Chapter 5
Medical Techniques and Patient Care
Students who successfully complete this chapter will be able to do the following:
• Understand the obligations of the sonographer to patients, institution, and self.
• Discuss the patient care partnership.
• Describe patient reactions to illness.
• Describe the correct techniques for obtaining accurate vital signs.
• Discuss the care of patients with tubes or tubing.
• Discuss the safety considerations associated with patient care.
• List the components of good body mechanics.
• Describe the correct patient-transfer methods.
• Identify good health and hygiene practices.
• Discuss the sonographer’s role in infection control.
• Identify the signs of cardiac arrest and airway obstruction.
• Describe basic life support techniques.
• Discuss the impact of transcultural communications and beliefs on diagnosis and treatment.
automated external defibrillators (AEDs)
cardiopulmonary resuscitation (CPR)
continuous chest compression CPR (CCC-CPR)
Health Insurance Portability and Accountability Act (HIPAA)
methicillin-resistant Staphylococcus aureus (MRSA)
National Patient Safety Goals (NPSGs)
purified protein derivative (PPD)
vancomycin-resistant Enterococcus (VRE)
Patient rights
In addition to having the necessary knowledge and skills to perform competent sonographic examinations, sonographers are responsible for the type of care given to patients. In 1973 the American Hospital Association (AHA) first adopted a Patient’s Bill of Rights with the expectation that hospitals and health care institutions would support these rights in the interest of delivering effective patient care. The AHA encouraged institutions to translate or simplify the bill of rights to meet the needs of their specific patient populations and to make patient rights and responsibilities understandable to patients and their families. The federal government also was concerned about this issue. In 1998 the U.S. Advisory Commission on Consumer Protection and Quality in the Health Care Industry adopted a Consumers’ Bill of Rights and Responsibilities (also known as the Patient’s Bill of Rights). By 2004 the AHA had replaced the Patient’s Bill of Rights with a plain language brochure, The Patient Care Partnership: Understanding Expectations, Rights and Responsibilities, which informed patients about what to expect during their hospital stay with regard to their rights and responsibilities. The most recent update took place in 2008 and includes translations in English, Arabic, Simplified and Traditional Chinese, Russian, Spanish, Tagalog, and Vietnamese. It is available at http://www.aha.org/aha/issues/Communicating-With-Patients/pt-care-partnership.html.
The Affordable Care Act
• No pre-existing condition exclusions for children under age 19
• No arbitrary recisions of insurance coverage
• No lifetime limits on coverage
• No restricted annual dollar limits on coverage
• Protection for patients’ choice of doctors
• Removal of insurance company barriers to emergency department services
More detailed information can be obtained by accessing http://www.healthcare.gov/.
Health Insurance Portability and Accountability Act (HIPAA)
The Privacy Rule was created to achieve the following:
• Give patients more control over their health information
• Set boundaries on the use and release of their health records
• Establish appropriate safeguards that health care providers must achieve to protect the privacy of health information
• Hold violators accountable, with civil and criminal penalties that can be imposed for violation of patients’ privacy rights
• Strike a balance when public responsibility requires disclosure of some forms of data (e.g., to protect public health)
• Enable patients to find out how their information may be used and what disclosure of their information was made
• Limit the release of information to the minimum reasonably needed for the purpose of the disclosure
• Give patients the right to examine and obtain a copy of their own health records and to request corrections
• Put patient information away after hours.
• Take files out of sight of any lingering staff members and custodians.
• Set screensavers on computers for the shortest time possible.
• Take care that any conversations (including phone conversations) are not overheard by other patients.
• Remove patient identification from any scans that will be used for publication or presentation.
• Keep any patient charts filed with names facing the wall to ensure that passersby or visitors to the ultrasound laboratory cannot see the names or any information on the charts.
Vital signs
Pulse
Pulse rate refers to the number of beats per minute (bpm), whereas rhythm refers to the time interval between beats. The sonographer should evaluate whether the pulse has a smooth and regular rhythm as opposed to irregular rhythms with skipped beats. The strength of a pulse refers to its force and usually is described as either bounding or weak and thready. Substances such as coffee, tea, tobacco, or certain drugs can cause rhythm irregularities. Shock and hemorrhage can cause a weak, thready pulse, whereas fever can produce a bounding pulse. The normal adult pulse rate is 60 to 65 beats per minute (bpm). Newborn infants have a pulse rate of 120 to 140 bpm, and women, children, and elderly patients usually have a slightly faster than normal pulse rate (Table 5-1). Athletes in good condition generally have a slower pulse: below 60 bpm.
Table 5-1
Average Heart Rates for Different Age Groups
| Age Group | Beats Per Minute (BPM) |
| Adult | 60–100 |
| Child | 100–120 |
| Newborn | 140 |
| Fetus | 120–160 |
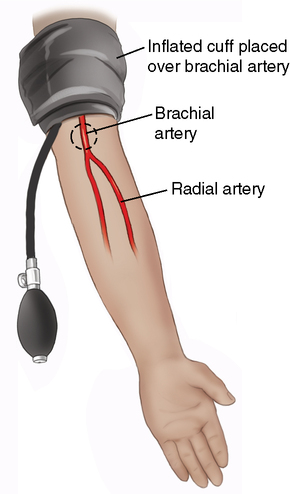
The pulse is felt by gently compressing the artery over a bony prominence in the area. Never feel the pulse with the thumb, because the thumb has a pulse of its own that interferes with obtaining an accurate reading of the patient’s pulse. An arterial pulse should be obtained as follows (Figure 5-1):

The patient’s arm should be supported in a comfortable position. Never use your thumb to feel the patient’s pulse.
• Explain to the patient that you plan to take his or her pulse.
• Place the patient’s arm in a comfortable, resting position.
• Identify the location of the artery by placing your fingertips over the artery and pressing firmly enough to feel the pulsation.
• Count the beats of the pulse (starting the count with zero) for at least 30 seconds. Multiply this number by 2 to obtain the beats per minute.
• If irregularities are noted (too fast/too slow), count the beats for a full minute and report the findings.
Blood Pressure
• Pre-hypertension: between 120/80 and 139/89
• Stage one hypertension: 140/90
• Stage two hypertension: 160/100
A wide variety of blood pressure monitors are available: mercury/aneroid, digital, and multipurpose vital sign monitors. The most familiar of these is the sphygmomanometer (either mercury or aneroid), used with a cuff and a stethoscope (Figure 5-2). Mercury manometers, which provide the most accurate measurements, show increments of 10 points, from 0 to 300. Aneroid manometers show units of 20, ranging from 20 to 300. Raising the silver column of mercury or the aneroid needle to 200 begins the procedure. A properly calibrated manometer will show the needle and mercury column at the zero mark on the mercury manometer (20 on the aneroid manometer) when not in use.
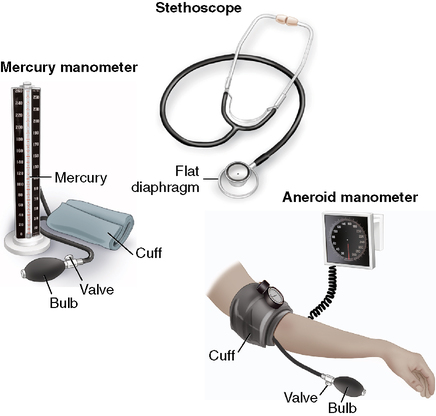
Mercury and aneroid types of manometers and accessory equipment (stethoscope and cuff).
The cuff contains an inflatable rubber bladder; center this over the brachial artery, 1 inch above the elbow (Figure 5-3). Wrap the cuff snugly but not tightly. If the cuff is too loose, systolic and diastolic readings will be heard higher than their actual values.
Blood pressure cuff should be snugly wrapped approximately 1 inch above the bend of the arm, leaving room to place a stethoscope over the brachial artery at the bend of the arm.
A stethoscope with a flat diaphragm is best for taking blood pressure. After using your fingers to locate the brachial artery in the shallow depression where the elbow bends, place the diaphragm of the stethoscope over the artery without touching the cuff or the patient’s clothing (Figure 5-4). Use gentle application, because too much pressure can cause abnormally low diastolic sounds.
Measuring blood pressure
Sonographers measuring blood pressure should do the following:
• Explain the procedure to the patient in a private and noise-free environment.
• Ensure that the patient rests for 5 minutes before the blood pressure is taken. If the patient has been actively exercising, take the reading after 15 to 30 minutes of rest.
• Select and use the same site consistently, because variation occurs in blood pressures taken in different locations. Take blood pressures with the patient in the same position each time. A lying, sitting, or standing blood pressure can vary within the same individual.
• Remove, as necessary, any of the patient’s clothing, to expose the site. The patient’s arm should be positioned on a supporting structure (table or bed) at heart level while the blood pressure is being taken.
• Check that no leaks exist in the tubes, cuff, or valve, and remember that using too small a cuff can result in pressure readings higher than normal.
• Sit or stand when taking the blood pressure to read the manometer at eye level. The manometer should read 0 before beginning.
• Deflate any air out of the cuff, and apply the cuff just far enough above the patient’s elbow to leave the space over the brachial artery free. Wrap the cuff firmly around the patient’s arm and fasten it securely on the last turn.
• Locate the pulse in the artery and place the stethoscope directly over the point of strongest pulsation.
• Hold the rubber bulb in the palm of one hand; close the valve on the rubber bulb with a thumb and finger and rapidly inflate the cuff by pumping the bulb.
• Inflate the cuff to about 20 to 30 mm Hg above the expected systolic reading. As the cuff pressure increases, it will shut off the flow of blood within the artery. Inflation of the cuff should take 7 seconds or less.
• Carefully loosen the valve and deflate the cuff slowly and steadily. Then listen carefully for sounds of the first heartbeat (systolic pressure) and watch the mercury column or aneroid needle gauge for the points at which the sounds are first heard.
• Deflate about 2 to 3 mm Hg per heartbeat until all sounds stop or a distinct change occurs in the sound (diastolic pressure).
• When all sounds stop, deflate the cuff rapidly and completely to 0.
• Do not reinflate the cuff during the reading. If you must repeat a reading, let all the air out of the cuff and allow 15 seconds to lapse before inflating the cuff again.
Interpreting arterial sounds
Arterial sounds are interpreted as follows:
• Systolic readings are the first sounds heard as the cuff is deflated (blood resuming flow as the heart pumps).
• The last sound heard as the air is let out is the diastolic reading (blood flowing freely through the artery when the heart is resting).
• If hearing the diastolic sounds is difficult, completely deflate the cuff. After 15 seconds, the patient should raise his or her arm to drain the blood from the blood vessels of the lower arm. When the patient lowers the arm, retake the blood pressure.
• Repeat the procedure if you have any doubt about the reading. If the reading is elevated, recheck it after 5 minutes. Briefly explain the reason for a second reading to avoid alarming the patient and affecting the blood pressure.
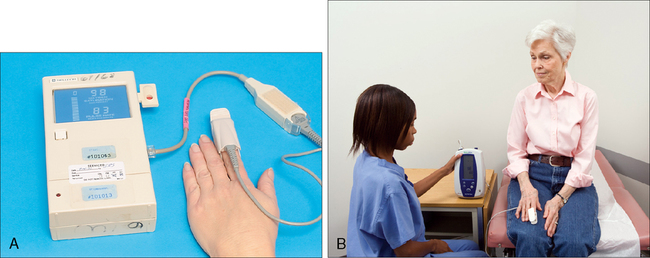
Continuous vital signs monitors also are widely used in hospital settings. They are designed to spot check or continuously monitor several critical parameters such as heart (pulse) rate, pulse oximetry, blood pressure, and temperature. Pulse oximeters are used in various situations, especially in surgery and the intensive care unit (ICU). Pulse oximetry measures the oxygen concentration in arterial blood. The normal range is 95% to 100%. Measurements are used to prevent hypoxia and to evaluate the effectiveness of treatment. A sensor is attached to the patient’s finger, toe, earlobe, nose, or forehead. The sensor light beams pass through the tissues, and a detector on the other side measures the amount passing through the tissues. The oximeter then measures the oxygen concentration from this information (Figure 5-5). That value, and the patient’s pulse rate, are displayed on the monitor. Oximeter alarms will sound if the oxygen concentration is low or if the pulse rate is too fast or too slow. Easily attached to IV poles or on rolling stands, these monitors may accompany inpatients who must be transported to the ultrasound laboratory.
Intravenous Equipment
IV tubing connected to a plastic bag or bottle is used to infuse fluids into the patient’s body. A needle or plastic catheter attached to the container is inserted into a vein. The flow of fluid is measured by a drip meter, and a clamp on the tubing is used to regulate the flow of the prescribed fluid (Figure 5-6).
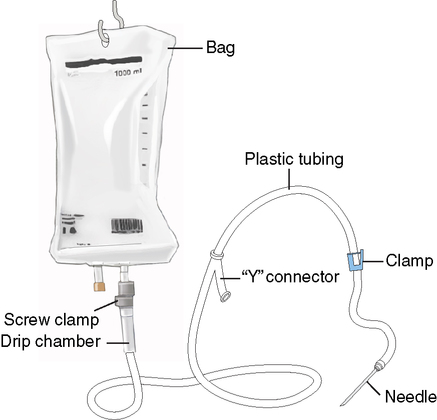
Plastic tubing leads from a solution-filled bag at one end and connects to a needle at the other end. Clamping the tubing controls the rate of flow.
1. If the needle has been inserted in the patient’s hand or arm, help the patient keep the involved arm straight.
2. Never lower the bottle or bag below the level of the needle insertion when transferring or positioning the patient.
3. Watch for and immediately report any of the following:
• Nausea, vomiting, rapid breathing, or an increase in pulse rate occurs, which are signs of circulatory overload that must be dealt with immediately.
• No solution is passing from the bottle into the tubing, even though solution is still in the bottle.
• The plastic drip chamber is completely filled with solution.
• Blood appears in the tubing at the needle end.
• All of the solution has run out of the bottle or bag or it is almost empty.
• The needle has deliberately or accidentally been removed.
• The patient complains of pain or tenderness at the needle insertion site.
• A raised or inflamed area occurs on the patient’s skin or near the needle insertion, which may mean that the solution has infiltrated and is running into the adjacent tissues (the sonographer may be asked to close the clamp to shut off the flow of solution).
• The tubing becomes disconnected, and the patient is bleeding freely from the connection site.
Nasogastric Tubes
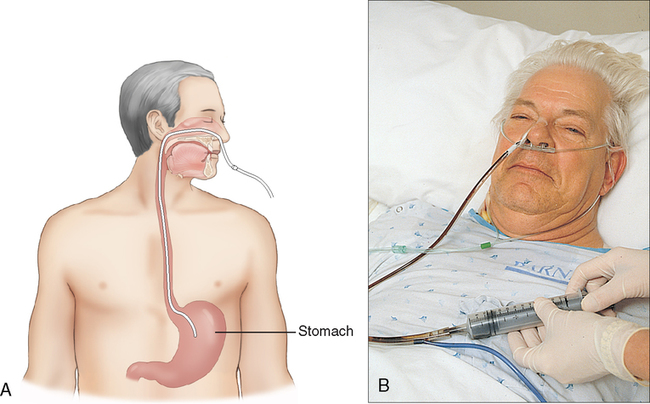
Hospital patients commonly have a tube inserted into one nostril. Depending on the length of the tube, it may terminate in the patient’s stomach or intestine. Such tubes can be used for feeding, to obtain specimens, to treat intestinal obstructions, to prevent or treat distention after surgery, or to drain fluids from the patient’s stomach by suction (Figure 5-7).
Here are some rules for working with patients connected to mechanical suction machines:
Oxygen Therapy
Delivery systems for oxygen therapy include in-room piping systems and oxygen tanks, or cylinders. If a laboratory is equipped with an in-room piping system, oxygen and suction usually are provided through wall outlets. Outlet connectors, which vary in shape, color, and connection methods used, are keyed to a specific gas or function (Figure 5-8).
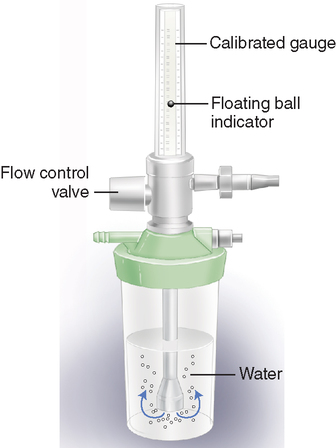
Water levels must be kept high enough to bubble as oxygen flows through the flowmeter.
• Transport a high-pressure cylinder unless it is secure in a cylinder cart.
• Allow a cylinder to stand free; it must be secured to avoid falling and causing an accident.
• Transport patients on a stretcher with a cylinder lying next to them.
• Place a cylinder near a source of heat such as a radiator, because it may cause an explosion.
The delivery of oxygen to the patient may involve the use of either high- or low-flow devices. Among the low-flow devices are the nasal cannula or nasal prongs, nasal catheter, or simple oxygen masks. The nasal cannula is used when a patient needs extra oxygen rather than a total supply of oxygen (Figure 5-9, A). The prongs are inserted into the patient’s nostrils and held in place by an elastic band around the patient’s head. They are connected to the oxygen source by a length of plastic tubing.
• Simple mask: A transparent mask with a simple nipple adapter fitted over the nose, mouth, and chin (Figure 5-9, B)
• Partial rebreathing or reservoir mask: A low-flow device identified by the presence of a bag, which must remain constantly inflated by one-third (Figure 5-9, C)
• Venturi mask: A high-flow mask that provides the most reliable and consistent oxygen enrichment. The Venturi mask is identified by the presence of a hard plastic adapter with large “windows” on either side
• Observe all fire regulations in effect at the institution.
• Check the flowmeter to ensure oxygen is being delivered to the patient. The water level in the humidifying chamber should be high enough so that it bubbles as the oxygen goes through it. The tubing connected to the oxygen source should be taped to the patient to help keep it from accidentally being pulled when moving the patient.
• The patient should not lie on the tubing and the tubing should not be kinked, which can slow or stop the oxygen flow.
• Inhalation therapy or respiratory therapy departments are responsible in most hospitals for the patient’s treatment. They should be called to make any needed adjustments after checking with the patient’s physician or nurse.
Catheters
The most common kind of catheter used for removing fluids from the body is the urinary catheter. The catheter (made of plastic tubing) is inserted through the patient’s urethra and into the bladder (Figure 5-10). Catheters may be used to obtain sterile specimens when patients are unable to urinate naturally or to determine how much residual urine remains in a patient’s bladder after urination.
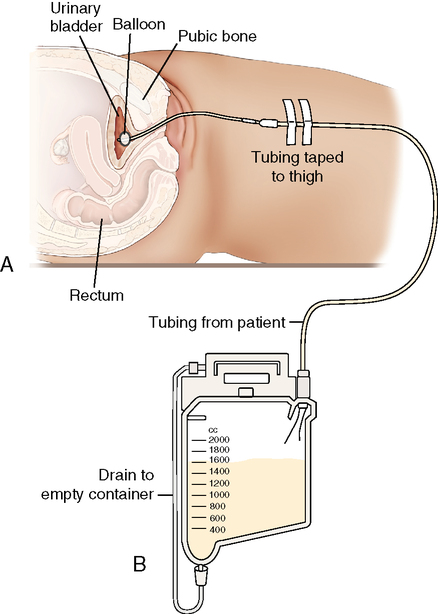
A, A plastic/rubber urinary catheter is inserted through the urethra and into the bladder. B, Urine drains into a container.
Colostomies and Ileostomies
• Use clean, rather than sterile technique, whenever removing or changing these dressings or bags. Wear gloves at all times. If a patient has a latex allergy, wear vinyl gloves.
• Gently remove the old appliance and clean the area around the stoma. Tape a folded gauze pad around the stoma to absorb any discharge and to protect the scanning surface during the examination.
• Flush contents of the old appliance into a toilet. Then dispose of the old appliance in a plastic bag to prevent cross-contamination.
• Before applying a new bag, cleanse and dry the skin around the stoma so that the appliance can be fastened securely to prevent the escape of discharge or odors.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree