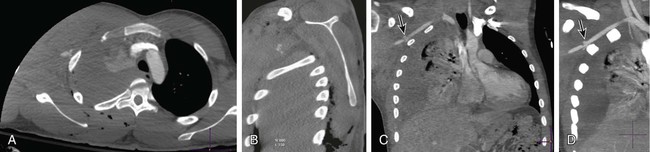
Chapter 39 Sean R. Dariushnia and Curtis A. Lewis Vascular injury has two main consequences—hemorrhage and ischemia. Or, in the words of an anonymous Czech surgeon, “Bloody vascular trauma—it’s either bleeding too much or it’s not bleeding enough.”1 Unrecognized and uncontrolled hemorrhage can rapidly lead to a trauma patient’s demise. Unrecognized and untreated ischemia can lead to limb loss, stroke, bowel necrosis, and multiple organ failure. The aim of this chapter is to highlight the fundamentals of peripheral vascular trauma and provide an approach to the diagnosis and management of vascular injury. Similarly, a reduction in the ankle-brachial pressure index in the presence of a palpable pulse does indicate the presence of a vascular injury requiring intervention. A differential in peak systolic cuff pressures between the traumatized and normal extremity predicts a significant (requiring repair) vascular injury at angiography. This was clearly demonstrated in 1993 by Schwartz and Weaver, who entered over 500 consecutive patients with isolated upper or lower extremity penetrating injury into a prospective study designed to refine the indications for diagnostic arteriography. Fourteen major injuries and 10 nonocclusive injuries were identified. Only pulse deficit (P < .01) and an ankle-brachial or wrist-brachial index less than 1.00 in the injured extremity (P < .03) were found to be significant predictors of an arterial injury.2 Doppler sonography alone, therefore, adds little to careful clinical examination. CT scanners are present in nearly every hospital. In trauma centers, 16- and 64-MDCT technology is commonplace and allows for fast image acquisition of the entire body (seconds). Routinely, if the patient presents with polytrauma and is hemodynamically stable, a head, chest, and abdomen/pelvis CT (PAN-SCAN) can be obtained. With multidetector scanners, an extremity computed tomographic angiography (CTA) examination can easily be added to the PAN-SCAN with the same contrast injection, without significantly adding to image acquisition time.3 Axial images can be viewed immediately after image acquisition and most injuries identified. Postprocessing three-dimensional (3D) reconstructions can provide an easily understandable format obtainable within minutes of the scan and can be of benefit to both the radiologist and nonradiologist clinician, especially the vascular or trauma surgeon (Fig. 39-1).
Management of Extremity Vascular Trauma
Technique
Diagnostic Tests
Doppler Ultrasonography
Computed Tomographic Angiography
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Management of Extremity Vascular Trauma