Always a rush in the morning. Time to fix lunch for the kids. Did we go grocery shopping this week? Those grapes don’t look so hot. I think they’ve been in the produce drawer too long. What about these other grapes? Oh no—they have seeds. The kids never eat those. I’d better find something else to send with my kids for lunch. There are often clues that a mass in the breast is a potential problem. Something about it doesn’t look so great.
Lawyers have been known to ask a radiologist on the stand, “Shouldn’t you do a biopsy if there is any chance of cancer?” The answer is plainly, “No.” Reading mammograms is all about the odds. What are the odds that a particular finding represents cancer? If the odds are less than 2%, then biopsy is not usually indicated.
A primary role of the radiologist is to determine the likelihood of cancer and to base management decisions according to that level of risk. Mass characteristics and change over time are the primary determinants of management. The shape and margins are important features of masses on any modality. Additional characteristics include density on mammography; echotexture, heterogeneity, and posterior acoustic features on ultrasonography (US); and enhancement pattern on magnetic resonance imaging (MRI). The management of masses is relatively straightforward once the characteristics and behavior over time are determined.
Benign Masses (BI-RADS 2)
The ability to recognize masses that are characteristically benign provides a great service to our patients. Establishing a mass as benign (BI-RADS 2) by any modality provides immediate reassurance to the patient and can spare her the anxiety and discomfort of unnecessary follow-up studies or biopsy. Certain masses—specifically, the fat-containing circumscribed masses, most cystic masses, and solid circumscribed masses that are stable for at least 2 years—are considered benign.
Fat-Containing Circumscribed Masses
On screening mammography, a circumscribed fat-containing mass is considered benign BI-RADS 2, without the need for recall. These masses are virtually always benign (BI-RADS 2). Okay, yes, it is possible that a hamartoma could have a cancer develop within its boundaries, but the odds of that are extremely small. Okay, and also a lymph node that is enlarged or has a thickened cortex could be due to metastatic disease or lymphoma/leukemia. But otherwise, fat-containing circumscribed masses are benign.
Why circumscribed? An invasive carcinoma that has engulfed fat can present as an irregular fat-containing mass, so those don’t count. A fat-containing circumscribed mass seen on screening mammography does not need recall for diagnostic imaging. BI-RADS 2 at screening is fine. In fact, if you do bring the patient back for a diagnostic evaluation and end up performing US, the odd appearance of the mass may end up prompting a biopsy recommendation.
Fat-containing circumscribed masses are no problem. There are only five types, and they are pretty easy to tell apart ( Box 7-1 ). Note that the first two masses, lipoma and oil cyst, are completely fat density with no soft tissue components on mammography. The last three have both fat and soft-tissue density and are therefore mixed radiodense and radiolucent on mammography.
- •
Lipoma
- •
Oil cyst
- •
Hamartoma
- •
Lymph node
- •
Galactocele
Lipoma
These common masses may be asymptomatic or palpable as a soft mobile mass, and they may be multiple. They are completely fat containing (radiolucent) on mammography ( Fig. 7-1 ). Occasionally, lipomas can contain central lucent-centered calcifications.

Elsewhere in the body, lipomas are hyperechoic. In the breast, however, lipomas on US are isoechoic to the fat or minimally hyperechoic (see Fig. 7-1 ). Sometimes it is difficult to tell whether a palpable lump represents a fat lobule or a lipoma. If it is just a fat lobule, the edges will blend into the next fat lobule. If it is a lipoma, rocking the transducer from side to side may demonstrate the well-defined margins. Note that fibroadenomas can also be isoechoic to fat, so correlation with mammography is important. A lipoma will be radiolucent, whereas a fibroadenoma will be radiopaque.
Oil Cyst
An oil cyst occurs when a fat lobule is devascularized and undergoes liquefaction necrosis, forming a lipid-containing mass. When an area of fat necrosis is larger than 1 cm, it is often referred to as an oil cyst. These cysts are usually due to significant trauma, such as a motor vehicle collision with seatbelt injury or an encounter with a surgeon ( Fig. 7-2 ). The rim of oil cysts often calcifies. In the acute phase, the mass may be mixed fat and soft tissue density, but will quickly evolve to fat density over a few months ( Box 7-2 ).

- •
Motor vehicle collision
- •
Reduction mammoplasty
- •
Benign surgical biopsy
- •
Lumpectomy ± radiation therapy
The US appearance of oil cysts can be quite variable ( Fig. 7-3 ). Remember that these are called oil cysts— their appearance is often similar to a fluid-filled cyst on US. The most common appearance is a round or oval circumscribed anechoic mass. Unlike fluid-filled cysts, though, oil cysts do not usually have increased through transmission and can even have some shadowing. Oil cysts can also have mixed echogenicity, mimicking a complex mass such as a papillary carcinoma. The lesions do not need aspiration or biopsy! Correlation with the mammogram is key. A papillary lesion would have to be white on the mammogram, whereas an oil cyst will be black.

In its earliest stage, fat necrosis may present as a palpable mass, often with tenderness. The patient may or may not recall trauma or bruising. The US appearance of an oval, circumscribed, very hyperechoic subcutaneous mass is quite characteristic ( Fig. 7-4 ). If you are unsure about the cause, place a radiopaque marker over the finding and do a tangential view. The finding should correspond to a circumscribed fat-containing mass. If not, then biopsy should be considered.

Lymph Node
Lymph nodes are unmistakable with their C-shaped cortex and central fat. Intramammary lymph nodes may require recall with spot compression views or even US if the fatty hilum is not visualized on a screening mammogram. Lymph nodes with an abnormal appearance, such as loss of the fatty hilum, enlargement, rounding, or focal or diffuse cortical thickening, should be considered suspicious, however, because these may contain metastatic deposits or lymphoma.
Galactocele
These masses are seen exclusively in women who are lactating or are late in pregnancy ( Fig. 7-5 ). Galactocele literally means “milk cyst,” which explains why this finding is included with the fat-containing masses. Human milk has a very high fat content. The fatty component will rise above the solids. That said, the fat-fluid line of a galactocele is rarely sharp. It is more common that there are bubbles of fat at the superior aspect of the mass on mammography.

On US, galactoceles have mixed echogenicity. The contents often shift during scanning, similar to a complicated cyst.
Hamartoma
Let’s say that you have found a mixed-density circumscribed mass on mammography. Because is it not completely radiolucent, it is not a lipoma or an oil cyst. It doesn’t look like a lymph node, and the patients’ not pregnant or lactating. Of the five fat-containing circumscribed masses, that leaves only hamartoma. Occasionally, acute fat necrosis that has not yet formed a perfect oil cyst can appear as a mixed-density fat-containing mass on mammography. However, there is usually a history of trauma to help make that diagnosis.
Hamartomas are congenital masses with mixed fat and soft-tissue density and circumscribed margins ( Fig. 7-6 ). The soft-tissue component is often slightly strange looking—a little denser than the rest of the tissue and perhaps slightly distorted. Think of a hamartoma as a fat and soft-tissue mass in which the components have been slightly swirled. Our eyes tend to rest on the odd appearing white soft-tissue component and do not always recognize the surrounding fat and capsule. Reviewing many cases of hamartomas will train your eye to spot them easily as they are an Aunt Minnie.

On US, hamartomas can also appear somewhat bizarre. Hyperechoic breast tissue is mixed with hypoechoic fat ( Fig. 7-7 ).

Benign Cystic Masses
There are four types of cystic masses in the breast: simple, clustered microcysts, complicated, and complex ( Box 7-3 ). Simple cysts, clustered microcysts, and most complicated cysts are benign. Complex masses have a moderate risk of malignancy.
- •
Simple cyst
- •
Clustered microcysts
- •
Complicated cyst (includes hemorrhagic cysts)
- •
Complex mass
The mammographic appearance of cystic masses is typically a round or oval, circumscribed, low- or equal-density mass. The margins may also be obscured on mammography, or the mass may be palpable but occult on mammography.
Simple Cysts
The cysts should have imperceptible walls, be completely anechoic (a little reverberation artifact is fine), and demonstrate posterior acoustic enhancement ( Fig. 7-8 ). They may be multiple and wax and wane in size. Obviously a simple cyst needs no further intervention (BI-RADS 2). Or does it? What if she is 72 years old, not on hormones, and develops a new simple cyst? It’s still okay! The ACRIN 6666 Screening US trial found that 39% of postmenopausal women had simple breast cysts. Aspiration is not indicated unless the patient requests it because of pain. Routine screening is all that is needed (even if the mass is palpable).

On MRI, benign cysts may occasionally have a thin rim of enhancement around a T2 hyperintense mass ( Fig. 7-9 ). This is a normal finding, and aspiration or biopsy is not necessary.

Clustered Microcysts
These microcysts are a common, benign variant of simple cysts ( Fig. 7-10 ). They are essentially a lobule that is expanded with fluid. Think of them as a bunch of grapes. It’s really hard to take a good picture of them on US because some of the microcysts will be in the scan plane and others will not. At real time US, each of the microcysts should be otherwise simple.

Of 203 women with clustered microcysts across four series, one cancer was detected, for an overall incidence of 0.5%. Clustered microcysts are BI-RADS 2, even in postmenopausal women. Just like simple cysts, microcysts may correspond to a new mammographic finding and are still BI-RADS 2. However, we need to look really closely. They should look like grapes that you would send with your child to school. If it looks like the grapes have been in your produce drawer too long—and you know what we mean—they have ill-defined margins, or if they look like grapes with seeds (which your children are not going to eat anyway), then biopsy should be considered. If the grapes have gone bad, they are no longer considered clustered microcysts but a complex cystic mass.
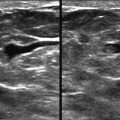
Complicated Cysts
These cysts contain diffuse low level echoes. If the echoes are seen swirling around inside the cyst or layer at real time US, then you know that it is a complicated cyst and not a solid mass ( Figs. 7-11 and 7-12 ). As long as the wall is thin, these cysts are typically BI-RADS 2.


Differentiating a complicated cyst with low level echoes that are not moving from a solid mass can be very challenging ( Fig. 7-13 ). If blood flow is present within the mass, then it is solid. However, the absence of blood flow by Doppler interrogation does not exclude a solid mass. These masses must be assumed solid and managed as such. If the mass corresponds to a new or enlarging mass on mammography, then biopsy should be considered. An attempt can first be made to aspirate the lesion, followed by core biopsy if fluid is not obtained.

The risk of malignancy is very low for complicated cysts. Nearly all of them are benign. Four cancers were detected in seven series that included a total of 1343 patients with complicated cysts for an overall cancer incidence of 0.3%. When these are identified in a background of other simple cysts, BI-RADS 2 is reasonable. However, a solitary complicated cyst on a first study may be considered BI-RADS 3. Aspiration may be indicated for a new or enlarging complicated cyst (BI-RADS 4), particularly if it is a solitary finding or high-density appearance on mammography.
Hemorrhagic Cyst
These cysts are also included in the category of complicated cysts. Hemorrhagic cysts have a very distinctive appearance ( Fig. 7-14 ). They look like the yin-yang symbol. These often occur following cyst aspiration. A small clot develops on the anterior wall and appears solid. These can be confused with complex masses. The solid clot, however, has a broad base along the wall rather than being exophytic within the cyst.

Do you see these a lot in your practice? If so, then you have someone who is aspirating the fluid out of cysts. This is easy to change. After aspiration, injection of air into the cyst will considerably lower the chance of recurrence of the cyst. If you inject an equal or slightly smaller volume of room air into a cyst following aspiration, the likelihood of recurrence is only about 15% compared with 80% if you simply remove the fluid.
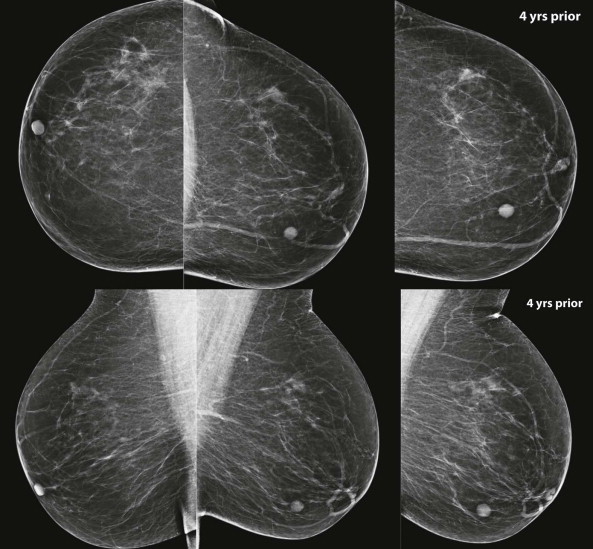
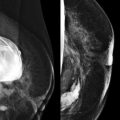
Stable Solid Mass with Benign Features
Benign features for a solid mass include a round or oval shape, circumscribed margins, low or equal density on mammography ( Fig. 7-15 ), and homogeneously hypoechoic with a parallel orientation on US. Benign features on MRI include smooth margin, oval or round shape, homogenous persistent enhancement, nonenhancing septations, and T2 hyperintensity ( Fig. 7-16 ).