Definition Amniotic band syndrome (ABS) is a rare spectrum of congenital anomalies caused by entanglement of fetal parts, or disruption of anatomic structures, by fibrous amniotic bands.
Epidemiology The exact incidence of ABS is uncertain but may be as high as 1 in 15,000 live births.
Embryology There are two theories proposed for ABS: (1) The bands are due to early amniotic rupture, leaving fibrous bands floating in the amniotic fluid to become entangled with the fetus; or (2) the bands are secondary to membrane malformations caused by ischemia. There are others who postulate that ABS is part of the limb–body wall spectrum. The timing of the insult determines the effect of the amniotic band on fetal development. An amniotic band can be: (1) disruptive, resulting in finger, toe, or extremity amputation; (2) an early insult may give rise to a malformation (i.e., an encephalocele); and (3) if a band constricts movement, a deformation (scoliosis) may result.
Inheritance Pattern ABS appears to be sporadic. ABS has been associated with maternal Ehlers-Danlos syndrome and epidermolysis bullosa.
Teratogens None are known.
Prognosis The prognosis depends on the resulting anomalies. Cranial and chest anomalies are more likely to be fatal, while limb involvement may have a better prognosis.
Atypical anomalies or an unusual constellation of abnormalities are frequently the presenting findings for ABS. Some anomalies that have been associated with ABS are as follows:
Isolated limb amputations or missing hands, feet, or digits in 80% of cases
Midline cleft lip, or transverse facial clefts
Asymmetric craniofacial defects
Acrania or encephalocele
Body wall defects (i.e., ectopia cordis, gastroschisis, omphalocele, and limb–body wall)
If an isolated abnormality, or group of anomalies, seems asymmetric or atypical, ABS should be considered.
The amniotic fluid volume may be decreased.
ABS has been detected as early as the first trimester.
ABS can be definitively identified when the following occur:
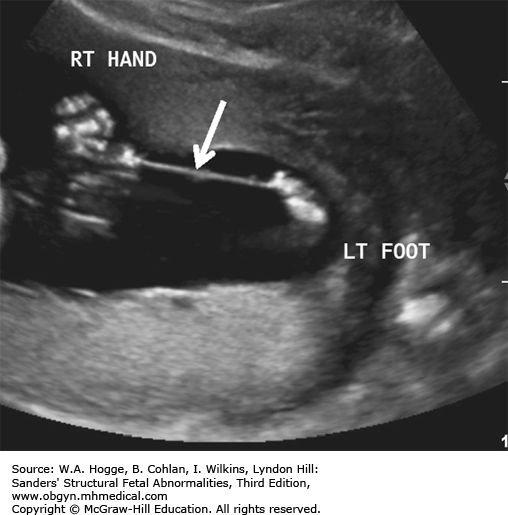
Bands can be visualized within the amniotic fluid and appear as single or multiple thin membranes that attach to, or limit the motion of, specific fetal parts.
They can be difficult to identify; only the sequelae of the amniotic bands may be apparent.
Extremity constriction can be the first sign and usually presents with edema of the distal extremity. This is frequently followed by limb amputation.
Look for
Amnion in continuity with the fetal parts
Extremity edema/localized swelling with reduced distal vascular flow detected with Doppler
Fetal scoliosis
Echogenic debris within the amniotic fluid
Anomalies that can be isolated, can be related to aneuploidy or a syndrome, or can be ABS-related defects, including
Body stalk anomaly
Cephalocele
Acrania
Cleft lip
Omphalocele
Amniotic sheets
Chorioamniotic separation
Investigations and Consultations Required Further consultation depends on the site(s) involved.
Fetal Intervention Fetoscopic intervention has been performed to lyse bands that show evidence of increasing vascular compromise of a limb; however, the diagnosis is frequently made after the damage has occurred.
Monitoring Frequent ultrasound examination of the extremities is critical to monitor for evidence of vascular compromise. Monitoring should be in a facility with the means for fetal intervention.
Pregnancy Course In most cases, the damage from the bands has preceded ultrasound diagnosis; further ultrasound examinations may be useful to monitor for further injury.
Delivery Most deliveries will need to occur in a tertiary center for newborn evaluation and treatment planning. The mode of delivery will depend on the location and extent of the defects.
Resuscitation In general, most fetuses that have been affected by ABS do not experience distress in labor and thus do not require assistance with the onset of respiration. Only those with significant chest, face, or cranial defects are at risk for respiratory compromise and will need intervention.
Transport Indications for referral to a tertiary perinatal center immediately following birth include anomalies that will require specialist pediatric surgical correction, such as abdominal wall defects or partially compromised extremities.
Testing and Confirmation There are no specific tests for the evaluation of fetuses with suspected ABS. Pathological evaluation of the membranes and placenta is suggested.
Nursery Management Nursery management is supportive, depending on the location and extent of the associated defects.
Definition Chorioangiomas are benign vascular tumors of the placenta that are most commonly encapsulated and intraplacental and found on the fetal side of the placenta.
Epidemiology Chorioangiomas are the most common primary tumors of the placenta and are found in approximately 1% of term placentas.
Embryology Chorioangiomas are either hamartomas derived from primitive chorionic mesenchyme or placental hemangiomas arising from the chorionic plate.
Inheritance These tumors are sporadic, with no increased risk in future pregnancies.
Prognosis Most chorioangiomas are incidental findings. Very rarely, secondary fetal hydrops can develop.
Fetus
The fetus is usually normal.
On rare occasions, severe fetal anemia develops because the mass shunts blood and acts as an arteriovenous malformation.
Hydrops may develop, with the earliest signs being hepatosplenomegaly and small pericardial effusions.
Amniotic Fluid
If a large mass is present, the amniotic fluid volume is almost always increased.
Placenta
A well-defined mass is present in the placenta that demonstrates arterial flow on color Doppler.
The mass is usually solitary, but can be multiple, and usually protrudes into the amniotic cavity.
It is often located near the cord insertion, and vascularity varies.
Color Doppler mapping usually demonstrates arterial flow compatible with an arteriovenous malformation.
Vascularity and size (≥5 cm) tend to correlate with polyhydramnios and hydrops.
Chorioangiomas are usually not associated with any complications if they are less than 5 cm in diameter.
Earliest detection reported is at 15 weeks’ gestation, but chorioangiomas often develop in the second trimester of pregnancy.
Venous lakes can be confused with chorioangiomas. Venous flow within a venous lake may not be visible with color flow or Doppler sonography. Observation with real-time imaging can reveal blood flow movement. Venous lakes often lie at the edge of the placenta and can protrude into the amniotic fluid.
The chorioangioma may lie alongside the fetus and be mistaken for a fetal mass, such as a sacrococcygeal teratoma.
Placental hematoma: This is a mass with a similar appearance to a chorioangioma arising from the placental surface. No flow will be seen in real time or with Doppler imaging.
Placental lake on placental surface: The apparent mass will show venous flow with real-time imaging and no flow with color flow or Doppler imaging.
Placental cyst: Cysts arising from the placental surface often have a solid component at the base. A round, thin membrane outlining the echo-free component of the cyst will be seen. These cysts may represent a resolving hematoma.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree