Unruptured intracranial aneurysms (UIAs) are common and are being detected with increasing frequency given the improved quality and higher frequency of cross-sectional imaging. The long-term natural history of UIAs remains poorly understood. To date, there is relative lack of clear guidelines for selection of patients with UIAs for treatment. Surveillance imaging for untreated UIAs is frequently performed, but frequency, duration, and modality of surveillance imaging need clearer guidelines. The authors review the current evidence on prevalence, natural history, role of treatment, and surveillance and screening imaging and highlight the areas for further research.
Key points
- •
Unruptured intracranial aneurysms are common and are being more frequently diagnosed.
- •
Surveillance imaging plays an important role in the follow-up of untreated aneurysms, but further research is needed to define the optimal frequency and duration of imaging.
- •
Consistent, standardized reporting of criteria for growth/change in aneurysms on surveillance imaging is important.
Introduction
Unruptured intracranial aneurysms (UIAs) are common and most often detected between the fourth and sixth decade of life. More than 30% of patients with UIAs may harbor more than 1 aneurysm. There have been significant improvements in detection/imaging surveillance as well as treatment of intracranial aneurysms (IAs). However, preventive treatment (endovascular or surgical repair) has inherent risks of complications, recurrence, and need for follow-up and possible re-treatment. The proportion of UIAs that rupture is not known, but rupture is thought to occur in only 1 out of 200 to 400 patients per year. Conservative management without surveillance imaging carries the risk of aneurysm rupture and subarachnoid hemorrhage (SAH), which is associated with poor patient outcomes. , The utility of surveillance imaging depends on its ability to detect early changes in aneurysm, which accurately reflect the risk of rupture, and subsequent treatment mitigating rupture and improving patient outcomes. , Despite advancements in knowledge, the dilemma regarding optimal management of UIAs persists. In this review, the authors discuss the available evidence regarding prevalence of UIAs, risk factors, role of imaging in surveillance, and screening of UIAs and treatment.
Epidemiology, clinical presentation, and risk factors
The incidence rate for unruptured aneurysms is not known because of a lack of prospective, long-term follow-up studies in populations at risk, and the prevalence depends on the population studied, reason for imaging, and method of detection. Based on a 2011 meta-analysis on 94,912 patients in 83 studies, the overall prevalence was thought to be 3.2% (95% confidence interval [CI], 1.9–5.2) in a population without comorbidity with mean age of 50 years. However, subsequent studies have reported a prevalence of 6% to 7%, with a recent analysis on computed tomography angiographies (CTAs) from acute stroke patients reporting a prevalence of 11.4%. , UIAs are more common in women, smokers, and patients with hypertension, although limited data are available regarding impact of risk factor modification on occurrence of UIAs. , Prevalence studies show an increasing frequency of UIAs with age, with peak in the fifth and sixth decade. Pediatric cases are usually associated with other underlying conditions or genetic risks.
Small aneurysms are the ones most frequently detected, uncommonly cause aneurysmal symptoms, and are frequently labeled as incidental or asymptomatic. The 2011 meta-analysis reported 66% of UIAs were smaller than 5 mm. In a more recent 2016 study on screening asymptomatic patients, 87.5% of UIAs detected were smaller than 5 mm. In the absence of hemorrhage, the most common indication for diagnostic imaging leading to detection of a UIA is headache. However, most headaches in patients with UIAs are not directly related to the aneurysm.
Risk factors for growth and rupture
Risk factors in UIAs may be patient specific, such as younger age, history of prior SAH, family history of UIA or SAH, female sex, smoking, hypertension, and underlying conditions, such as autosomal dominant polycystic kidney disease (ADPKD). Aneurysm-specific risk factors are aneurysm size, morphology, location (anterior communicating artery [ACom], posterior communicating artery [PCom], and posterior circulation), and aneurysmal growth on serial imaging. ,
Aneurysm size (maximum diameter from center of the neck plane to the aneurysm dome) is one of the most important predictors of rupture. The International Study of Unruptured Intracranial Aneurysm trial reported a negligible annual risk of rupture in aneurysms less than 7 mm in size, with increasing rupture risks for larger aneurysms. The large, prospective Unruptured Cerebral Aneurysm Study in Japan study also showed increasing annual risk of rupture with increasing size of aneurysm, as well as location in the anterior or posterior communicating arteries and aneurysms with daughter sacs. A 1.09-fold increase in risk of growth has been reported for every 1-mm increase in initial size (95% CI, 1.04–1.15). However, many of the ruptured aneurysms seen in clinical practice are small (<5 mm) and may account for nearly 30% cases. Size of UIAs, if dichotomized at the cutoff value of 7 mm, seems to be an unreliable surrogate predictor of future rupture. UIAs less than 7 mm are also not a homogeneous group, with growth and rupture risks being significantly smaller in less than 3- and less than 5-mm aneurysms compared with larger UIAs.
Irregular morphology has been shown to be strongly associated with rupture in aneurysms of all sizes and independent of location. Multilobulated aneurysms, aneurysms with daughter sac, and single sac with irregular margins have all been reported to be significant predictors of rupture. “Lobulation” is defined as “a protuberance arising directly from the primary neck of the aneurysm or from the main body and representing 25% or more of the apparent volume of the main sac.” Irregularly shaped aneurysms have a risk ratio of 2.32 (95% CI, 1.46–3.68) for aneurysm growth. Aneurysms with daughter sacs or lobulations may have a 14.7% growth rate per year. Higher Aspect Ratio (ratio of size to neck diameter), Bottleneck factor (dome width to neck width), size ratio (ratio of aneurysm size to parent vessel diameter), and straighter inflow angle have all been shown to predict rupture. , For small UIAs, the size ratio and not the absolute size may highly predict the risk of rupture.
Most studies reporting on role of morphology and aneurysm geometry on rupture risk are based on showing morphologic differences between cohorts of ruptured and unruptured aneurysms. However, there is an assumption that postrupture morphology is not significantly different from that before rupture. Recent studies have raised concern that postrupture morphology should not be considered an adequate surrogate for the prerupture morphology in the evaluation of rupture risk. Hemodynamic characteristics can also be altered by geometric changes during or just after rupture and therefore should be used with caution in case-control studies comparing ruptured with unruptured aneurysms.
Most risk factors for aneurysm growth are consistent with risk factors for rupture. Based on a meta-analysis of 21 studies, the overall proportion of growing aneurysms has been reported to be 3.0% per aneurysm-year (95% CI, 2.0%–4.0%). Rupture rate of 3.1% per year is reported in growing aneurysms compared with 0.1% per year for stable aneurysms. A higher rate of growth is reported in larger aneurysms, up to 9.7% per year in aneurysms greater than 10 mm compared with 2.9% per year in aneurysms less than 10 mm size. Current American Heart Association/American Stroke Association (AHA/ASA) guidelines recommend offering treatment to patients with documented enlargement of aneurysms in the absence of prohibitive comorbidities (Class I; Level of Evidence B).
Imaging for evaluation of aneurysmal change
Saccular aneurysms less than 7 mm in the anterior circulation in low-risk locations may be managed conservatively with imaging follow-up. Surveillance imaging is performed in aneurysms to evaluate change in size or morphology, which indicates a higher risk for rupture. The choice of imaging modality, the frequency, and the duration of imaging has to be appropriate for early and accurate detection of change. However, because of the absence of long-term studies on natural history of UIAs, these are not currently well defined.
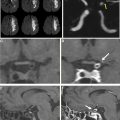
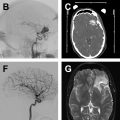
There is lack of literature on accuracy of imaging in detection of subtle changes in size/morphology, which is especially critical for small aneurysms where subtle changes must be above the spatial resolution of imaging method used to define growth. Some studies assessing serial magnetic resonance angiography (MRA) to evaluate enlargement excluded UIAs less than 2 mm in diameter, as they were considered beyond the capabilities of MRA. A recent study assessed 3-dimensional (3D) black-blood MR imaging, 3D time-of-flight (TOF)-MRA, and contrast-enhanced (CE) MRA and found all three to have excellent interreader reliability. However, all aneurysms included in the study were larger than 7 mm. Some studies assessed the first and last imaging of each patient in a single session by the same researcher to avoid interobserver variability and to minimize intraobserver variability.
There is significant variability between studies with regards to definition of aneurysm growth. , In a meta-analysis of 26 studies on UIAs less than 7 mm, 5 studies used CTA, 5 used MRA, and 9 used CTA, MRA, or digital subtraction angiography (DSA) for surveillance imaging. Only 16/26 studies used consistent, periodic follow-up to assess growth. Five of the 16 studies did not define criteria for enlargement. Only 8 studies defined enlargement clearly, with considerable variability in definition of growth.
It has been postulated that risk of rupture may be higher shortly after diagnosis of UIA and may decline with time. However, there is lack of specific literature on the dynamic growth pattern of aneurysms. Aneurysm growth may be an irregular and discontinuous process, and growth at follow-up may not be a sign of instability at the time of imaging. A decrease in the risk of rupture has been postulated after 5 years. However, in the only long-term study of natural history of UIAs, Juvela and colleagues found the risk of rupture to be virtually constant during the first 25 years after diagnosis except for patients above 50 years.
Although growing aneurysms are at higher risk for rupture, published studies are heterogeneous in terms of correlation between growth and rupture. In the SUAVe (Small Unruptured Intracranial Aneurysm Verification) study, of 480 UIAs 5 mm and smaller followed for a mean of 41.0 months, 30 grew and 7 ruptured, and only 4 of the ruptured aneurysms were growing. Bor and colleagues reported 2 ruptures in 403 UIAs 7 mm or smaller, both in nonenlarging aneurysms; none of the 37 growing aneurysms ruptured.
Irregular morphology is predictive of higher rupture risk, and risk of rupture might increase according to extent of morphologic change. However, definition of aneurysm morphology is not standardized and is subject to interobserver variation.
Risk prediction scores
Based on 6 prospective studies, the PHASES risk score ( Table 1 ) was proposed to predict risk of rupture based on location, size, age, race, history of rupture, and hypertension. The imaging criterion included in the PHASES score is size of aneurysm, with a risk score of 0 assigned to aneurysms less than 7 mm in size. The ELAPSS score has been proposed for prediction of risk of growth in UIAs and includes shape of aneurysm in addition to size as a risk predictor. The ELAPSS score also gives a differential score for aneurysms smaller than 7 mm with 0 points only ascribed to aneurysms less than 3.0 mm in size.
| PHASES Rupture Risk Score | Points |
|---|---|
| P: Population | |
| North American, European (other than Finnish) | 0 |
| Japanese | 3 |
| Finnish | 5 |
| H: Hypertension | |
| No | 0 |
| Yes | 1 |
| A: Age | |
| <70 y | 0 |
| ≥70 y | 1 |
| S: Size of aneurysm | |
| 7.0 m | 0 |
| 7.0–9.9 mm | 3 |
| 10.0–19.9 mm | 6 |
| ≥20.0 mm | 10 |
| E: Earlier SAH from another aneurysm | |
| No | 0 |
| Yes | 1 |
| S: Site of aneurysm | |
| ICA | 0 |
| MCA | 2 |
| ACA/PCom/Posterior | 4 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree