumor has a peak incidence between 18 and 24 months of age. Hepatoblastoma is more frequent in males than in females.
Clinically, children with hepatoblastoma present with abdominal swelling that may be accompanied by anorexia or weight loss. More rarely, children may present with precocious puberty due to secretion of gonadotropins or testosterone by the tumor. The serum α-fetoprotein level is markedly elevated in most patients. This tumor is aggressive, and lung metastases are frequently encountered at the time of diagnosis. Conditions associated with hepatoblastoma include Beckwith-Wiedemann syndrome, hemihypertrophy, familial polyposis coli, and Wilms’ tumor.
Radiologic Findings
Plain Radiography
Because hepatoblastoma is usually a large solitary tumor, a large right upper quadrant mass may be detected on plain abdominal radiographs. Extensive coarse, dense calcification is often present because of osteoid formation.
Nuclear Medicine
Hepatoblastoma appears as a large defect on sulfur colloid scans. It may take up gallium and FDG and excrete iminodiacetic acid derivative agents.
Ultrasound
On sonography, hepatoblastoma appears as an echogenic mass that may have shadowing echogenic foci corresponding to intratumor calcification. Hyperechoic or cystic areas, corresponding to hemorrhage within the tumor, or necrotic areas may be present as well. Hepatoblastoma is associated with high Doppler frequency shifts that correlate with the neovascularity typical of this tumor.
Computed Tomography
On unenhanced CT scans, hepatoblastoma appears as a solid hypodense mass, with or without calcification, that may occupy large portions of the liver. A lobulated pattern caused by bands of fibrosis can frequently be seen. Calcification and a heterogeneous appearance are particularly extensive in mixed hepatoblastoma. After intravenous administration of a contrast agent, the tumor appears hyperdense, in keeping with its hypervascular nature. In the early arterial phase, enhancement of a thick peripheral rim, corresponding to the viable portion of the tumor, may be seen. Invasion of perihepatic vessels or other structures can be demonstrated. The 3D reconstruction of helical CT data provides important information in the preoperative assessment of patients with hepatoblastoma ( Fig. 87-24 ). For example, when tumor impinges on the portal vein, the initial treatment is chemotherapy to reduce the size of the lesion. If shrinkage of the tumor away from the vessel is seen on follow-up 3D CT, surgery is indicated.

Angiography
On angiography, hepatoblastoma is hypervascular and occasionally has a “spoke-wheel” pattern, reminiscent of FNH, that is due to the presence of multiple fibrous septa and bands. Arteriovenous shunting is uncommon, and invasion of the vessels is rare. Hypovascular or avascular zones resulting from hemorrhage can occur within the tumor.
Magnetic Resonance Imaging
Hepatoblastoma is hyperintense on T2-weighted images and hypointense on T1-weighted images. Foci of high signal due to hemorrhage may be seen on T1-weighted images. On T2-weighted images, internal septa corresponding to fibrosis within the tumor appear as hypointense bands. The mixed type may demonstrate a more heterogeneous appearance on T1- and T2-weighted images because of the necrosis, hemorrhage, fibrosis, calcification, cartilage, and fibrous septa contents. After intravenous administration of gadolinium, hepatoblastoma shows immediate diffuse (homogeneous or heterogeneous) enhancement followed by a rapid washout. On the hepatocellular phase of an MR scan with hepatobiliary contrast agents, the lesion does not show uptake of the agent. MRI also demonstrates the presence of perihepatic vascular invasion. MRI can be more accurate than conventional CT in both assessing preoperative tumor extension and detecting postoperative tumor recurrence. However, CT has an important advantage over MRI in the evaluation of the pediatric abdomen; shorter scanning times result in less motion artifact, obviating the need for sedation.
Intrahepatic Cholangiocarcinoma
Pathologic Findings
Intrahepatic cholangiocarcinoma (ICAC), or adenocarcinoma of biliary duct origin, originates in the small intrahepatic ducts and represents only 10% of all cholangiocarcinomas. Hilar (Klatskin’s) and bile duct cholangiocarcinomas account for the remaining 90%.
In gross appearance, these neoplasms are large, firm masses ( Fig. 87-25 ). On cut section, they are characterized by large amounts of whitish, fibrous tissue. They rarely have internal areas of necrosis and hemorrhage.

On microscopic examination, the tumor is an adenocarcinoma with a glandular appearance and cells resembling biliary epithelium. Mucin and calcification can often be demonstrated. A large amount of desmoplastic reaction is typical of cholangiocarcinoma.
Pathologic-radiologic correlates of this lesion are given in Table 87-3 .
| Pathologic Features | Radiologic Features |
|---|---|
| Fibrosis |
|
| No necrosis or hemorrhage | Homogeneous mass: CT, ultrasound, MRI |
| Vascular encasement |
|
Incidence and Clinical Presentation
ICAC is the second most common primary hepatic malignant neoplasm in adults. It is usually seen in the seventh decade of life, and there is a slight male predominance.
Clinical signs and symptoms are related to the site of origin of the tumor. Symptoms are vague until the tumor is far advanced, and patients present with abdominal pain and a palpable mass in the upper abdomen. Jaundice is rarely a presenting symptom in ICAC, whereas it is common with hilar or ductal cholangiocarcinoma.
Radiologic Findings
Plain Radiography
On plain radiographs, ICAC may appear as a large upper abdominal mass. Calcification is frequently seen and results from mucous secretions or amorphous calcification in sclerotic areas.
Nuclear Medicine
Sulfur colloid and hepatobiliary scans demonstrate a large defect; signs of cirrhosis are present in 20% of patients with ICAC. There is no accumulation of gallium in ICAC. Red blood cell scans demonstrate a defect without late filling, reflecting the markedly hypovascular nature of this tumor.
Ultrasound
On sonograms, ICAC appears as a homogeneous mass that is usually hypoechoic. Satellite nodules may be seen. Calcified foci can be seen as high-level echoes with acoustic shadowing. Although the majority of the tumors appear slightly hyperperfused in color Doppler ultrasound studies, Doppler imaging findings vary widely. In the arterial phase of contrast-enhanced sonography, the perfusion picture of ICAC is variable but mainly hyperperfused. In the late portal venous phase, the tumor is contrasted as punched-out defects.
Computed Tomography
On unenhanced CT, this lesion usually is manifested as a homogeneous, hypodense mass. After injection of contrast material, there is early peripheral enhancement with delayed, persistent central enhancement that may take 5 to 15 minutes to be manifested ( Fig. 87-26 ). Retraction of the overlying liver capsule is a feature suggestive of ICAC. A central scar may be seen in 30% of cases. Small areas of necrosis, hemorrhage, mucin, and calcification can also be present within the tumor. Biliary dilation adjacent to the tumor is another finding seen in 20% of the cases.

Extension through the hepatic capsule and invasion of organs adjacent to the liver are common in ICAC but rare in HCC. Invasion of vascular structures around the liver is uncommon but may be seen with ICAC.
Angiography
On angiography, ICAC is predominantly hypovascular with small, thin vessels corresponding to the fibrous nature of this tumor. Encasement of hepatic arteries and other major vessels is associated with the degree of sclerosis resulting from the tumor.
Magnetic Resonance Imaging
On MRI, ICAC appears as a large mass of decreased signal intensity on T1-weighted images and increased signal on T2-weighted images. A central area of hypointensity is seen in some cases on T2-weighted images and corresponds to the central scar. The pattern of enhancement on Gd-DTPA–enhanced scans depends on the size of the lesion ( Fig. 87-27 ). Larger ICACs (>4 cm) show peripheral enhancement that progresses centripetally and spares the central scar ( Fig. 87-28 ). Smaller lesions (2-4 cm) enhance homogeneously. These patterns of enhancement may also be seen in hemangiomas. However, the degree of enhancement of hemangiomas is greater. In addition, ICACs may have other features, such as satellite nodules, invasion of the portal vein, and dilation of intrahepatic bile ducts distal to the lesion, that are not associated with hemangiomas. ICACs do not show uptake of hepatobiliary contrast agents during the hepatocellular phase scans. On diffusion-weighted imaging with increasing b values, ICACs show high signal intensity and low ADC values, indicating their malignant character.


Cystadenoma and Cystadenocarcinoma
Pathologic Findings
Biliary cystadenoma and cystadenocarcinoma are currently considered forms of the same disease, with cystadenocarcinoma being overtly malignant and cystadenoma having malignant potential. Transformation of cystadenoma to cystadenocarcinoma is a recognized complication.
On microscopic examination ( Fig. 87-29 ), cystadenomas and cystadenocarcinomas are commonly mucinous, but a serous variety is also recognized. The locules of these tumors are lined by columnar, cuboidal, or even flattened epithelium. Polypoid projections and papillary areas are frequently present. There is a well-formed wall, and focal calcification within the wall is rare. Biliary-type epithelium lines the cysts. In cystadenocarcinoma, malignant epithelial cells line the cysts. Pathologists have categorized biliary cystadenocarcinoma by whether ovarian stroma is present or absent. Cystadenocarcinoma with ovarian stroma is found in women and has an indolent course and a good prognosis, whereas tumors without ovarian stroma are found in both sexes and have an aggressive clinical course and a poor prognosis.