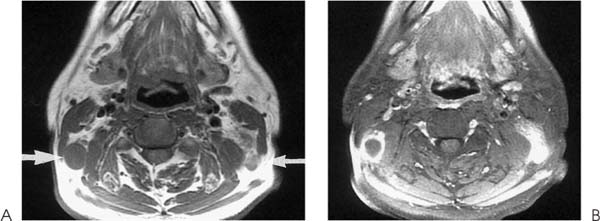
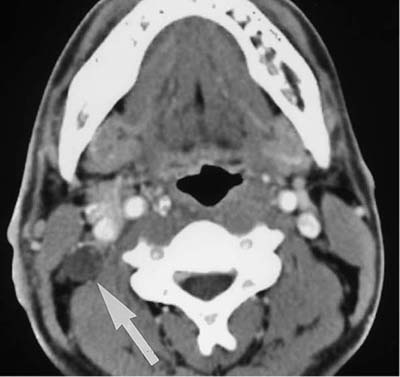
Chapter 164 Cervical nodal metastasis is extremely common. Most head and neck tumors spread to the neck nodes as part of their natural history. For instance, depending on the primary site, up to 80% of patients with upper aerodigestive mucosal malignancy will have cervical nodal metastasis at presentation. The presence of cervical lymphadenopathy is noted to reduce the long-term survival rate by 50%. The traditional terminology of cervical nodes is based on the description by the French anatomist, Rouvière. This system refers to the classical surface triangles of the neck. The orientation of these triangles makes them rather unsuitable for description in axial images. In recent years, the simpler numerical system (Table 164–1; Fig. 164–4) became the dominant nomenclature. The retropharyngeal, parotid, and facial groups are not included in this classification. Under this system, a radiologist can assign a numerical level for nodal involvement and when the retropharyngeal, parotid, or facial nodes are involved they should be reported as such. In 1997 the International Union against Cancer and the American Joint Committee on Cancer (AJCC) introduced a new group of nodes to specifically address the importance of supraclavicular nodal metastasis in nasopharyngeal carcinoma. These nodes represent the lower level IV and V nodes. Carcinomas show a high tendency to infiltrate local lymphatics at an early stage. Groups of tumor cells within the infiltrated lymphatics may embolize to the regional lymph nodes (Figs. 164–1 and 164–2). It takes about 1 billion malignant cells to form a mass of 1 mm3. Such lesions are difficult to see with the naked eye, let alone on CT or MR imaging (Fig. 164–3). The embolized malignant cells initially lodge in the subcapsular sinuses. If they survive they will eventually replace the lymph node. This may lead to extracapsular spread or further extension to the next group of lymph nodes via the efferent lymphatics. Patients with cervical lymphadenopathy may present in several ways. First, the initial presentation is that of the primary disease wherein cervical lymphadenopathy is detected during physical or radiological assessment. Second, patients may present with hard neck masses and the primary malignant lesion is found during further evaluation. Third, in 2 to 3% of all patients with head and neck cancer who present with cervical lymphadenopathy, the primary tumor was never found. Figure 164–1. Cervical lymphadenopathy with nodal necrosis. (A) Axial T1-weighted MR image shows a well demarcated right cervical node (large arrow). There are also nodes on the contralateral side (small arrow). (B) Axial contrast-enhanced MR image shows right cervical node demonstrating rim enhancement and necrotic center. Note the intense enhancement on the contralateral side.
Metastatic Cervical Lymphadenopathy
Epidemiology
Classification of Cervical Nodes
Pathology
Clinical Findings
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree