Mediastinitis refers to a focal or diffuse inflammation of the tissues located in the mediastinum. The mediastinum lies between the right and left pleural cavities and extends from the thoracic inlet to the diaphragm. Mediastinitis can be classified into acute and chronic forms. Acute mediastinitis is usually a catastrophic disorder manifesting with a sudden and dramatic onset and a high mortality rate when the diagnosis is delayed. The chronic forms of mediastinitis (fibrosing mediastinitis) comprise a spectrum of disease ranging from active granulomatous inflammation to “burned-out” mediastinal fibrosis.
There are infectious and noninfectious causes of mediastinitis. Mediastinal infection occurs through direct contamination and hematogenous or lymphatic spread or extension from the head, neck, lung, pleura, chest wall, or peritoneum. The clinical presentation is variable, depending on the chronicity of the underlying process. Acute mediastinitis is usually caused by bacteria, and chronic mediastinitis is most often related to tuberculous or fungal infections.
Acute Mediastinitis
Etiology, Prevalence, and Epidemiology
Acute mediastinitis may be classified, on the basis of its cause, as being postoperative, secondary to esophageal perforation, a result of the spread of osteomyelitis from adjacent bone, a direct extension of head and neck infection, or a result of hematogenous spread of infection. Acute mediastinitis is a potentially life-threatening condition that necessitates aggressive surgical intervention, drainage of the mediastinum, and aggressive therapy with broad-spectrum parenterally administered antibiotics. The mortality ranges from 10% to 20% to 40% to 50% and increases drastically with delay in diagnosis and treatment.
The most common cause (90%) of acute mediastinitis is iatrogenic esophageal perforation during diagnostic or therapeutic endoscopic procedures ( Box 76.1 ). Esophageal perforation is an uncommon and life-threatening event that occurs more frequently in association with the use of endoscopic instruments and surgical thoracic procedures. This complication has been reported in about 1 per 1000 patients who undergo endoscopic examinations. The mortality associated with acute mediastinitis from esophageal disruption is 5% to 30%, even with appropriate treatment. Perforation has been described after rigid esophagoscopy, dilatation of a stricture, pneumatic dilatation for achalasia, after variceal sclerosis, and esophageal tube placement (nasogastric and Sengstaken-Blakemore). In one review of 114 cases of esophageal rupture, the cause was iatrogenic in 55%. Esophageal perforation may also occur in association with a necrotic esophageal carcinoma, radiation esophagitis, and ulceration of a hiatal hernia. Outcome after esophageal perforation is dependent on the cause and location of the injury, the presence of underlying esophageal disease, and the interval between injury and initiation of treatment. Late complications of acute mediastinitis resulting from esophageal perforation include esophagocutaneous, esophagopleural, and esophagobronchial fistulas.
Perforation or rupture of esophagus
- •
Iatrogenic: diagnostic or therapeutic endoscopic procedures, sclerotherapy of esophageal varices, surgery
- •
Spontaneous: Boerhaave syndrome, labor, asthmatic attack
- •
Direct penetrating or blunt trauma
- •
Impacted foreign body
- •
Erosion: caustic ingestion, esophageal carcinoma, necrotizing infection, radiation esophagitis
- •
Perforation or rupture of airways
- •
Direct penetrating or blunt trauma
- •
Iatrogenic: intubation, bronchoscopy
- •
Foreign body
- •
Broncholithiasis
- •
Erosion: bronchogenic carcinoma
- •
Perforation of vessels
- •
Iatrogenic: indwelling central venous catheters
- •
Direct extension
- •
Adjacent tissues: oropharyngeal infections, periodontal tissues, paraspinous abscess, retroperitoneal and subphrenic infection
- •
Anterior chest wall: drug abuse, closed-chest cardiopulmonary resuscitation
- •
Retroperitoneum: pancreatitis
- •
Infection
- •
Tuberculosis
- •
Postsurgical
- •
Cardiothoracic surgery, esophageal surgery
- •
Primary
- •
Inhalational anthrax: hemorrhagic mediastinitis
- •
Infectious mediastinitis also may occur after major airways perforation secondary to trauma or instrumentation. Other causes of acute mediastinitis include odontogenic infections, perforation of the superior vena cava (SVC) by a central venous catheter, and the leakage of parenteral nutrition from a migrated central venous catheter.
Postoperative acute mediastinitis occurs in 0.5% to 5% of patients who underwent median sternotomy for cardiothoracic surgery. Nearly 700,000 median sternotomies are performed each year in the United States, leading to approximately 8300 deep sternal wound infections. The risk of infection is increased in obesity, insulin-dependent diabetes, internal mammary artery grafting (especially bilaterally), and reoperation. Commonly isolated organisms are Staphylococcus epidermidis and Staphylococcus aureus , various gram-negative organisms, fungi, and atypical mycobacteria.
Boerhaave syndrome refers to spontaneous esophageal perforation associated with forceful vomiting after a sudden rise in intraesophageal pressure. It represents a diagnostic challenge and remains a major consideration in patients with otherwise unexplained mediastinitis. Patients with significant pleural and mediastinal contamination are at high risk for sepsis and systemic inflammatory response syndrome.
Descending necrotizing mediastinitis refers to a primary complication of oropharyngeal infections that can spread to the mediastinum through the anatomic fascial planes and cervical spaces (prevertebral, retrovisceral, pretracheal, or retropharyngeal).
Pancreatitis can extend from the retroperitoneum into the mediastinum, resulting in mediastinitis. On occasion, osteomyelitis of the spine and ribs may lead to mediastinitis. In 2001 hemorrhagic mediastinitis was found in 5 of 11 patients with inhalational anthrax related to a bioterrorism attack in the United States.
Clinical Presentation
The characteristic clinical findings of acute mediastinitis consist of a sudden and dramatic onset with chills, high fever, tachycardia, tachypnea, and prostration. Retrosternal pain, worsened by breathing or coughing, is common; radiation to the neck and ear may occur. The Hamman sign, a crunching sound heard over the anterior chest wall, synchronous with cardiac systole, may be secondary to pneumomediastinum associated with acute mediastinitis. Accurate diagnosis depends on an appropriate degree of clinical suspicion. Although a history of a potential predisposing event or disease process can be elicited in most patients, cases without these associations may occur. In such circumstances the diagnosis may be delayed because symptoms may mimic those of myocardial infarction, aortic dissection, and pulmonary thromboembolism. In one review of 54 patients with esophageal perforations related to endoscopy, the diagnosis of perforation was made within 2 hours in 94.4% of cases. Descending necrotizing mediastinitis has been linked with significant morbidity and mortality, and early recognition is important for a good prognosis for this potentially fatal condition.
A distinctive clinical picture results from acute mediastinitis secondary to a spontaneous rupture of the esophagus as a result of a violent vomiting episode (Boerhaave syndrome). This condition affects approximately 1 in 6000 patients. Rupture is typically posterior, near the left hemidiaphragmatic crus. Clinically, esophageal perforation must be suspected on the basis of the history in association with vomiting, chest pain, fever, and subcutaneous air. In spontaneous esophageal perforation (Boerhaave syndrome), hematemesis also is common.
During October and November 2001, public health authorities investigated 11 patients with inhalational anthrax related to a bioterrorism attack in the United States. Clinically, patients presented with a biphasic illness characterized by an initial insidious flu-like illness lasting 2 to 4 days and characterized by fever, malaise, myalgias, and nonproductive cough. This was followed by a fulminant acute mediastinitis with respiratory distress and chest pain. Serosanguineous pleural effusions and hemorrhagic mediastinitis were found in 5 patients who died. Immunohistochemical assays demonstrated abundant intracellular and extracellular bacilli, bacillary fragments, and granular antigen staining in mediastinal lymph nodes, surrounding soft tissues, and pleura.
Pathologic Findings and Pathophysiology
Acute mediastinitis is usually infectious in etiology and sometimes progresses to abscess formation. The organisms detected in acute mediastinitis vary with the underlying cause. Mixed infections containing aerobic and anaerobic organisms are commonly associated with acute mediastinitis resulting from esophageal perforation and spread from oropharyngeal sources. Anaerobic bacteria are common in infections from esophageal perforation and oropharyngeal sources. Candida mediastinitis is an uncommon complication of a cardiothoracic surgery but is associated with a high mortality rate.
Imaging Findings
Radiography
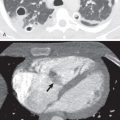
In acute mediastinitis chest radiography may show widening and poor definition of the margins of the superior mediastinum with or without pneumomediastinum ( Fig. 76.1 ). Subcutaneous air may also be seen in the soft tissues of the neck.

Most cases of acute mediastinitis result from esophageal perforation. Radiologically, detection of esophageal perforation relies on the presence of indirect signs, including pneumomediastinum, left-sided pneumothorax, and pleural effusion. Pneumomediastinum typically manifests as delineation of the pleura as a white line adjacent to the mediastinum, linear streaks of radiolucency in the mediastinum and cervical soft tissues, focal retrosternal air collections, linear extrapleural air collection outlining the diaphragm (“continuous diaphragm” sign), and a focal, sharply marginated area of radiolucency in a paraspinal location on the left side immediately above the diaphragm (V sign of Naclerio) ( Fig. 76.2 ). Although contrast-enhanced esophagram has been the standard technique for diagnosis of esophageal perforation, 10% of patients can have a false-negative result. Extravasation of oral contrast material into the mediastinum or into the pleural cavity is an unequivocal sign of perforation ( Figs. 76.3 and 76.4 ). Direct extension of sternal infection after surgery is another common cause of acute mediastinitis. Radiographic findings of sternal dehiscence include displacement, rotation, and fracture of the sternal wires on serial chest radiographs.



Computed Tomography
Computed tomography (CT) is the imaging modality of choice in the evaluation of patients with suspected acute mediastinitis and mediastinal abscess (see Fig. 76.1 ). Common CT findings secondary to esophageal perforation include esophageal thickening, extraluminal gas, pleural effusion, single or multiple abscesses, and extraluminal contrast medium ( Figs. 76.5 to 76.7 ). Pleural effusion tends to be right-sided in patients with iatrogenic, midesophageal perforation and left-sided in patients with spontaneous, distal esophageal perforation. CT esophagography with ingested water-soluble contrast agent is more sensitive than fluoroscopic esophagram in the detection of esophageal perforation.



In descending necrotizing mediastinitis, CT shows solitary or multiple fluid collections, which may be contiguous with other collections in the cervical region, increased attenuation and diffuse obliteration of normal mediastinal fat planes related to fasciitis, cellulitis, or myositis. CT also may depict associated abnormalities, such as pleural and pericardial effusions, vein thrombosis, and lymphadenopathy.
CT is a valuable tool in diagnosing complications after sternotomy because it accurately depicts the extent and depth of the wound infections ( Fig. 76.8 ). Fluid and air collections, hematomas, pleural effusion, and increased attenuation of mediastinal fat are common findings in the immediate postoperative period ( Fig. 76.9 ). Distinguishing these normal postoperative findings from superimposed infection can be difficult or impossible on CT performed within the first few days after surgery. Timing of the CT examination is important in determining the clinical value of the imaging findings, such as cortical destruction of the sternum and the adjacent sternoclavicular joint, widening of the joint space, irregular sternal contours, peristernal soft tissue swelling, and gas or fluid collections. In one series of 50 patients with clinically suspected mediastinitis, these CT findings were nonspecific for mediastinitis until postoperative day 14; however, such findings were highly indicative of mediastinitis after the first 2 weeks.


CT is also a valuable technique in the management of mediastinal abscesses and fluid collections. Percutaneous catheter aspiration and drainage of mediastinal fluid collections, under CT guidance, can be useful as a diagnostic and therapeutic approach.
Imaging Algorithm
In most patients with acute mediastinitis, a confident diagnosis can be made based on clinical and imaging findings. Acute mediastinitis is encountered clinically in two main settings: the rupture or perforation of the esophagus as a complication of instrumentation and the extension of infections from neighboring tissues in the neck. In these circumstances the chest radiograph may show widening of the mediastinum and air within the mediastinum and in the soft tissues of the neck. Esophagram with a water-soluble contrast agent, such as diatrizoate meglumine (Gastrografin), is safe and effective for evaluating the esophagus to rule out esophageal perforations. Esophagram can also be performed safely with barium. A typical esophagram protocol would include both water-soluble contrast to rule out frank rupture and then dilute barium to increase the sensitivity for a small esophageal leak.
Cross-sectional imaging techniques generally are required for diagnosis and evaluation of the site and extent of mediastinal involvement. The main utility of CT is in the evaluation of patients with clinical suspicion of acute mediastinitis and normal or nonspecific radiographic findings. In complications of median sternotomy and closed blunt chest trauma, CT is of great value in determining whether the infection is limited to the presternal tissues, the anterior mediastinum, or both. CT and magnetic resonance imaging (MRI) also may guide the choice of the optimal therapeutic approach.
Differential Diagnosis
The main role of imaging in the diagnosis of acute mediastinitis is in confirming the presence of mediastinal abnormalities consistent with the clinical diagnosis. The radiographic finding of a widened mediastinum in the clinical setting of fever and pleuritic chest pain strongly suggests acute mediastinitis.
Fibrosing Mediastinitis
Etiology, Prevalence, and Epidemiology
Fibrosing mediastinitis, also known as sclerosing mediastinitis and mediastinal fibrosis, is a rare entity characterized by excessive fibrotic reaction usually caused by granulomatous infection, most commonly histoplasmosis and tuberculosis. It also may be idiopathic or secondary to the exposure to methysergide ( Box 76.2 ). Less common causes are silicosis, sarcoidosis, autoimmune disorders, immunoglobulin G4 (IgG4)-related disease, and familial multifocal fibrosclerosis.