MANDIBLE: INTRODUCTION AND GENERAL PRINCIPLES
TECHNICAL ASPECTS
General Examination Technique
The entire mandible must be imaged even, for instance, if the temporomandibular joint (TMJ) is the only stated clinical area of interest. Treatment planning will almost always have to take into account the occlusal plane as well as the integrity of the entire mandible and its relationship to the maxilla and skull base attachment at the coronoid fossa.
Mandibular computed tomography (CT), cone beam volume computed tomography (CBVCT), and magnetic resonance imaging (MRI) must include the axial and off-axial acquisition and/or viewing as a routine. Multidetector computed tomography (MDCT) and CBVCT have made it simple to obtain a volume data set that can be routinely reconstructed as well as viewed with multiplanar reformation (MPR) tools (Figs. 96.1 and 96.2).
Any study of the mandible and facial region must be viewed and/or filmed in both soft tissue and bone windows. Other extracranial pathology may present with mandibular dysfunction, and either mandibular or other extracranial disease may extend intracranially. The soft tissues, including the brain, are not adequately evaluated when viewed on images done with a bone algorithm. This is a major shortcoming of CBVCT (Fig. 96.1H) since its low-contrast resolution is inherently very poor, thereby rendering its use primarily for osseous and dental structures of the maxillofacial complex.
Standard MDCT data sets should be obtained with 0.50- to 0.75-mm sections. Contrast is used with CT depending on specific indications. The most common applications of CT for uncomplicated mandibular and facial studies are done without intravenous contrast unless central osseous disease is suspected of soft tissue invasion. Specific CT protocols are presented in Appendix A.
CBVCT data can be acquired at voxel resolutions of up to 80 mm for limited fields of view. Most CBVCT units offer isotropic voxel dimensions ranging from 125 to 400 mm. MPR tools can be used to reconstruct two-dimensional slices at desired thicknesses ranging from the lowest possible voxel dimension offered to any desired level (0.125 mm to >100 mm) (Fig. 96.1F,G). Acquisition times range from 10 to 40 seconds using a pulsed or continuous exposure. The radiation burden is significantly lower compared to conventional CT. Metallic artifacts are significantly reduced in the reconstructions.
MRI should be done with 3-mm sections and a field of view of 12 to 16 cm. All three orthogonal planes might be obtained, but axials and coronals usually suffice. T1- and T2-weighted images must be obtained, preferably in both planes. Fat suppression by frequency-selective techniques may be used but are predictably and severely degraded by susceptibility artifacts along the dental arches when unremovable dental hardware or restorations are present (Figs. 1.3, 1.4, and 3.1 and Chapters 1 and 3). Non–fat-suppressed T1- and T2-weighted images before and after contrast are a safer choice, although the examination becomes lengthened. Intravenous contrast is used in most cases. Magnetic resonance (MR) protocols are presented in Appendix B.
Pros and Cons
MDCT, CBVCT, and MRI are used for the advanced imaging of the mandible and facial region (Table 4.1). Plain films including panoramic and intraoral dental images remain a standard starting point for the study of the body of the mandible, dentoalveolar processes, and teeth. Advanced imaging studies are reserved for more complex clinical decision making. Kinematic studies are possible on 320 MDCT units.
MRI has essentially replaced arthrography for evaluating internal derangements of the TMJ. Kinematic studies of the articular disk are possible. It is used only adjunctively in other mandibular problems.
Ultrasound has essentially no role in primarily mandibular pathology; however, there have been some initial attempts at utilizing ultrasound for the TMJ complex with mixed results.
Angiography is used occasionally in both diagnosis and treatment settings. Catheter angiography remains necessary if angioarchitecture and temporal flow dynamics of a lesion are in question. If not, CT and/or MR angiography will usually suffice.
Radionuclide studies, particularly single photon emission computed tomography (SPECT) gallium and 99mTc bone scans, are useful in selected cases of infectious disease or facial/mandibular asymmetry such as temporomandibular condyle hyperplasia. Fluorine-18 2-fluoro-2-deoxy-D-glucose positron emission tomography (FDG-PET) is assuming some role in infectious diseases. Specific radionuclide technique depends on the indications; those are discussed in Chapter 5 and other specific relevant chapters.
Specific Areas of Interest
Developmental Abnormalities
Developmental abnormalities are studied primarily with CT because bone detail is critical to diagnosis and three-dimensional (3D) planning or craniofacial reconstruction. However, soft tissue algorithms with less beam hardening are best for 3D stereolithic model productions. These studies require CT to be done with as good a volumetric data set as possible at reasonable dose limits with little to no patient movement. Additionally, CBVCT data that are now being utilized in dentistry, including oral and maxillofacial surgery, orthodontics, periodontics, and oral and maxillofacial radiology, may now be utilized in specialized stand-alone software specific for their individual specialty needs.
MR may be used to look for associated brain anomalies or for concerns of intracranial extension or associations of congenital anomalies, especially when these are syndromic.


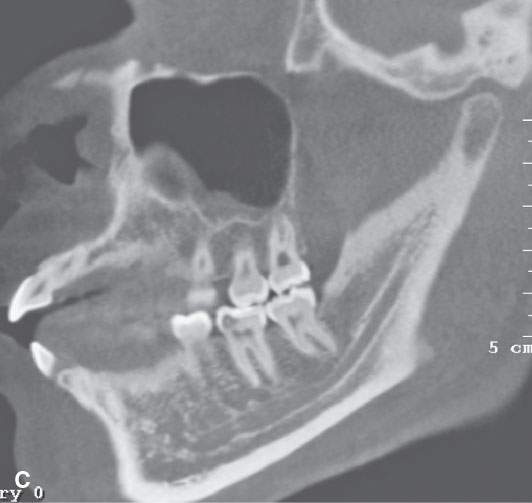
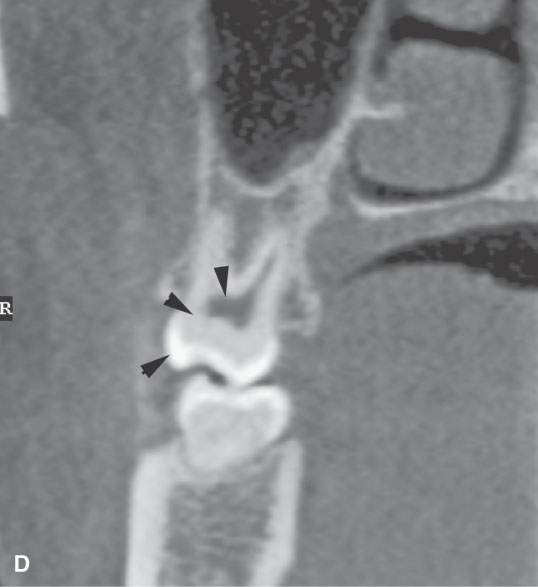
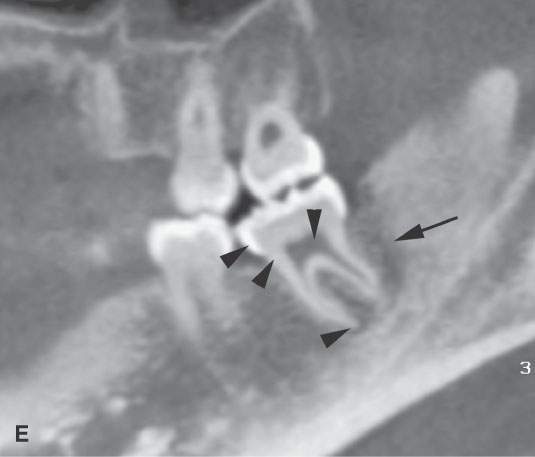

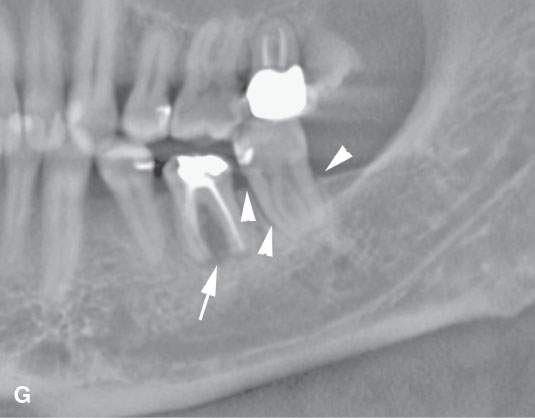
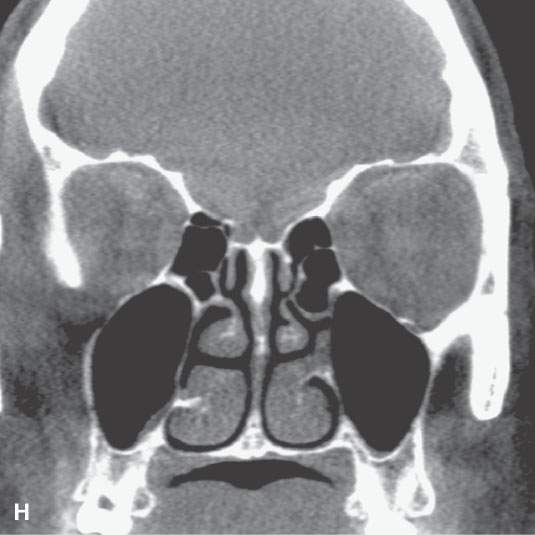

FIGURE 96.1. Images made with standard cone beam volume computed tomography (CBVCT). A: Axial image through the maxillary alveolar ridge showing the standard detail related to dentition and mandibular detail for comparison with other techniques as seen in this and some of the following figures. B: CBVCT can produce reasonable images of the sinuses as long as soft tissue detail is not at a premium. C: Sagittal reformatted images to demonstrate a level of detail of the dentition and the mandible are available from standard CBVCT. D, E: Magnified views of reformatted images showing reasonable detail related to dentition anatomy (the crown, dentin, pulp cavity, root detail are shown by arrowheads) and dental disease provided by this technique (periodontal disease is shown by arrows). F: High-resolution CBVCT to compare with (A) through (E). G: A magnified view from (F) showing excellent bone detail as demonstrated by the ability of this technique to detect relatively minor changes associated with periodontal disease (arrowheads) and rarifying changes around the tooth with extensive endodontal disease (arrow). H: The major disadvantage of CBVCT is the relatively poor soft tissue or low-contrast resolution. Evaluation of the brain and orbital soft tissues is simply unreliable with this technique, and a definitive statement about those soft tissues is rarely possible. This is important since sometimes diseases within the soft tissues only will present with oral and maxillofacial types of complaints and may go unnoticed on CBVCT studies. I: An example of the type of three-dimensional reconstructions that are possible from high-resolution CBVCT studies. Such images can be used can be planning complex reconstructions.
Inflammatory Disease
The evaluation of infectious and noninfectious inflammatory mandibular disease still often begins with plain films. Some patients with persistent, and especially worsening, symptoms after a course of conservative management requiring imaging will get a CT. Means of complying with reducing radiation exposure, such as CBVCT data volumes, should be considered in pediatric screening studies and multiple recurring CT examinations that may be required for certain postoperative follow-ups. Such indications might include maxillomandibular reconstructions, dental implants, and ongoing orthodontic therapy. CBVCT doses typically are ≤50% in comparison with MDCT studies, a factor producing increasing interest in CBVCT’s applications. Starburst artifacts are minimal and not as disruptive as an additional benefit (Fig. 96.1F,G).
The techniques used in the evaluation of patients who are potential candidates for major craniofacial reconstruction, possibly with allograft planning, require a high-resolution volume acquisition (Fig. 96.1I). Such a study must be done in compliance with equipment used for image-guided surgery if serving surgeons using such guidance systems. Such protocols are outlined in Appendix A.
Complex inflammatory cases posing a risk for associated abscess should be studied with standard MDCT during infusion of intravenous contrast (Appendix A).
Tumor
Patients with benign and malignant tumors often present with signs and symptoms identical to those of dental inflammatory disease; therefore, these patients usually have had at least dental-type plain films, non–contrast-enhanced CT, or CBVCT by the time a tumor is confirmed by biopsy. A supplemental MRI may be useful. The MR in these cases is usually focused on clarifying specific issues that may critically alter patient management, such as the extent of extramandibular involvement and presence and extent of perineural spread. MRI or CT may be most appropriate for follow-up of treated cancers; however, with MRI, early bone invasion as a sign of recurrence or persistence may go unnoticed.
If MRI, CT, or the clinical evaluation suggests a vasoformative lesion or highly vascular tumor, angiography may be done to confirm this impression. In hypervascular lesions, embolotherapy may be used as a definitive treatment or adjunct to surgical removal. This possibility must be resolved before any dental procedure is initiated.
Trauma
CT has replaced plain films for evaluating patients at risk or with complex injuries. These CT studies are done with volume acquisition and MPR viewing.
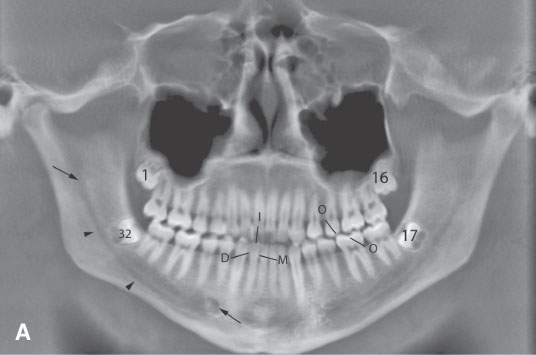
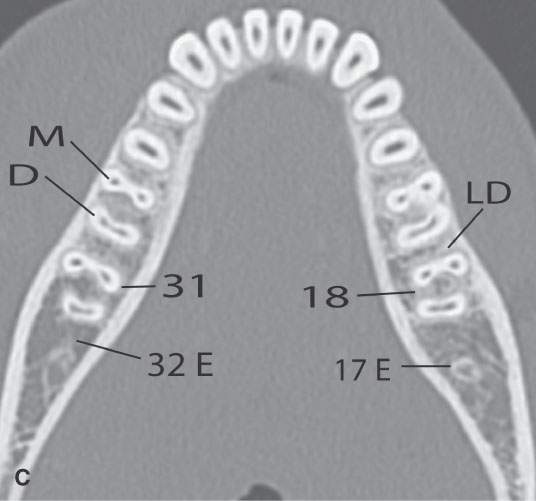
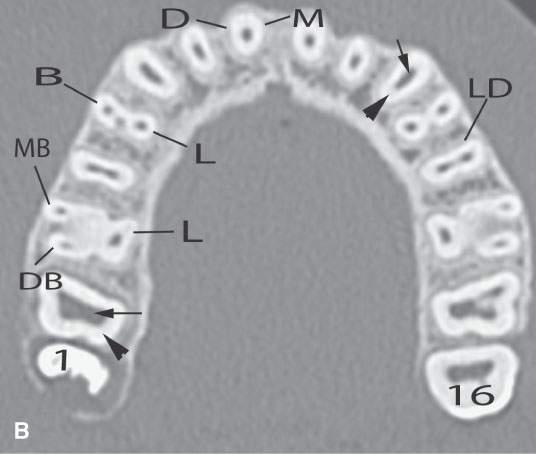

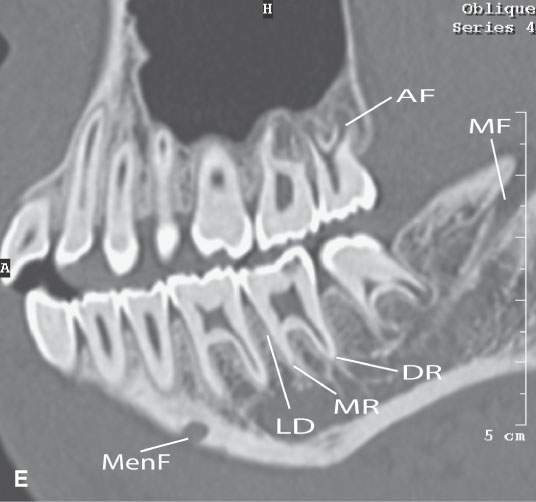
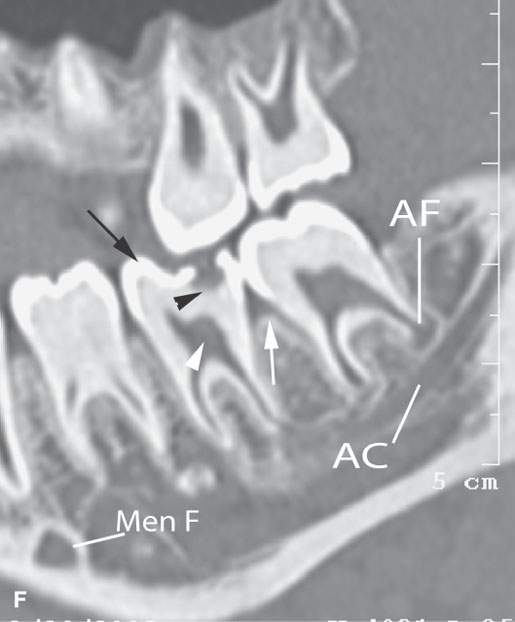
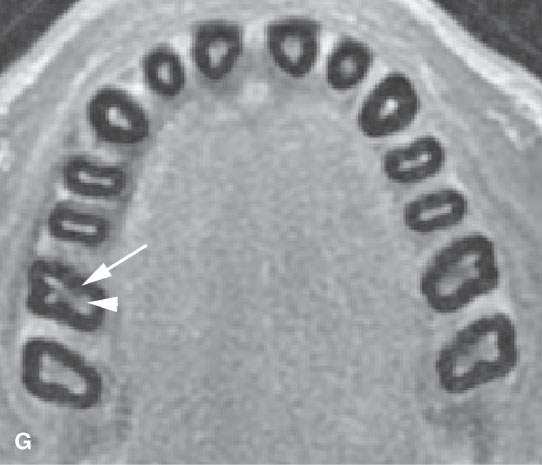

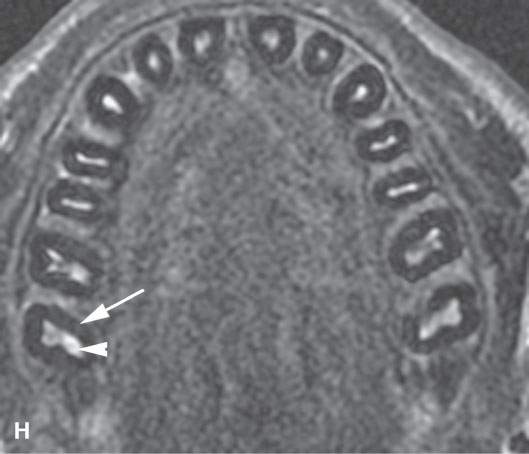
FIGURE 96.2. A series of images meant to illustrate the naming and organization of the dentition in addition to some other anatomic features of the mandible. A: Cone beam volume computed tomography panoramic view showing how the teeth are numbered from 1 to 32. This also illustrates how the anterior and posterior surfaces are designated. Anterior teeth have incisal (I), distal (D), and mesial (M) surfaces. Posterior teeth have similar surfaces except at the top of the tooth is designated as its occlusal (O) surface. Note the position of the inferior alveolar canal (arrowheads) from the mandibular foramen to the mental foramen (arrows). B, C: High-resolution computed tomography (CT) examination of the maxilla and mandible. Note the manner in which the upper teeth are numbered—1 to 16 from right to left. The numbering is continued in the mandible as indicated from left to right. Note that the third molars in the mandible have been extracted and are referred to as 32E and 17E, and numbering is continued from there as designated by the numbers 18 and 31. The remainder of the lettering demonstrates the designation of the surfaces of the teeth and other related structures as follows: D, distal; M, mesial; B, buccal; L, lingual; MB, mesiobuccal; DB, distobuccal; and LD, lamina dura. Also note the pulp cavity (arrows) and its relationship to the surrounding dentin (arrowheads). D: Coronal CT reformations illustrating the anatomy of the teeth. Structures of the tooth are designated as follows: C, crown; D, dentin; PC, pulp cavity; RC, root canal; and A, root apex. The horizontal line designates the occlusal plane (OP). Also note the lamina dura (LD) surrounding the tooth socket. E: Sagittal CT reformations further illustrating mandibular and dental anatomic detail. The anatomy of the molar teeth includes a mesial and distal root (DR and MR); each tooth root has an apical foramen (AF). Note the lamina dura around the designated second molar (LD). The mental foramen (MF) is the point of entry of the inferior alveolar nerve to the mandible, with its main branch exiting at the mental foramen (Men F). F: A more magnified view of the same patient seen in (E). The crown of the second molar (arrow) is interrupted by a cavity (black arrowhead) that has not completely penetrated the dentin to involve the pulp cavity (white arrow). Bone loss of periodontal disease is present between the second and third molar (arrow). Note the very close relationship between the apical foramen of the third molar (AF) and the inferior alveolar canal (AC). G: T1-weighted magnetic resonance study showing the relatively low signal intensity of the dentin (arrow) surrounding the higher signal intensity of the pulp cavity (arrowhead). H: T2-weighted image of the same patient seen in (G) demonstrating the dentin (arrow) versus pulp cavity signal intensities. I: A defect along the lingual cortex related to this rooted tooth is a normal variant called a furcation and should not be mistaken for pathologic bone loss.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








