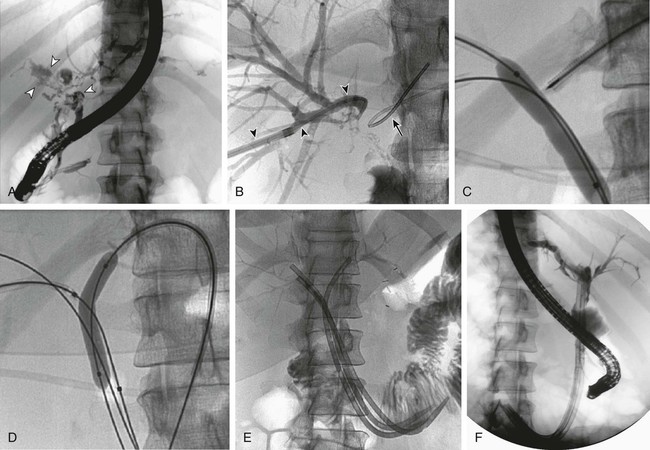
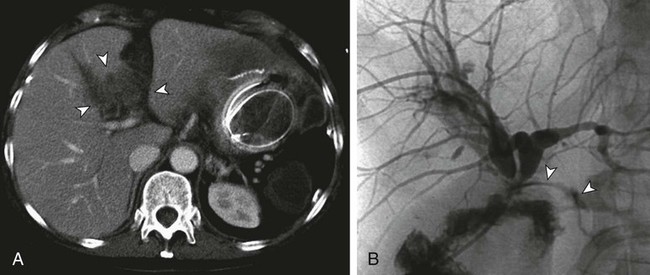
Biliary leakage is defined as diversion of bile via a defect in the ductal wall leading to the formation of bilomas, fistulas, or free spillage into the peritoneal cavity. It is a common complication after liver and biliary surgery. With emerging laparoscopic techniques and transplantation, the rate of bile leakage is reported to range from 0.8% to 12%.1–4 Massive hepatic trauma with subsequent biliary leakage has also been reported.5 Leaks can originate from biliary-enteric anastomoses, choledochocholedochostomy, bile or cystic duct stumps, cystohepatic ducts, blind-ending aberrant bile ducts (ducts of Luschka),6 intraoperative bile duct injury, or ablation of the surface of the liver, or they may be due to loose or dislocated T-tube drainage.7 Biliary anastomotic or T-tube exit site leaks attract early attention, whereas symptoms from bile duct necrosis occur relatively late3 (Fig. 136-1). Small leaks can be managed conservatively with antibiotics and maintenance of perioperatively placed drains,8 but massive biliary extravasation can result in bilomas, fistulas, or biliary peritonitis, with subsequent abscess formation and sepsis. Patients usually have localized or diffuse abdominal pain and tenderness and fever and chills. Jaundice is indicative of concomitant biliary strictures. Leukocytosis and elevated C-reactive protein levels are signs of active inflammation. Older patients, however, may lack typical symptoms. Because biliary leakage can provoke a life-threatening condition, early diagnosis and therapy are crucial. Intravenous administration of broad-spectrum antibiotics is mandatory. When bile or blood cultures are available, specific antibiotic therapy is initiated. Bilomas should be diverted percutaneously under ultrasound or computed tomography (CT) guidance or with perioperatively placed drains. Irrigation and low-pressure suction prevent stasis of fluid in a closed space and thus decrease the likelihood of infection.9,10 • Major biliary leakage unlikely to resolve spontaneously (ongoing abdominal drainage of a significant amount of bilious fluid) • Surgical therapy not necessary (definitive healing of the leakage expected after endoluminal decompression alone) • Surgical therapy impossible because of extensive tissue adhesions (previous operations) • Poor patient condition, with high anesthesiology risk • Endoscopic management not possible because of In patients with massive biliary peritonitis, surgical revision and peritoneal lavage are usually necessary. Bile duct transection or disruption requires surgical therapy as well. In contrast to the blind-ending ducts of Luschka, the cystohepatic ducts drain liver parenchyma. Thus, injuries to the cystohepatic ducts must be treated by either surgical biliary reconstruction or diversion to the jejunum.6 If surgical treatment is not necessary or impossible, endoluminal biliary drainage is indicated for persistent biliary leakage. The principle of healing a bile leak is to create a low-pressure system along the biliary tract by means of internal or external drainage. Endoscopic therapy with nasobiliary drainage, sphincterotomy, or placement of an endoprosthesis has been reported to result in a high closure rate of up to 82%.11–13 Because percutaneous transhepatic access is more invasive, endoscopic retrograde cholangiopancreatography (ERCP) is recommended as the first option. However, when the duodenum or the common bile duct cannot be cannulated, percutaneous transhepatic biliary drainage (PTBD) is the only endoluminal treatment option. PTBD serves to decompress the biliary system and redirect bile flow from the defect into the bile ducts. This may lead to sufficient healing of the leakage that additional surgery is not necessary (see Fig. 136-1). In critically ill patients, PTBD may allow the patient’s condition to improve before subsequent definitive surgery (Fig. 136-2). • Coagulopathy that cannot be corrected. Because the risk of uncontrollable hemorrhage from the liver is high in patients with coagulopathy, every effort should be made to correct or improve coagulation status before the procedure.14 • History of allergies to contrast material. During hepatic puncture for PTBD, contrast material is likely to be injected into blood vessels before a bile duct is opacified. If a patient is known to be allergic to contrast agents, cortisone and antihistamine should be used prophylactically. • 5- and 10-mL syringes; sterile swabs • Nonionic water-soluble contrast agent (300-370 mg iodine/mL) • Local anesthetic: 5 to 10 mL of 2% lidocaine; injection needles • Single-puncture technique: Neff Percutaneous Access Set (William Cook Europe, Bjaeverskov, Denmark): • Small-gauge stainless steel access needle with an inner stylet • Coaxial introducer system consisting of three parts: an outer sheath, an inner tapered introducer, and an innermost metal stiffening cannula • 0.035-inch hydrophilic Radiofocus guidewire M (Terumo Medical Corp., Tokyo, Japan) • 5F Angled Taper Glidecath (Terumo) • 0.035-inch Amplatz Extra Stiff guidewire (William Cook Europe) • 8.3F ring, Lunderquist biliary drainage catheter • 10F and 12F Munich drainage catheters (Peter Pflugbeil GmbH, Zorneding, Germany): perforated bile duct drainage with a special flange (perforation distance, 7.5, 10, or 15 cm), connecting tube, sealing cap, and adapter Biliary leakage is suspected when persistent bilious-looking effluent from the abdominal drain is noted. Injection of contrast material through the drain may result in opacification of a bile duct.15 Before PTBD, contrast-enhanced CT or magnetic resonance imaging (MRI) yields important anatomic information. Bilomas or fistulas, as well as abscesses, are especially well visualized with magnetic resonance cholangiopancreatography (MRCP),16 and the site of the bile leak may be tentatively established. Though more investigator dependent, ultrasonography is an alternative preinterventional imaging method.8 Generally, PTBD for biliary leakage is performed in similar fashion as for biliary obstruction. However, in 88% to 100% of cases, the intrahepatic bile ducts are not dilated or only minimally dilated, and hence more difficult to cannulate.5,8,15,17 The percutaneous access site is chosen according to the estimated site of leakage, because the biliary drainage catheter should finally be able to cross the injured portion of the bile duct. A single-puncture technique is acceptable for nondilated bile ducts.16 This technique requires that the initial puncture be appropriate for definitive catheter placement (Fig. 136-3
Management of Biliary Leaks
Indications
Contraindications
Equipment
Technique
Anatomy and Approach
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Radiology Key
Fastest Radiology Insight Engine