MANDIBULAR TRAUMA: BLUNT-FORCE FRACTURES AND PENETRATING INJURIES
KEY POINTS
- The imaging findings in mandibular trauma are critical to treatment decisions, including precise surgical planning.
- Imaging can identify findings that are critical to prognosis.
- Imaging can help detect important complications such as infection, retained foreign bodies, or airway compromise.
Blunt-force and penetrating trauma may result in both soft tissue and bony injury. This chapter describes common patterns of mandibular fractures. Facial fractures that are primarily of the orbit are discussed in Chapter 63, and other facial fractures are discussed in Chapter 88. This chapter also discusses the effects of penetrating trauma and the evaluation of possibly retained foreign bodies. Vascular malformations due to facial trauma are discussed in Chapter 59.
ANATOMIC AND DEVELOPMENTAL CONSIDERATIONS
Applied Anatomy
The relevant mandibular anatomy is discussed in Chapter 96 and that of the temporomandibular joint (TMJ) is discussed in Chapter 101. The mandibular anatomy must be understood to properly describe and classify fractures. Proper classification leads to proper consideration of treatment options.
Three paired vertical midface buttresses have an effect on the patterns of facial injury and strategy of repair (Chapter 88). Functionally, these buttresses support the face against the vertical forces of mastication, and understanding them is relevant to this consideration of mandibular injury. A weaker midline buttress, the frontoethmoidal-vomerine, supports the midline. The horizontal buttresses are relatively frail compared to the three main vertical buttresses. These include the superior alveolar ridges, palate, and inferior orbital rims. The latter have much to do with the integrity of the occlusal plane.
IMAGING APPROACH
Techniques and Relevant Aspects
The mandible and maxilla are studied with computed tomography (CT) and magnetic resonance (MR) techniques described in detail in Chapter 78. Specific CT protocols by indications are detailed in Appendix A. Specific MR protocols by indications are outlined in Appendix B.
Almost all studies to investigate facial trauma are done without contrast except if an infectious complication or vascular malformation is suspected. In cases of more complex maxillofacial/mandible “smash” or gunshot trauma, three-dimensional CT postprocessing may be helpful for surgical orientation. Cone beam volume computed tomography (CBVCT) may be very useful in planning complex reconstructions at a savings of radiation dose to the patient.
Pros and Cons
CT is done routinely for the evaluation of facial and sinonasal injury and typically is sufficient for all medical decision making. Emergent evaluation with CT is indicated for possible associated tension orbit. Magnetic resonance imaging (MRI) is used occasionally to assess optic nerve compromise (Chapter 54).
MR is used adjunctively in highly selected cases of penetrating trauma with possibly retained foreign bodies and in those complicated by infection that might result in intracranial complications (Fig. 63.19).
Plain films may be used to confirm proper gross placement of components of constructs but have essentially little if any definitive primary role if CT is available except for panoramic imaging for mandibular injuries. Dental images may be employed for teeth injuries and alveolar fractures.
SPECIFIC DISEASE/CONDITION
Blunt-Force Trauma and Mandibular Fractures
Etiology
Acute trauma to the mandible may be caused by blunt force or be penetrating from a wide variety of untoward events but are mainly due to motor vehicle crashes, fighting, and sports. Mandibular fractures are uncommon in children. Both mechanisms of injury can also occur during surgery and may result in the presence of retained foreign bodies. The chronic effects of mandibular trauma due to those mechanisms are also discussed in following sections.
Clinical Presentation
Fractures may present with only soft tissue trauma or a hematoma. Facial deformity, either visible or palpable, suggests fractures. Mandibular fractures are associated with an array of signs and symptoms including localized pain, trismus, deformity, dental malocclusion, paresthesias and dysesthesias, and lost teeth. Associated midface and cervical spine injuries are relatively common in high-energy incidents such as motor vehicle crashes. Associated retained foreign bodies may be suggested by the physical examination or circumstance of the injury.
Fracture Patterns and Classification
Fractures may be closed, open, simple, compound (including fractures that communicate through the periodontium), comminuted, greenstick, pathologic, atrophic, and impacted or telescoped. Highly complex fractures may result in significant soft tissue damage. More than one fracture is commonly present, with injuries often being bilateral.
Fractures most typically involve the body, ramus, and angle of the mandible (Figs. 98.1–98.7). The ramus and coronoid process are relatively infrequent sites of injury (Fig. 98.1). This anatomic distribution is the primary means of classification of fractures. The anatomic classification is rounded out by the terms symphyseal fractures, those within the bounds of the central incisors and parasymphyseal, those within the bounds of the canines (Figs. 98.2 and 98.3). Alveolar process fractures involve may or may not involve the tooth sockets.
Additional classification is by “favorable” and “unfavorable” in the vertical and horizontal vectors based on fracture orientation to the pulls of the muscles in the masticator space (Figs. 98.3A and 98.5). An unfavorable fracture is one in which the natural pull of the involved muscles tends to displace the fracture, while a favorable fracture is one in which the involved muscles tend to reduce the fracture. For example, the digastric, genioglossus, and geniohyoid muscles of the floor of the mouth can exert unfavorable forces on symphyseal-region fractures. This concept is not used typically to describe a fracture, although it may be incorporated into imaging reports. It does, however, illustrate how precise imaging data contributes to management decisions.
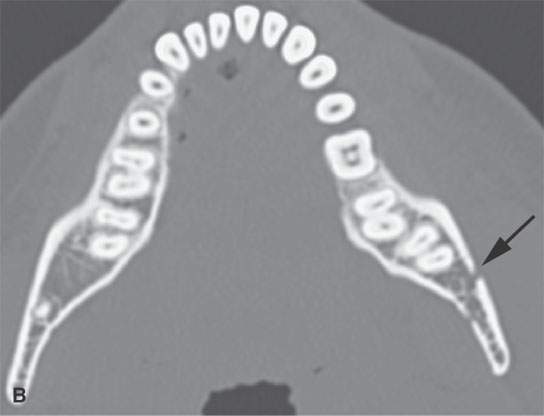
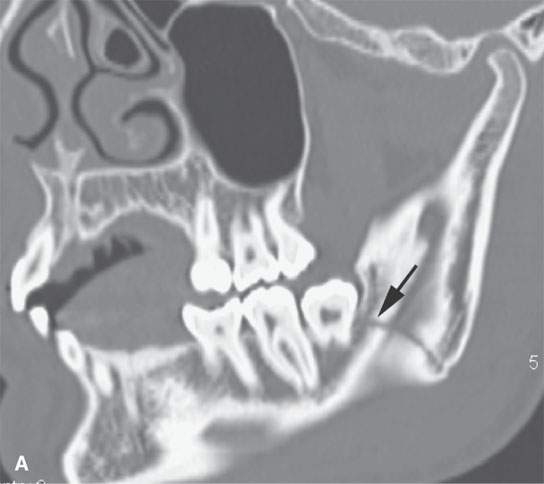
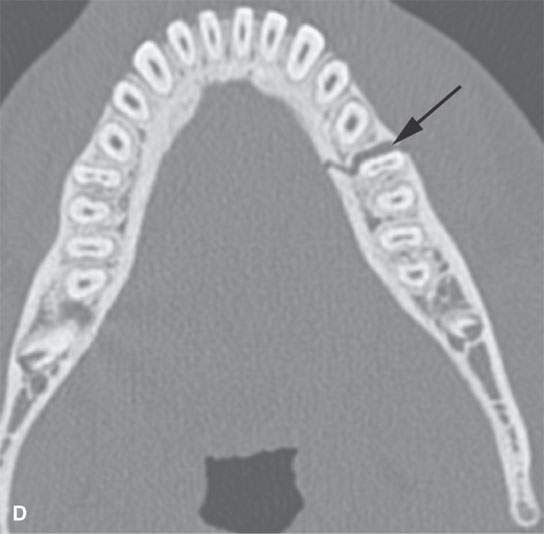
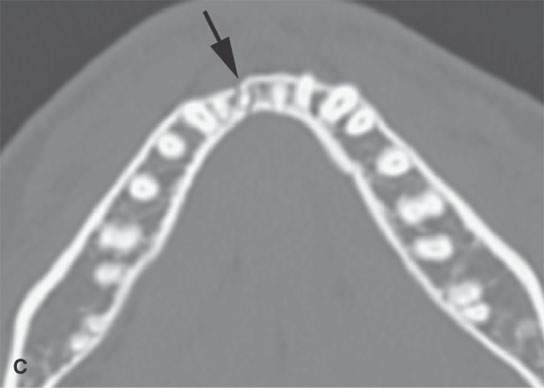
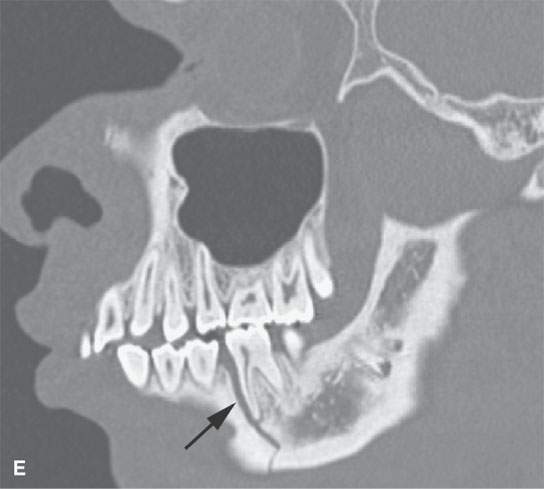
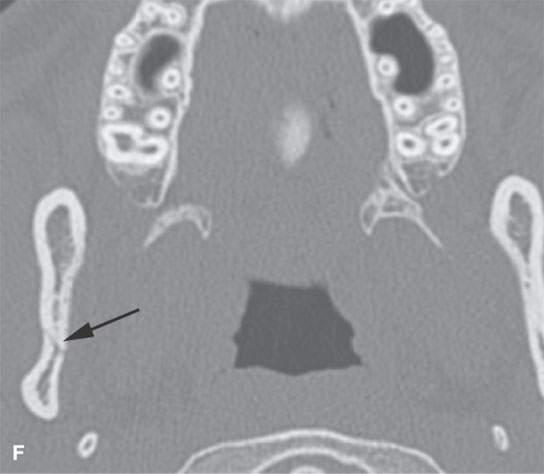
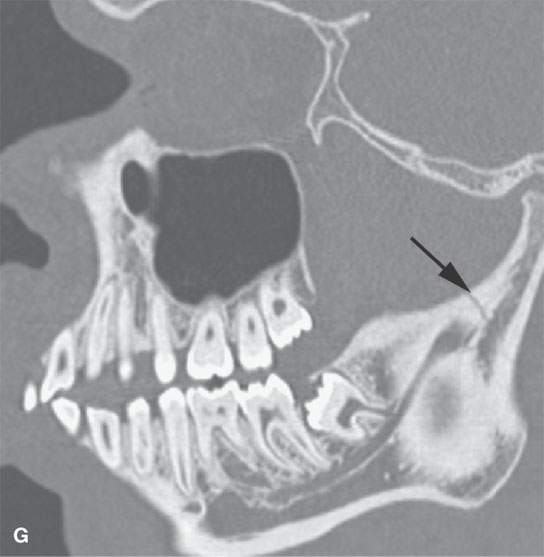

FIGURE 98.1. Three patients with fractures of the angle and ramus of the mandible. A–C: Patient 1. In (A), the sagittal reformation shows the oblique fracture line entering the last molar tooth socket (arrow). In (B), the axial section shows the nondisplaced fracture continuing in the condyle (arrow). In (C), a second fracture involves the right central incisor (arrow). D–G: Patient 2. A mandibular fracture through the body of the mandible. In (D), the axial image shows that the fracture enters the first molar tooth socket (arrow) but appears to spare the root. (continued) In (E), the sagittal reformation confirms that the fracture has not interrupted the tooth root (arrow). In (F), an additional subtle nondisplaced fracture of the contralateral ascending ramus at its junction with the condyle is present (arrow). In (G), the subcondylar fracture in its entirety (arrow) is shown. H: Patient 3. A mandibular fracture studied with a panoramic view shows a fracture similar to Patient 2 involving the canine tooth socket. The socket is involved, but the root has not been injured. The tooth was saved.
There are five subtypes of condylar fractures sometimes described with regard to management issues; however, it is sufficient to describe them as extracapsular, intracapsular, or subcondylar as well as with regard to their degree of displacement (Figs. 98.2A and 98.4).
Mandibular fractures, especially in children, may be buckled or “greenstick” rather than frankly fractured (Fig. 98.4F,G). These may result from relatively minor trauma and tend to have a lesser association with complications than fractures in adults.
Other facial injuries are fairly common, especially in motor vehicle crashes.
Pathologic fractures will occur with less than the usual amount of energy expected to cause such injury and may be the presenting event of the pathologic process (Fig. 98.8).
Delayed Complications
Long-term complications of mandibular fractures may result in significant cosmetic deficits, mandibular dysfunction, and chronic pain (Figs. 98.9 and 98.10). Non- or partial union, infection, construct failure, inadequate restoration of occlusion, and secondary TMJ dysfunction account for most of the complications. TMJ dysfunction may be mechanical or due to osteonecrosis or accelerated degenerative changes (Fig. 98.10). Posttraumatic cysts may occur due to intramedullary bleeding much as described for the hematic and subperiosteal cyst of the orbit and face (Chapters 41 and 88).
Neuralgia-inducing cavitary osteonecrosis is associated with iatrogenic causes rather than blunt-force trauma (Chapters 43 and 97); however, injuries to the inferior alveolar nerve may also occur and produce neuralgia.
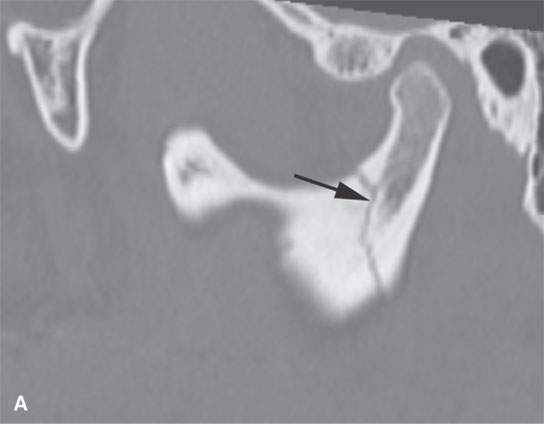

FIGURE 98.2. Mandibular fractures as shown in Figure 98.1 are frequently multiple. Figure 98.1 shows a tendency for multiple fractures to involve both sides of the mandible. In (A), a subcondylar fracture is present; in (B), an ipsilateral fracture involves the parasymphyseal region (arrows).
Manifestations and Findings
Plain Film and Fluoroscopy
Plain films may be used as guide during and just after surgery to grossly check the adequacy of reduction and treatment results (Fig. 98.10).

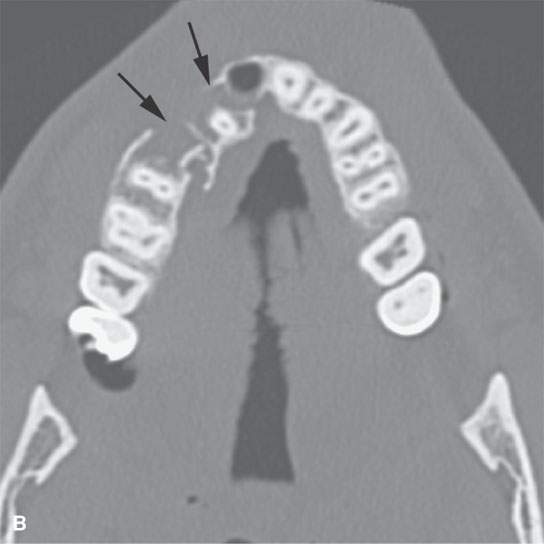


FIGURE 98.3. A patient with a symphyseal fracture with a complicating hard palate injury. A: Fractures involving the central and lateral incisors with significant posterior displacement and comminution (arrows). B: Similar injury is present involving the maxillary alveolus with obviously missing teeth (arrows). C: The hard palate is fractured, presenting an added challenge in planning the repair that will have to include intermaxillary fixation. D: The full extent of the hard palate injury (arrows).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








