MANDIBLE AND MAXILLA: ODONTOGENIC TUMORS AND CYSTS
KEY POINTS
- Computed tomography can be highly specific in the diagnosis of mandibular masses given an organized approach that considers both odontogenic and nonodontogenic tumors and cysts.
- The mandible is much more likely to be involved by most of these tumors and cysts than the maxilla.
- Cystic varieties of these lesions without an identifiable matrix often cannot be distinguished from one another.
- Enucleation and curettage is suitable definitive therapy for few of these lesions, and precise imaging is required for medical decision making if a gross bony margin must be recommended for adequate surgical management.
- In malignant forms of these tumors, imaging should include an assessment of perineural spread and sometimes regional lymph node spread and distant disease even though those risks tend to be low.
JAW MASSES: AN ODONTOGENIC VERSUS NONODONTOGENIC ORGANIZATIONAL FRAMEWORK
Mandibular and maxillary masses generally arise from the region of the dental arches and are best separated into those of odontogenic origin, considered in this chapter, and nonodontogenic (Chapter 100) origin. This organizes not only the approach to differential considerations but also the clinical decision making process.
The odontogenic lesions may then be divided into cystic and solid groups. Cysts may be acquired or developmental. The solid group may demonstrate a mineralizing matrix. Tumors and cysts of odontogenic origin may come from one of several cell lines that contribute to the formation of the tooth. These include the cells of the enamel, pulp, cementum, epithelium of the dental lamina, and fibrous and bony elements. Strictly fibro-osseous and osteoid-origin lesions are discussed in general in Chapters 38 and 40.
Most developmental cysts and tumors of the jaws are much more common in the mandible and most commonly associated with the molar region. Outside of the molars, the canines are the next most common teeth of origin.
General Patterns of Disease
The general growth patterns and imaging appearance of primary bone tumors are discussed in detail in Chapters 38 through 42. Fibro-osseous conditions are discussed in Chapter 40, and bone cysts are discussed in Chapter 41. The odontogenic tumors and cysts discussed here share many of the growth characteristics of these other tumors.
In general, odontogenic cysts and tumors will range from a unilocular “cystic expansile” appearance to a multilocular, septated mass sometimes with an identifiable mineralized matrix. The odontogenic lesions tend to have a narrow zone of transition and bulge rather than infiltrate into surrounding tissues; thus, their basic appearance suggests a lesion of low biologic activity. This accurately reflects the behavior of the majority of these lesions. In fact, a more aggressive appearance will typically push the differential diagnosis to a nonodontogenic gamut. Malignant and aggressive forms of these tumors do occur, with perhaps the most important being the juvenile aggressive ossifying fibroma since its growth potential may be underestimated.
These tumors have a relatively low propensity for intratumoral regressive changes such as hemorrhage and necrosis. When malignant, they will tend to recur locally without a strong tendency to produce regional lymph node disease or manifest perineural spread or distant metastases.
The developmental lesions must be distinguished from the acquired inflammatory cysts. These inflammatory cysts are typically periapical and in communication with a diseased tooth root.
SPECIFIC TYPES OF TUMORS AND CYSTS: DIFFERENTIAL FEATURES, IMAGING APPEARANCE, AND TREATMENT CONSIDERATIONS
Acquired Cysts
Periapical or radicular cysts surround a tooth root or may persist as a residual cyst after removal of the tooth remnant. They are mainly the acquired result of periapical inflammatory disease. These cysts arise from the rests of epithelial cells in the periodontal ligament, undergoing cystic degeneration when the tooth becomes nonvital (Fig. 99.1). Acquired cysts may also be posttraumatic (Fig. 100.7). While the majority of these lesions are diagnosed from plain dental x-rays, computed tomography (CT) techniques show the extent of periapical cysts and other changes more precisely than plain films. More importantly, CT may show tracts to the lingual and buccal cortex as a sign of early breach of the cortex in a periapical abscess (Chapter 97). However, if the cyst is not inflammatory, such a tract can be a clue to the dental and developmental nature of the cyst. Acquired cysts may heal following root canal surgery, leaving a sclerotic remnant; healing may take up to 1 or 2 years. Some adjacent reactive bone sclerosis may be present in the marrow space around the cyst in the absence of healing.
Non–contrast-enhanced T2-weighted magnetic resonance (MR) is a very sensitive test for detecting periapical fluid collections. Marrow space edema may reflect the inflammatory nature of the cyst. Highly proteinaceous collections and granulation tissue will have more complex patterns of signal intensity than simple periapical cysts on T1- and T20-weighted images.
Contrast-enhanced MR will show the periapical collection to enhance due to active inflammation; this may be caused by granulation tissue and/or a more acute inflammatory response.
The natural history and pathologic implications of these apical cysts and granulomas are discussed in Chapter 97.
Dentigerous Cyst
Dentigerous cysts, also referred to as follicular cysts, arise from lining cells of the tooth bud or normal dental follicle. They form around the crown of an unerupted tooth, often causing tooth displacement. These cysts can sometimes cause root resorption and expand the cortical plates (Fig. 99.2). They are unilocular typically with a very thin sclerotic margin. The margin may become focally dehiscent but generally is retained within the periosteum. The cysts may bulge beyond the limits of the mandible but will not invade surrounding soft tissues. They will have morphologic features similar to a simple bone cyst on CT and magnetic resonance imaging (MRI).
Dentigerous cysts are the second most common cysts in the jaws, with periapical cysts being the first. They are commonly associated with unerupted third molar and supernumerary teeth.
KERATOCYSTIC ODONTOGENIC TUMOR
The World Health Organization (WHO) has reclassified this cystic lesion from the former odontogenic keratocyst (OKC) to the current keratocystic odontogenic tumor (KOT). It may present as a uni- or multicystic odontogenic tumor.
KOTs arise from squamous epidermal elements of the tooth bud (dental lamina) with characteristic lining of parakeratinized stratified squamous epithelium. They typically splay the tooth roots as a unilocular mass with a very thin sclerotic margin (Fig. 99.3). Internal septa may be present, giving the lesion a multilocular appearance. The margin may become focally dehiscent. The tumors may bulge beyond the limits of the mandible but will not invade surrounding soft tissues. They will have morphologic features similar to an epidermoid cyst on CT and MRI.
These tumors are most commonly associated with the posterior body of the mandible or within the ramus. The epicenter of these lesions is usually superior to the inferior alveolar nerve canal. They appear similar to a dentigerous cyst on routine imaging. However, they tend to extend along the internal cortices instead of expanding them like the dentigerous cyst. They can reach a considerable size before detection, sometimes occupying the entire mandibular ramus. KOTs have a propensity for recurrence if treated with simple enucleation and curettage, and some form of peripheral ostectomy, either mechanical or chemical, is recommended.
Multiple KOTs may be associated with Gorlin Goltz syndrome or blue rubber bleb nevus syndrome (Fig. 99.3).
Globulomaxillary and Other “Fissural” Cysts
There is continuous controversy about the origin of these epithelial cysts. These may be epithelial remnants trapped during facial development, or of dental origin. The globulomaxillary variety, when the term is applied, arises in the premaxilla between the lateral incisor and canine. It is currently explained as either a lateral periodontal cyst, radicular cyst, or KOT.
Solid Odontogenic Tumors
Ameloblastoma
Ameloblastomas are a true neoplasm of odontogenic epithelium. These solid tumors arise from the enamel elements of the tooth and are locally aggressive but benign histologically, representing approximately 10% of all odontogenic tumors. They may originate from remnants of the dental lamina and dental organ. Subtypes include solid/multicystic, desmoplastic, and unicystic (Fig. 99.3).
These tumors usually appear as a relatively large multilocular mass at the time of presentation since they do not typically produce pain. They have a predilection in males, more so in blacks between the ages of 20 to 50 years of age; 80% are found within the molar/ramus areas. Those discovered incidentally, usually by routine dental x-rays, may be small and unilocular. An ameloblastoma will have a very thin cortical margin that is often focally dehiscent. It usually will bulge well beyond the limits of the mandible and will invade surrounding soft tissues. The tumor does not have a mineralizing matrix, although there is a fibrous variant that tends to be less locally aggressive (Fig. 99.4G).
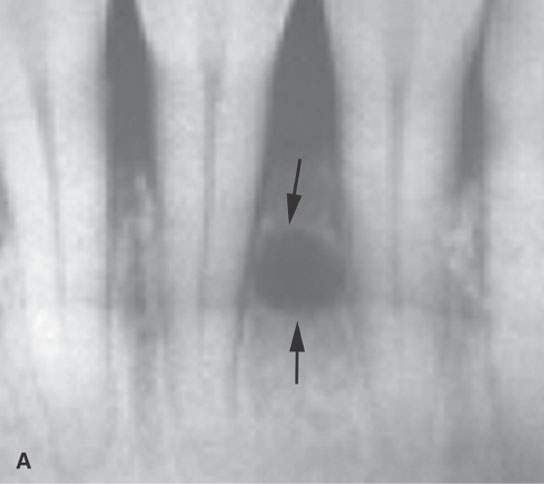
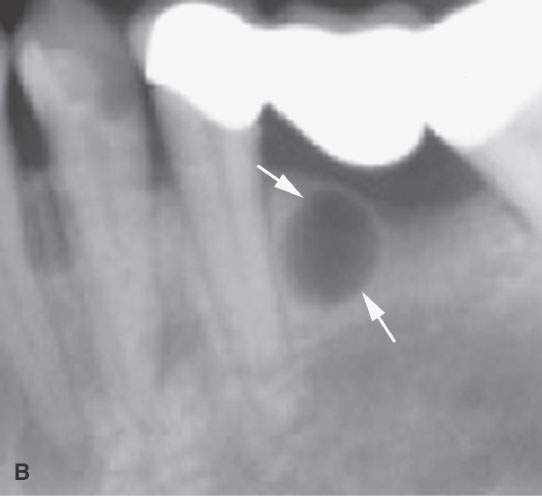
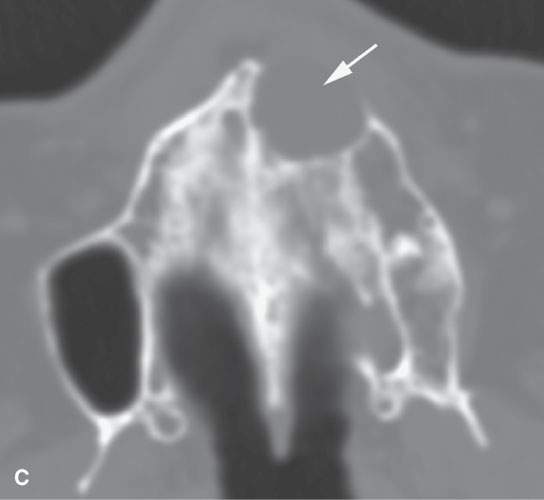
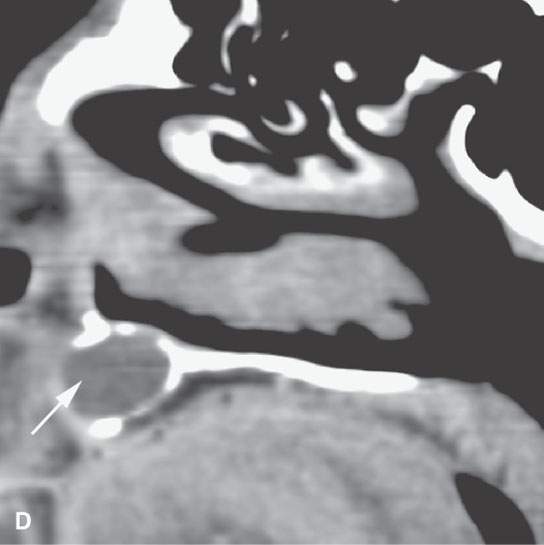
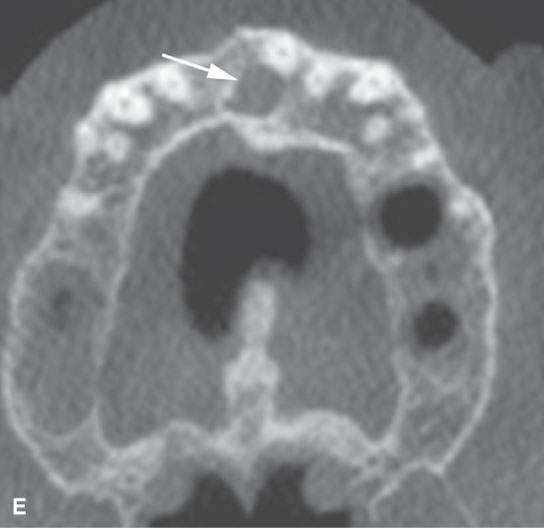
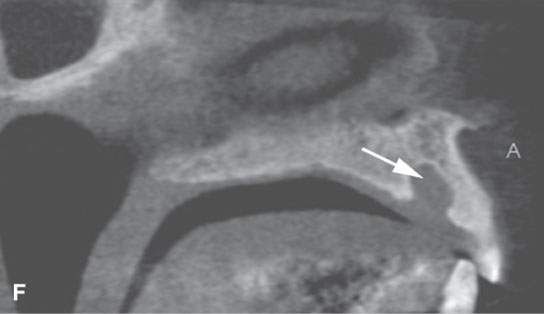

FIGURE 99.1. Various dental cysts. A: Dental views of a lateral periodontal cyst (arrows). These are believed to rise from the periodontal ligament. B: Plain films showing a residual cyst (arrows). C, D: A cyst arising between the lateral incisor and canine in the premaxilla (arrows). This type of cyst is still sometimes referred to as a globulomaxillary cyst. There is ongoing controversy about whether such cysts are about dental origin or developmental epithelial cysts not related to the teeth. Current thinking favors dental origin. E, F: A small cyst of the nasopalatine canal. G: A large cyst of the nasopalatine canal.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








