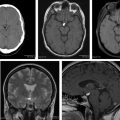
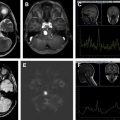
Metastatic cancer to the central nervous system is primarily deposited by hematogenous spread in various anatomically distinct regions: calvarial, pachymeningeal, leptomeningeal, and brain parenchyma. A patient’s overall clinical status and the information needed to make treatment decisions are the primary considerations in initial imaging modality selection. Contrast-enhanced MR imaging is the preferred imaging modality. Morphologic MR imaging is limited to delineating anatomic deraignment of tissues. Dynamic susceptibility contrast-enhanced perfusion and diffusion-weighted physiology-based MR imaging sequences have been developed that complement morphologic MR imaging by providing additional diagnostic information.
Patients with neurologic symptoms often undergo noncontrast CT as an initial screening tool for the diagnosis of metastatic disease. The presence of a mass lesion by CT may be the first clue to the presence of a previously unidentified systemic neoplastic process. Conversely, asymptomatic patients with known systemic malignancy often undergo staging of the CNS prior to the initiation of medical therapy using MR imaging.
Patients with metastatic intracranial neoplasms often present with focal neurologic deficits, which are clinically indistinguishable from acute cerebral infarction. To further confuse the clinical diagnosis, metastatic neoplasms can resemble cerebral ischemia on initial imaging examinations. CT findings that favor the diagnosis of metastatic intracranial neoplasms include round hypodensity that preferentially involves the white matter with sparing of cortical gray matter that is not confined to a specific vascular territory. MR imaging is markedly useful in the evaluation of lesions initially detected by noncontrast CT imaging. Evolving subacute infarctions with normalizing ADC metrics should not demonstrate elevated CBV by DSC perfusion imaging.
Summary
The identification and classification of metastatic tumor can be a challenging task; however, with advanced CT and MR imaging of the CNS, multiple tools are available to correctly achieve this objective. DWI and DSC MR imaging, although currently investigational to some degree, add additional diagnostic information, allowing for improved tumor characterization.
Disclosures: None.
References
- 1. Barnholtz-Sloan J.S., Sloan A.E., Davis F.G., et al: Incidence proportions of brain metastases in patients diagnosed (1973 to 2001) in the metropolitan Detroit cancer surveillance system. J Clin Oncol 2004; 22: pp. 2865-2872
- 2. Nussbaum E.S., Djalilian H.R., Cho K.H., et al: Brain metastases. Histology, multiplicity, surgery, and survival. Cancer 1996; 78: pp. 1781-1788
- 3. Das A., and Hochberg F.H.: Clinical presentation of intracranial metastases. Neurosurg Clin N Am 1996; 7: pp. 377-391
- 4. Svokos K.A., Salhia B., and Toms S.A.: Molecular biology of brain metastasis. Int J Mol Sci 2014; 15: pp. 9519-9530
- 5. Beasley K.D., and Toms S.A.: The molecular pathobiology of metastasis to the brain: a review. Neurosurg Clin N Am 2011; 22: pp. 7-14
- 6. Cha S.: Neuroimaging in neuro-oncology. Neurotherapeutics 2009; 6: pp. 465-477
- 7. Ercan N., Gultekin S., Celik H., et al: Diagnostic value of contrast-enhanced fluid-attenuated inversion recovery MR imaging of intracranial metastases. AJNR Am J Neuroradiol 2004; 25: pp. 761-765
- 8. Singer M.B., Atlas S.W., and Drayer B.P.: Subarachnoid space disease: diagnosis with fluid-attenuated inversion-recovery MR imaging and comparison with gadolinium-enhanced spin-echo MR imaging– blinded reader study. Radiology 1998; 208: pp. 417-422
- 9. Lloret I., Server A., and Taksdal I.: Calvarial lesions: a radiological approach to diagnosis. Acta Radiol 2009; 50: pp. 531-542
- 10. Garfinkle J., Melançon D., Cortes M., et al: Imaging pattern of calvarial lesions in adults. Skeletal Radiol 2010; 40: pp. 1261-1273
- 11. Tyrrell R.L., Bundschuh C.V., and Modic M.T.: Dural carcinomatosis: MR demonstration. J Comput Assist Tomogr 1987; 11: pp. 329-332
- 12. Mahendru G., and Chong V.: Meninges in cancer imaging. Cancer Imaging 2009; 9: pp. S14-S21
- 13. Demopoulos A.: Leptomeningeal metastases. Curr Neurol Neurosci Rep 2004; 4: pp. 196-204
- 14. Ribeiro H.B., Paiva T.F., Mamprin G.P., et al: Carcinomatous encephalitis as clinical presentation of occult lung adenocarcinoma: case report. Arq Neuropsiquiatr 2007; 65: pp. 841-844
- 15. Olsen W.L., Winkler M.L., and Ross D.A.: Carcinomatous encephalitis: CT and MR findings. AJNR Am J Neuroradiol 1987; 8: pp. 553-554
- 16. Nemzek W., Poirier V., Salamat M.D., et al: Carcinomatous encephalitis (miliary metastases): lack of contrast enhancement. AJNR Am J Neuroradiol 1993; 14: pp. 540-542
- 17. Walker M.T., and Kapoor V.: Neuroimaging of parenchymal brain metastases. Cancer Treat Res 2007; 136: pp. 31-51
- 18. Chalela J.A., and Gomes J.: Magnetic resonance imaging in the evaluation of intracranial hemorrhage. Expert Rev Neurother 2004; 4: pp. 267-273
- 19. Aygun N., and Masaryk T.J.: Diagnostic imaging for intracerebral hemorrhage. Neurosurg Clin N Am 2002; 13: pp. 313-334
- 20. Bradley W.G.: MR appearance of hemorrhage in the brain. Radiology 1993; 189: pp. 15-26
- 21. Hayashida Y., Hirai T., Morishita S., et al: Diffusion-weighted imaging of metastatic brain tumors: comparison with histologic type and tumor cellularity. AJNR Am J Neuroradiol 2006; 27: pp. 1419-1425
- 22. Cha S., Lupo J.M., Chen M.H., et al: Differentiation of glioblastoma multiforme and single brain metastasis by peak height and percentage of signal intensity recovery derived from dynamic susceptibility-weighted contrast-enhanced perfusion MR imaging. AJNR Am J Neuroradiol 2007; 28: pp. 1078-1084
- 23. Wang S., Kim S., Chawla S., et al: Differentiation between glioblastomas, solitary brain metastases, and primary cerebral lymphomas using diffusion tensor and dynamic susceptibility contrast-enhanced MR imaging. AJNR Am J Neuroradiol 2011; 32: pp. 507-514
- 24. Barajas R.F., Chang J.S., Sneed P.K., et al: Distinguishing recurrent intra-axial metastatic tumor from radiation necrosis following gamma knife radiosurgery using dynamic susceptibility-weighted contrast-enhanced perfusion MR imaging. AJNR Am J Neuroradiol 2009; 30: pp. 367-372
- 25. Bronen R.A., Fulbright R.K., Spencer D.D., et al: MR characteristics of neoplasms and vascular malformations associated with epilepsy. Magn Reson Imaging 1995; 13: pp. 1153-1162
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree