Almost lunchtime. Need to finish the screening board first. Could that little area on the left craniocaudal (CC) be new? I don’t see anything on the mediolateral oblique (MLO). I’ll give her a 6-month follow-up and then we’ll know if it is important or not.
This is not a good approach to asymmetries! Malignant asymmetry is often subtle and can appear identical to normal fibroglandular tissue. In one study nearly half (47%) of interval cancers that were visible in retrospect appeared as an asymmetry. If we want to detect early breast cancer, then we need to pay attention to asymmetries.
The distribution of fibroglandular tissue, ducts, and adipose tissue in the right and left breasts usually produces a fairly symmetric pattern on mammography. Asymmetry in this pattern most commonly represents normal variation, but it may also be the sole presenting sign of breast cancer.
Differentiating between the two is one of the most challenging aspects of mammographic interpretation. Careful right-to-left comparison and comparison with previous mammograms are vital in this process. Detection and analysis of asymmetric soft tissue density findings are important components of mammographic interpretation that will increase the breast cancer detection rate and provide many women with an opportunity for earlier diagnosis.
Terminology and Significance of Types
There are four types of asymmetries: global asymmetry, focal asymmetry, developing asymmetry, and one-view asymmetry ( Box 10-1 ). Differentiation between the types is important because the positive predictive value for malignancy and management differs according to type. Asymmetry may be global (diffuse) or focal (one or more areas). If an asymmetry is new compared with old mammograms, it is considered a developing asymmetry. If an asymmetry is only seen on a single projection, it is a one-view asymmetry.
- •
Global asymmetry
- •
Focal asymmetry
- •
Developing asymmetry
- •
One-view asymmetry
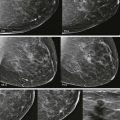
Asymmetries do not fulfill the criteria for the other soft tissue density findings described in the BI-RADS Atlas. They lack the convex borders of masses and are often interspersed with fat ( Fig. 10-1 ). They also lack the radiating lines or tissue retraction of architectural distortion (AD) and the tubular branching appearance of a dilated duct.

Global Asymmetry
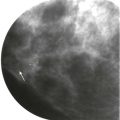
Global asymmetry is asymmetric tissue that occupies at least one breast quadrant ( Fig. 10-2 ) and is visualized on two or more projections. Global asymmetry is not uncommon; the prevalence is about 3%. Because the asymmetric tissue extends over a large region, a malignancy of this size is almost always associated with a palpable mass or other clinical abnormality.

Global asymmetry usually represents a normal variant. Therefore, provided there are no associated clinical abnormalities or suspicious changes on mammography, it is typically benign and is given BI-RADS 2 category. Global asymmetry associated with a palpable finding may indicate an underlying invasive cancer or noncalcified ductal carcinoma in situ (DCIS). When global asymmetry is encountered, it is important to ensure that the patient has had a recent clinical breast examination; when there is a corresponding palpable abnormality, the chance of malignancy increases to about 8%.
One malignant cause of global asymmetry is the “shrinking breast” that may be caused by invasive lobular carcinoma (ILC). In these cases, one breast appears smaller and denser than the contralateral side on mammography. This is not a clinical finding; the clinical examination may be underwhelming. The “shrinking breast” is discussed in more detail in Chapter 11 , Expanding the Differential Diagnosis. If the breast that is denser is also larger and associated with the clinical finding of erythema or edema, the patient may have mastitis or inflammatory breast cancer. Likewise, associated mammographic findings of increased density in one breast with AD or suspicious calcifications may be due to underlying cancer. ( Box 10-2 ).
- •
Palpable
- •
Associated breast erythema or edema
- •
Associated AD or calcifications
- •
One breast appears smaller and denser than the other (the “shrinking breast”)
Focal Asymmetry
Focal asymmetries are localized findings that have a similar shape on at least two views and occupy less than one breast quadrant (see Fig. 10-1 ); they lack the borders and conspicuity of a true mass. A finding detected at screening may be considered a focal asymmetry, but then it may be shown to be a mass on diagnostic mammography or ultrasonography (US).
Most focal asymmetries represent islands of normal tissue. Provided there are no associated clinical, mammographic, or sonographic abnormalities, then focal asymmetries on a baseline mammogram are probably benign findings (BI-RADS 3) with a less than 2% chance of malignancy. Short-term follow-up is reasonable after diagnostic evaluation.
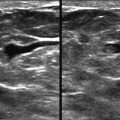
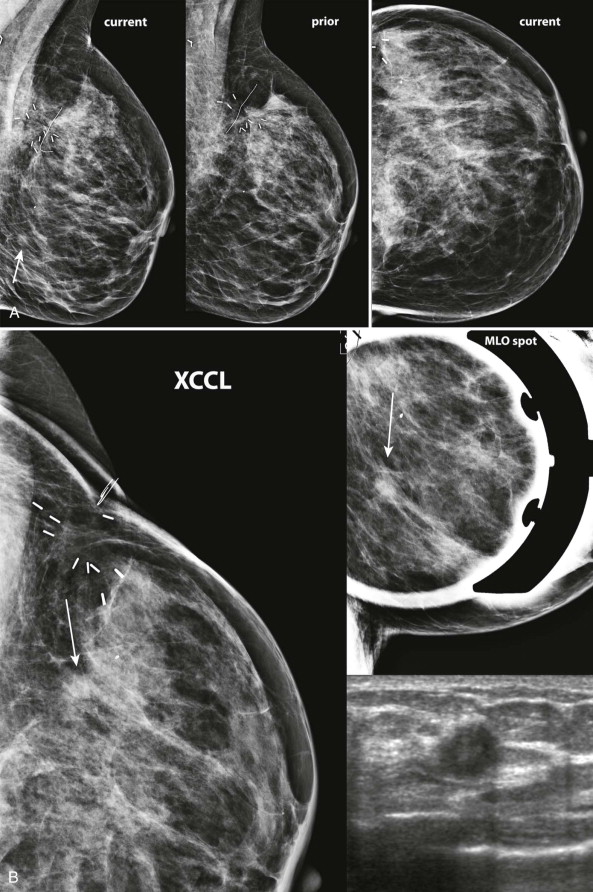
Developing Asymmetry
Developing asymmetry is a type of focal asymmetry (visualized on two or more projections) that has increased in size or density since a previous mammogram ( Figs. 10-3 and 10-4 ). It is the only type of asymmetry that, by definition, has undergone a suspicious change and it is therefore the most likely to be malignant. About 13% of developing asymmetries are malignant when detected at screening, and 27% are malignant based on diagnostic findings. Developing asymmetries detected on screening nearly always warrant diagnostic evaluation.
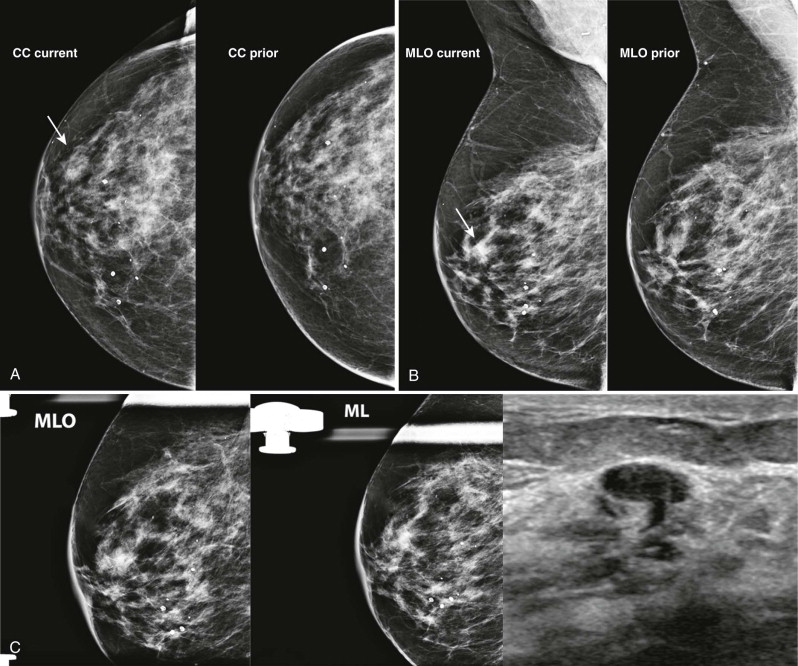
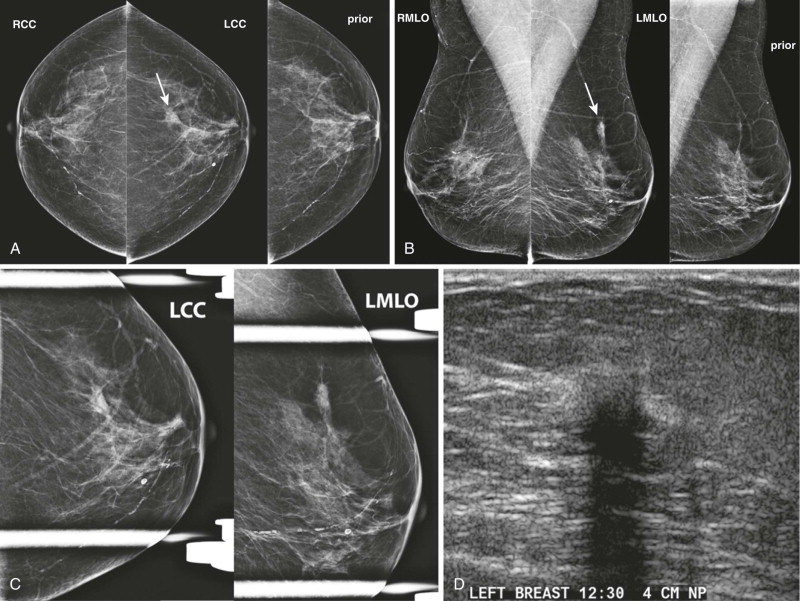
Over half of developing asymmetries are explained by summation artifact, which is resolved on diagnostic evaluation. Benign causes that may be suggested by the patient’s history include hormone-replacement therapy, trauma, surgery, and mastitis.
If a developing asymmetry persists on diagnostic views or there are suspicious findings on US, biopsy is indicated (BI-RADS 4). Importantly, US is negative in about 25% of malignant developing asymmetries, so the absence of findings on US does not justify follow-up rather than biopsy ( Box 10-3 ).
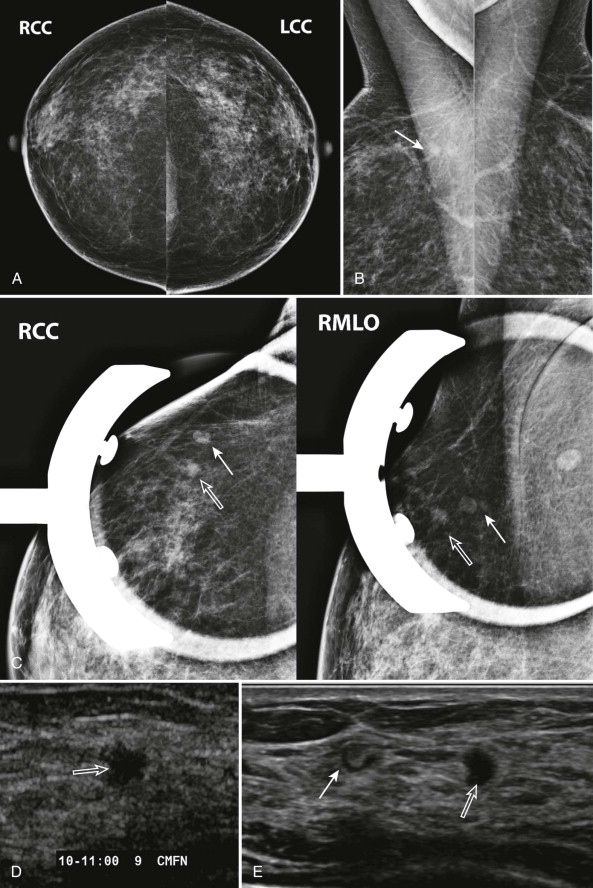
One-View Asymmetry
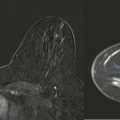
The old adage in radiology, “one view is no view,” doesn’t necessarily apply to mammographic screening. Single-view asymmetries are potential abnormalities detected in about 3% of mammograms ( Fig. 10-5 ). Fewer than 2% are found to be malignant. Most one-view asymmetries represent superimposed normal tissues (summation artifact). When asymmetries are not due to summation artifact, 10% prove to be malignant.

So how do we decide if a one-view asymmetry is important? An asymmetry that has been stable for at least several years is unlikely to be significant. If not, we need to figure out why the asymmetry is only seen in one view. An asymmetry that is in the posterior third of the breast may have been excluded from the other projection ( Fig. 10-6 ). A one-view asymmetry that is not in the posterior breast would usually have been included on the other view. In that case, the asymmetry is either due to summation artifact (see Fig. 10-5 ) or is obscured on the other view ( Fig. 10-7 ). So look at the other view closely, keeping in mind the size, density, and depth of asymmetry.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree