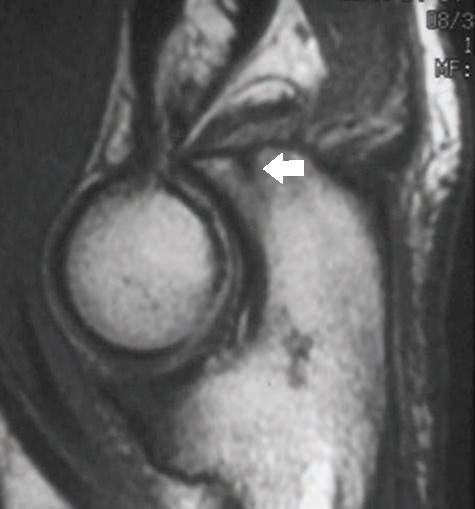
FIGURE 12.31 Type II coronoid fracture. Proton density-weighted sagittal MR image through the elbow show a coronoid fracture that involves less than 50% of the coronoid process (arrow) with edema on both sides of the fracture. The designation of near dislocation is applied as the distal humeral articular surface still contacts the distal coronoid articulating surface.
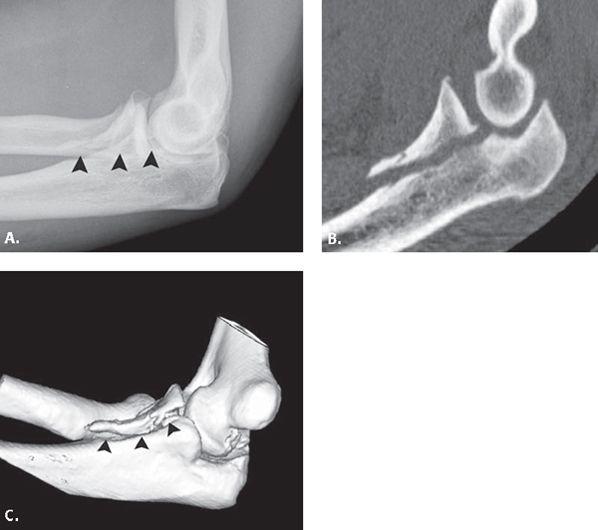
FIGURE 12.32 Type III coronoid fracture. A: Lateral radiograph shows a large coronoid fracture (arrowheads) that involves greater than 50% of the coronoid process. B: Sagittal reformatted computed tomography (CT) image and C: three-dimensional surface-rendered CT of the elbow confirm this finding.
Olecranon
Olecranon stress fractures have been described in throwing athletes, gymnasts, and weightlifters. Among the first reported cases were those in javelin throwers (58). Four distinct types of olecranon stress fractures have been described in the literature based on location of fracture as well as age group involved (Figs. 12-34–12-36). Fractures of the olecranon tip and oblique fractures through the midportion of the olecranon occur in adults, whereas transverse fractures and osteochondroses occur in the skeletally immature patient.
Different mechanisms of injury have been proposed for the different types of fractures described. It appears to be the general consensus in the literature that olecranon tip fractures result from impingement of the olecranon in its osseous fossa (58, 66, 67). Furthermore, asymmetric hypertrophy of the distal humerus and proximal ulna, radiographic findings often present in pitchers, result in decreased space within the olecranon fossa, further exacerbating the impingement. Oblique fractures may simply result from the biomechanical stressors intrinsic to the throwing motion. Suzuki et al. (68) noted that during the acceleration phase of throwing, the posteromedial olecranon impacts the medial wall of the fossa while concomitantly, the lateral aspect of the coronoid impinges against the intercondylar notch. These two points of stress could provide the points of insufficiency to result in an oblique fracture across the olecranon. The transverse fracture of the adolescent may be caused from extensor overload by the triceps at a weak area of the olecranon, notably the physis. It is proposed that the physis is pulled apart by repeated forceful contractions of the triceps, resulting in transient localized ischemia that compromises cartilage mineralization (66, 69). Osteochondroses of the olecranon epiphysis, the second type of fracture identified in the skeletally immature patient, may occur as a result of avascular necrosis. Similar traction forces may disturb ossification and cause fragmentation. Although not described formally in the literature as a specific type of stress fracture, painful, persistent bone marrow edema in the absence of a fracture line has been encountered in the adolescent patient population (58). This entity has been described in a little league baseball pitcher and was believed to be the result of traction forces on the olecranon.
FIGURE 12.33 Sublime tubercle fracture. Frontal radiograph of the elbow shows hypertrophic osseous change at the sublime tubercle of the coronoid process. Superimposed on these hypertrophic changes, there is a fracture (arrowhead) consistent with an avulsion of the anterior band of the ulnar collateral ligament.
FIGURE 12.34 Olecranon stress fracture. T1-weighted sagittal MR image shows a linear low-signal–intensity oblique fracture (arrowheads) extending through the midportion of the olecranon process. This is a well-recognized pattern of injury.
FIGURE 12.35 Olecranon stress fracture. T1-weighted sagittal MR image shows a linear low-signal–intensity fracture line in the tip of the olecranon (arrow) that parallels the long axis of the ulna. This is a common pattern of injury identified in overhead throwers resulting from the repetitive and forceful engagement of the olecranon tip and fossa.
FIGURE 12.36 Stress-related olecranon physeal injury in a gymnast. T2-weighted sagittal MR image through the elbow shows bone marrow edema in the olecranon (arrow) with abnormal widening and fluid between the olecranon ossification center and shaft (curved arrow).
The diagnosis of stress fractures in the adolescent patient can be particularly challenging as a result of variations in the appearance of the centers of ossification. A dense sclerotic edge develops along the physis just before ossification that should not be mistaken for a fracture or necrosis. Multiple centers of ossification within the epiphysis can exist. The physis can measure greater than 5 mm and still be within normal limits. In general, however, fractures tend to displace fat pads, run obliquely to the ulnar shaft axis, and cause soft tissue swelling and joint effusion.
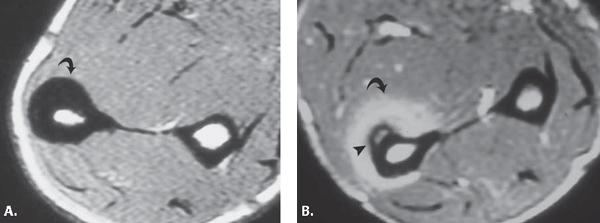
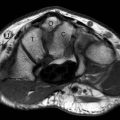
FIGURE 12.37 Ulnar shaft stress changes. A: T1-weighted axial MR image in the midforearm shows gross thickening of the periosteum of the ulna (curved arrow). B: T1-weighted axial MR image after administration of intravenous contrast material shows avid enhancement of the periostitis about the ulna (curved arrow) and an additional focus of subperiosteal hemorrhage (arrowhead).
Ulna
Stress fractures in the ulna have been reported in tennis players, softball players, weightlifters, table tennis players, bowlers, and baton twirlers (70). Although the primary mechanism of injury in ulnar stress fracture appears to be torsional stress, multiple mechanisms of injury have been proposed depending on the nature of the offending activity. In weightlifting, the mechanism is believed to be repetitive flexion and extension at the elbow with the forearm either pronated or supinated. This results in a vertical or torque-like stress on the midulna (71). In the bowler, the mechanism of the stress fracture, occurring in the distal third of the ulna, was believed to be related to repeated stress at the origin of the flexor digitorum profunda muscle (72). Imaging findings can include subtle thickening of the cortex and periosteal reaction with or without the presence of a fracture line (Fig. 12.37). If such findings are present on plain film, cross-sectional imaging through the area of abnormality can be helpful to identify subtle areas of cortical fracture with adjacent callus formation. These can involve the periosteum, endosteum, or both depending on the degree of fracture extension.
Radius
Stress fractures of the radius were first described in the military activity of “field gun running,” an activity that involves carrying a heavy gun barrel across the forearms of the radius bilaterally (73, 74). Radial stress fractures have also been described in gymnasts, tennis players, pool shooters, and cyclists (73, 75–78). In the gymnast, distal radial growth plate changes as well as radial shaft changes can be stress-related. The location of the stress fracture along the radial shaft can correspond to external forces resulting in chronic repetitive microtrauma or muscular attachment sites depending on the activity involved (Fig. 12.38).
Osteochondral Injury
Nomenclature and Imaging Diagnosis
Although confusion remains between the designation osteochondral injury and osteochondritis dissecans, it is really the etiology of the process that is in question. An osteochondral injury involves the separation of a segment of articular cartilage along with its underlying bone. It is a general term used to characterize the pathology encountered at the articular surface of a joint with no allusion to etiology. Mechanically, an osteochondral injury is produced by either repetitive and prolonged joint overloading or a sudden impact that results in high compressive stress to the tissue and high shear stress at the subchondral bone junction. This mechanical stress can occur in the setting of normal or abnormal underlying bone. The basic types of osteochondral lesions that occur in the elbow are classified by acuity as well as clinical history, including previous trauma and age at onset of symptoms. Differential considerations regarding etiology include the acute posttraumatic elbow as discussed in Chapter 10 and the osteochondroses, including Panner’s disease and osteochondritis dissecans.
FIGURE 12.38 Radial stress fracture. A: Frontal radiograph of the forearm shows a normal appearance with no evidence of fracture or periostitis. B: T2-weighted fat-suppressed coronal MR image through the forearm shows globular increased signal intensity within the medullary cavity of the radius (asterisk) with periostitis along the radial shaft (arrowheads) manifested by linear bright signal intensity.
The imaging approach to the osteochondral injury, regardless of etiology, should be the same. The goal of imaging is first to diagnose the abnormality, then characterize it with regard to degree of involvement, stability of lesion, complications associated with the lesion, and finally to offer imaging information that may suggest acuity of the injury as well as etiology. Although MRI has been established as the most sensitive and reliable means for assessment of osteochondritis dissecans, radiographic evaluation routinely precedes MRI in the workup of elbow pain (79).
The radiographic detection of osteochondral lesions can be challenging. Some authors have suggested that obtaining anterior–posterior radiographs in 45 degrees of flexion can facilitate the radiographic detection of subtle lesions (79, 80). In general, the characteristic radiographic imaging appearance of an osteochondral lesion includes radiolucency and rarefaction of the osseous articular surface, most commonly the capitellum. Morphology changes of the articular surface can be present in the form of flattening and/or irregularity. The mineralization and appearance of the subchondral bone should be precisely characterized with particular attention to any areas of sclerosis, sclerosis with adjacent lucency, or subchondral cyst formation. Fragmentation at the articular surface or the presence of intra-articular bodies should be noted. It is the presence of subchondral bone sclerosis and lucency as well as fragmentation that suggest unstable lesions. The presence of associated findings such as effusion, osseous injury such as fracture, or soft tissue changes could be helpful in the delineation of acute versus chronic injury.
As previously noted, it is MRI that has emerged as the most sensitive and reliable means for the assessment of osteochondral lesions. The MRI diagnosis is made by identifying signal change or morphology abnormality at the articular surface. In general, signal intensity changes in the subchondral bone that are low on T1-weighted images without (a) fragmentation or (b) high signal intensity at the interface of the lesion to normal bone on fluid-sensitive sequences are considered stable in nature. The MRI signs of an unstable lesion include: (a) high-signal–intensity interface between the lesion and normal bone on fluid sensitive sequence; (b) a high-signal–intensity line through the articular cartilage in the region of the lesion; and (c) a focal articular surface defect (79).
Three basic types of lesions have been identified: stable, unstable but attached, and unstable and displaced. Stable lesions by definition are in situ and have intact articular cartilage. Unstable lesions are those in which the overlying articular cartilage is broken. The unstable lesion can remain attached and in situ or can detach and become displaced, intra-articular bodies. It is for this reason that MR arthrography has improved staging accuracy for osteochondral lesions (80). By placing contrast material into the articulation, both saline and dilute gadolinium solutions have been used, the presence of contrast within the interface between the fragment and normal bone establishes the presence of a break in the articular surface, there by establishing the presence of an unstable lesion (80–82).
The use of intravenous gadolinium-based contrast has also been described in the evaluation of stability and viability of osteochondral lesions. Fragment enhancement after intravenous contrast administration suggests an intact blood supply and, hence, viability of the fragment. Diffuse enhancement at the fragment–subchondral bone interface may indicate a loose fragment. If enhancing granulation tissue is present, then the fragment is assumed to be separated and therefore unstable by some authors (80, 83). We have little experience with the use of intravenous gadolinium-based contrast material for the detection of lesion stability and prefer to use MR arthrography for the assessment of lesion stability.
Osteochondral Injury
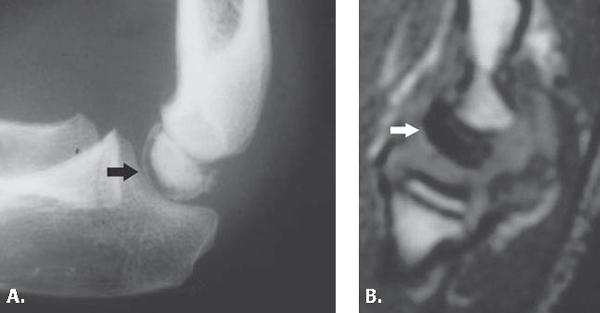
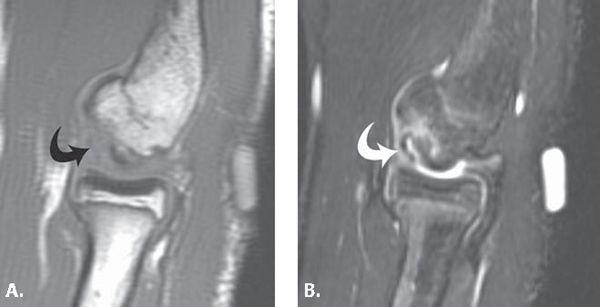
Panner’s Disease Osteochondrosis of the capitellum, so-called Panner’s disease, is the most common cause of chronic lateral elbow pain in the young athlete younger than age 10 years. Panner’s disease is a self-limited condition of the capitellum, often presenting with a dull, activity-related pain that quickly resolves with decreased activity. Minimal effusion and flexion contracture may be associated findings. On radiographs, rarefaction and fragmentation of a globally involved capitellar epiphysis is seen (84). Treatment of rest leads to a gradual restoration of symptoms and a relatively benign natural history. Regeneration and ossification of the epiphysis is eventually seen on radiographs with no residual deformity, joint collapse, or late sequelae (33). MRI findings have been described in this process and include low signal intensity on T1- and T2-weighted images throughout the entire capitellar ossification center. Fragmentation of the capitellum was also noted (Fig. 12.39) (85). This process must, however, be distinguished from osteochondritis dissecans of the capitellum, which has been described as more focal in nature, with a well-demarcated island of involvement and collapse.
Osteochondritis Dissecans The precise relationship of osteochondritis dissecans and osteochondral fracture is not clear, but most investigators regard the former condition as a posttraumatic abnormality that may lead to osteonecrosis. Its name is somewhat inaccurate in that it implies inflammation of the bone and cartilage, although no inflammatory cells have been shown on histologic sections of excised fragments or surrounding synovium (80, 86, 87). The term dissecans, however, comes from the Latin dissec (to separate) and accurately describes the pathology associated with this entity, the separation of a fragment of articular cartilage and bone from its donor site.
When occurring in the elbow, osteochondritis dissecans refers primarily to lesions of the anterior aspect of the capitellum, although lesions of the trochlea, radial head, olecranon, and olecranon fossa have been described (Figs. 12.40 and 12.41) (84). Osteochondritis dissecans occurs in immature athletes and is rarely found in adults. This entity has remained the center of much discussion and debate, principally as a result of controversy over its etiology, difficulty in its treatment, and poor long-term prognosis.
FIGURE 12.39 Panner’s disease. A: Lateral radiograph shows sclerosis of the capitellar ossification center (straight arrow) in a patient with elbow pain. B: T1-weighted sagittal MR image confirms the presence of diffuse low signal intensity throughout the capitellum (straight arrow) without fragmentation.
As previously noted, most authors agree that a combination of injury from repetitive trauma and a tenuous blood supply to the humeral capitellum leads to osteochondritis dissecans. The capitellar epiphysis receives blood from only one or two isolated vessels that enter posteriorly and traverse the capitellum. No metaphyseal collateral flow exists, resulting in a tenuous blood supply (80). This limits the ability of the epiphysis to heal between interim episodes of trauma, rendering it susceptible to osteonecrosis. Takahara et al. (88) discussed the natural progression of osteochondritis dissecans, emphasizing that the initial radiographic changes in this entity included localized subchondral bone flattening with thickening of the overlying cartilage. If allowed to heal, new bone formation occurs in the region of the subchondral morphologic change and over time unites with the underlying bone. If exposed to persistent, repetitive forces, the lesion progresses with fragmentation and potentially displacement.
As previously noted, this is an entity most commonly seen in adolescents and young adult males. Usually the dominant arm is affected and in most cases there is a history of overuse of the involved upper extremity. Common sports in which these patients participate are baseball, racquet sports, gymnastics, and weightlifting. Pain is the primary symptom at presentation. The onset of pain is insidious and progressive and, in most cases, tends to be activity-related. Often it is relieved by rest. Palpation of the radiocapitellar joint can elicit tenderness, but often this pain is dull and poorly localized. Another common finding is loss of motion, most commonly extension. If crepitus to palpation accompanies clicking, popping, or locking, the clinician should be highly suspicious of articular cartilage fragmentation and intra-articular body formation.
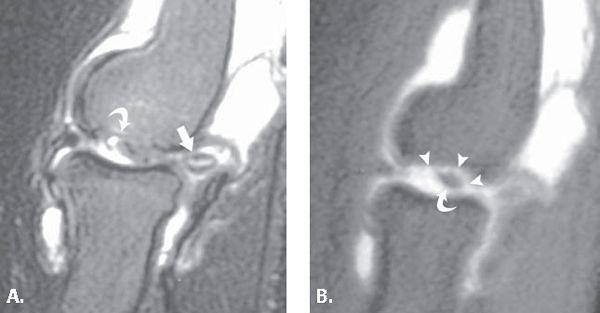
Central to the success of treatment of osteochondritis dissecans is fragment size, stability, viability, and location. Each of these should be considered and reported in the imaging assessment of the elbow. Lesion size, as determined by radiographic methods, has been associated with outcome (88, 89). Fragment stability, as noted previously, can be assessed with MRI (Fig. 12.42). Similarly, information regarding fragment viability can also be ascertained through the combination of MRI and the administration of intravenous gadolinium-based contrast material. This information is potentially useful because it could ultimately predict which lesions are likely to heal with nonoperative treatment. The location of the fragment is well accepted as occurring on the anterior capitellum, but concomitant radial head lesions have also been described and could affect both treatment and outcome (80, 90).
FIGURE 12.40 Osteochondritis dissecans of the trochlea. Frontal radiograph shows fragmentation of the trochlear ossification center (curved arrow) in a patient presenting with elbow pain. Although the ossification centers about the elbow can demonstrate variable appearance, the clinical history supports the diagnosis in this case.
FIGURE 12.41 Osteochondritis dissecans. A: T1- and B: T2-weighted fat-suppressed sagittal MR images of the elbow show an osteochondral irregularity at the capitellar surface with surrounding bone marrow edema (curved arrow). A region of linear high signal (curved arrow) on the T2-weighted image appears to undercut the articular surface suggesting that the lesion may be unstable.
Nonoperative treatment has been reserved for early lesions without mechanical symptoms and consists of cessation of the inciting trauma. It has been advised that return to sport is governed by symptoms, because imaging studies can remain abnormal for years (80). Surgical intervention has been implemented in those athletes with mechanical symptoms or obvious intraarticular bodies who have failed at least 6 months of nonoperative treatment. The predictors of a poor long-term outcome in patients with osteochondritis dissecans appear to be (a) large fragment size; (b) unstable lesion on presentation or progression of lesion severity over time; or (c) development of osteoarthritis (88).
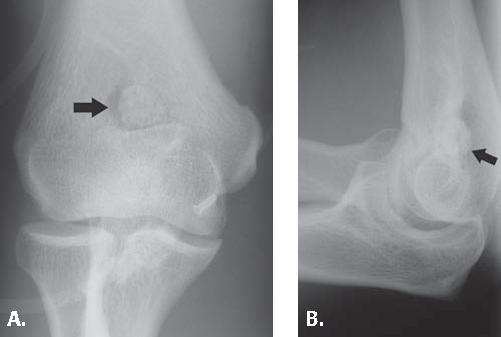
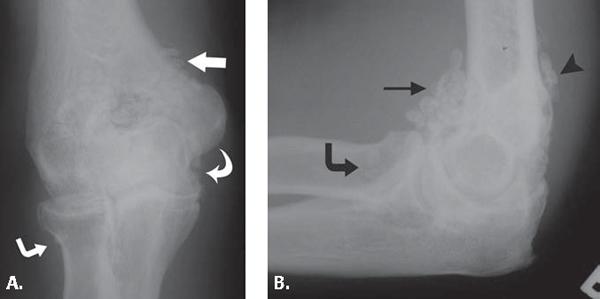
Intra-articular Bodies The elbow is the second most common site for intra-articular bodies (91). Any process that leads to damage of the articular surface of the elbow may result in the formation of cartilaginous or osteocartilaginous bodies (Fig. 12.43). Intra-articular bodies have been categorized based on origin: Category I listed as joint pathology related to articular-based disease such as osteoarthritis, inflammation, or infection; Category II related to trauma; and Category III related to synovial-based disease such as synovial chondromatosis (Fig. 12.44) (92). Cartilaginous or osteocartilaginous bodies may remain in situ, either partially detached or completely detached. When free, they can migrate and often collect in synovial recesses such as the coronoid and olecranon fossa, beneath the radial collateral or ulnar collateral ligament complexes. Most bodies have been localized to the anterior compartment; however, some activities such as overhead throwing predispose to body formation in the posterior compartment (91, 93). Bodies can also migrate within the joint (91, 94). If left in the joint, intra-articular bodies can grow as a result of the repetitive deposition of layers of fibrous and cartilaginous tissue (92).
FIGURE 12.42 Unstable osteochondral lesion. A: T2-weighted fat-suppressed sagittal MR image shows a region of osteochondral irregularity (curved arrow) at the capitellar articular surface. There appears to be an intra-articular body surrounded by joint fluid at the posterior aspect of the radiohumeral joint (arrow). B: T1-weighted fat-suppressed MR arthrogram image shows an in situ osteochondral lesion (curved arrow) with contrast entering into the plane between it and the native bone (arrowheads) consistent with an unstable fragment. The intra-articular body is again seen posterior to the radiohumeral joint.
FIGURE 12.43 Olecranon fossa intra-articular body. A: Frontal and B: lateral radiographs of the elbow show a large intra-articular body (arrow) in the olecranon fossa. This is a classic location for bodies within the elbow.
When detected, intra-articular bodies should be removed to resolve symptoms, prevent further articular damage as well as the development of osteoarthritis. Outcomes studies in patients undergoing elbow arthroscopy show the most benefit in the patient with intraarticular bodies who present with decreased range of motion, clicking, and locking (95–97). Elbow arthroscopy, however, is not without risk and has a complication rate reported between 0.1% and 15%, emphasizing the need for well-established indications before intervention (95–98). Limiting surgery to patients with confirmed intra-articular bodies avoids unnecessary expense and operative morbidity.
The imaging diagnosis of intra-articular bodies in the elbow begins with the radiograph. Several studies have demonstrated the fallibility of radiographs in the detection of intra-articular bodies in the elbow with both false-positive and false-negative studies reported (95, 97, 99). This is undoubtedly attributable in part to the complex osseous anatomy of this articulation as well as size variability of the bodies in question. In addition, osteophytes can be confused with bodies. One study demonstrated a 75% accuracy rate for detecting bodies with radiographs and 89% accuracy with conventional tomograms (97).
Brossmann et al. (100) explored the role of computed tomography, computed arthrotomography, MRI, and MR arthrography for the detection of osseous and cartilaginous intra-articular bodies in the knee (Figs. 12-45–12-47). They concluded that MR arthrography was the best imaging technique for detection of individual intraarticular bodies, emphasizing the spoiled gradient recalled acquisition in a steady state and T2-weighted sequences as the most accurate imaging sequences for this purpose. The accuracy of MR arthrography (92%) in the detection of osseous and cartilaginous bodies proved significantly better than that of standard MR imaging (57%–92%). Computed tomographic arthrography proved more accurate than standard MRI (82, 100, 101). Not only can MR arthrography delineate loose cartilage and bone in the joint, but it has the capability of identifying the donor site for the body as well as associated soft tissue findings that may exist.
Congenital Lesions
Radioulnar Synostosis
Congenital radioulnar synostosis is an uncommon disorder in which a developmental defect results in fusion of the proximal radioulnar joint of the forearm (Fig. 12.48). The forearm is usually fixed in pronation, often with diminished function. This disorder is familial in up to 20% of cases, most cases being diagnosed before the age of 5 years, although late-clinical–onset cases have been described (102). Two distinct types of radioulnar synostosis have been described. The first has been called a proximal or true radioulnar synostosis, in which the radius and ulna are fused smoothly at their proximal borders for a distance of 2 to 6 cm. In the second type, the fusion occurs just distal to the proximal radial epiphysis and is associated with congenital dislocation of the radial head (103). The fusion can take the form of a fibrous or complete osseous fusion (104).
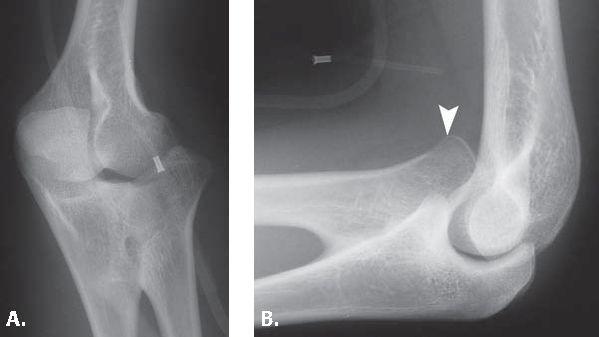
FIGURE 12.44 Synovial osteochondromatosis. A: Frontal and B: lateral radiographs of the elbow show multiple, small ossified bodies uniformly distributed throughout the elbow. They are in a recess beneath the ulnar collateral ligament (curved arrow), the annular ligament (angled arrow), the anterior humeral recess (arrow), the coronoid fossa (thin, straight arrow), and the olecranon fossa (arrowhead).
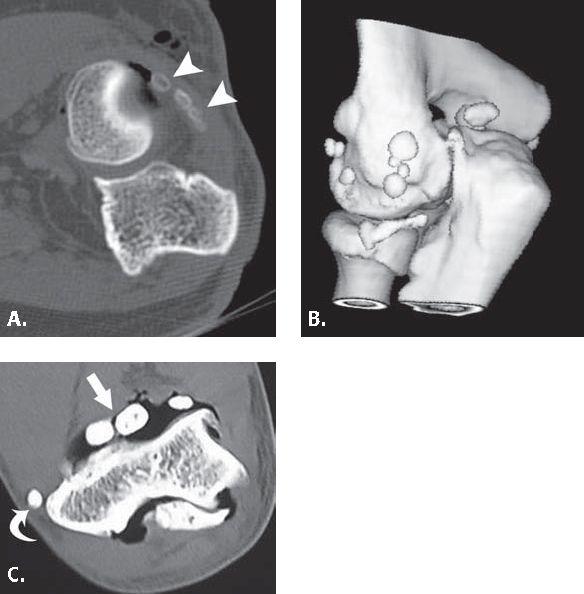
FIGURE 12.45 Computed tomography (CT) arthrography with air for intra-articular body evaluation. A: Axial CT image at the level of the proximal radioulnar joint after air arthrogram shows that the bodies within the posterior joint space are embedded within synovium (arrowheads). An arthroscopist looking for these bodies would be blinded to their location as a result of their synovial covering. B: A three-dimensional surface-rendered reformat confirms this finding. C: Axial CT image after air arthrogram at the level of the elbow in another patient shows the intra-articular bodies (arrow) in the anterior joint space surrounded by air. Incidental note is made of calcification within the common extensor tendon (curved arrow).
This entity is caused during the seventh week of gestation by a failure of separation of the fused cartilage precursors of the radius and ulna (102). This arrested development results in a cartilaginous bridge between the bones that usually ossify. At 7 weeks, the fetal forearm is in a position of semipronation to full pronation, accounting for the fixed pronation usually present in this disorder. It is bilateral in up to 80% of cases.
Congenital radioulnar synostosis may be associated with other musculoskeletal abnormalities such as congenital hip dislocation, clubfeet, or diminutive or supernumerary thumb. Syndromes associated with this entity include Antley-Bixler syndrome (congenital synostosis of the elbow and the cranial suture), Klinefelter’s, fetal alcohol syndrome, and acrocephalopolysyndactyly (102, 105, 106).
FIGURE 12.46 Intra-articular body. Gradient recalled echo sagittal MR image through the elbow shows intra-articular bodies within the olecranon (arrow) and coronoid (curved arrow) fossae.
FIGURE 12.47 Intra-articular body with MR arthrogram. T1-weighted fat-suppressed sagittal MR arthrogram image shows multiple intra-articular bodies within the coronoid fossa (curved arrow) of the elbow surrounded by contrast material.
FIGURE 12.48 Congenital radioulnar synostosis. A: Oblique frontal and B: lateral radiographs of the elbow show mature bone fusion across the proximal aspect of the radius and ulna. In addition, there is dislocation (arrowhead) of the radial head.
Congenital Dislocation of the Radial Head
Congenital radial head dislocation is the most commonly identified congenital elbow abnormality (107). It can occur in isolation, bilaterally and in association with other inherited conditions (Fig. 12.49). In approximately 60% of cases, this entity is found in conjunction with other conditions such as lower extremity anomalies, scoliosis, mental retardation, and syndromes such as nail patella and Klippel-Feil syndrome. Children often present because family members note a bump on the lateral side of the elbow that proves to be painless. In adolescence, however, elbow discomfort develops and worsens with motion.
The mode of inheritance in both isolated cases as well as those occurring with other conditions is believed to be autosomal-dominant. Although previously debated in the literature, it is now well accepted that congenital radial head dislocation can occur both unilaterally and bilaterally (108–111).
It is generally believed that the prime pathologic insult in congenital dislocation of the radial head is failure of normal capitellum formation. Normal cartilaginous and osseous development is highly dependent on normal contact pressure between both sides of the joint. Hypoplasia of the capitellum may adversely affect the development of a normal radial head and radiocapitellar joint. The hypoplastic capitellum fails to capture the radial head, allowing it to migrate both proximally and anteriorly, laterally, or posteriorly. The altered dynamics of the proximal elbow joint with subsequent dislocation of the radial head result in abnormal development of the ulna, which is severely bowed and relatively short in relation to the radius. Overall, the forearm appears small and underdeveloped. The capitellum is hypoplastic and flattened, the ulna short with negative ulnar variance, and the radial head has a domed shape rather than concave articular surface. There may be mechanical erosion on the distal humerus where the radial head rests on it (107).
Because ossification of the capitellum and radial head is not complete until 5 years of age, other parameters must be used in the radiographic assessment of congenital radial head dislocation. The capitellum is the first epiphysis to ossify around the elbow, usually at approximately 2 years of age. Radial head ossification occurs during the fifth year. Before radial head ossification, dislocation of the radial head is confirmed by drawing a line along the shaft of the radius and noting whether it bisects the capitellum ossification center. The radial head most commonly dislocates posteriorly (65%) followed by anterior (18%) and lateral (17%) (103, 107). No reports have explored the use of MRI in this diagnosis.
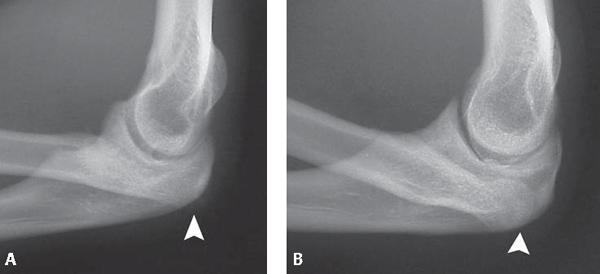
FIGURE 12.49 Congenital dislocation of the bilateral radial heads. Lateral radiographs of the A: right and B: left elbows show bilateral posterior radial head dislocation (arrowheads) with hypoplasia of the radial heads.
The standard treatment for congenital radial head dislocation is observation during childhood years. With the development of elbow pain, treatment options include excision of the radial head at skeletal maturity. This procedure has resulted in complications, most commonly wrist pain. An alternative technique involves reducing the radial head dislocation at an early age to avoid the complications of radial head excision and allow normal formation of the radiocapitellar joint. In so doing, the annular ligament is removed from the radiocapitellar joint, divided, and resutured around the radial head to achieve anatomic position (107).
References
1. Fowler KA, Chung CB. Normal MR imaging anatomy of the elbow. Magn Reson Imaging Clin N Am. 2004;12:191–206.
2. Rosenberg ZS, Beltran J, Cheung YY. Pseudodefect of the capitellum: potential MR imaging pitfall. Radiology. 1994;191:821–823.
3. Rosenberg ZS, Bencardino J, Beltran J. MR imaging of normal variants and interpretation pitfalls of the elbow. Magn Reson Imaging Clin N Am. 1997;5:481–499.
4. Rosenberg ZS, Bencardino J, Beltran J. MRI of normal variants and interpretation pitfalls of the elbow. Semin Musculoskelet Radiol. 1998;2:141–155.
5. Cotten A, Jacobson J, Brossmann J, et al. MR arthrography of the elbow: normal anatomy and diagnostic pitfalls. J Comput Assist Tomogr. 1997;21:516–522.
6. Rosenberg ZS, Beltran J, Cheung Y, et al. MR imaging of the elbow: normal variant and potential diagnostic pitfalls of the trochlear groove and cubital tunnel. AJR Am J Roentgenol. 1995;164:415–418.
7. Mallisee TA, Boynton MD, Erickson SJ, et al. Normal MR imaging anatomy of the elbow. Magn Reson Imaging Clin N Am. 1997;5:451–479.
8. Closkey RF, Goode JR, Kirschenbaum D, et al. The role of the coronoid process in elbow stability. A biomechanical analysis of axial loading. J Bone Joint Surg Am. 2000;82:1749–1753.
9. Cage DJ, Abrams RA, Callahan JJ, et al. Soft tissue attachments of the ulnar coronoid process. An anatomic study with radiographic correlation. Clin Orthop Relat Res. 1995;320:154–158.
10. Glajchen N, Schwartz ML, Andrews JR, et al. Avulsion fracture of the sublime tubercle of the ulna: a newly recognized injury in the throwing athlete. AJR Am J Roentgenol. 1998;170:627–628.
11. Pecina M, Boric I, Anticevic D. Intraoperatively proven anomalous Struthers’ ligament diagnosed by MRI. Skeletal Radiol. 2002;31:532–535.
12. Muller HA, Schild H. Diagnosis and therapy of capitulum humeri fractures [in German]. Unfallchirurgie. 1983;9:59–70.
13. Jupiter JB, Mehne DK. Fractures of the distal humerus. Orthopedics. 1992;15:825–833.
14. Farnsworth CL, Silva PD, Mubarak SJ. Etiology of supracondylar humerus fractures. J Pediatr Orthop. 1998;18:38–42.
15. De Boeck H, De Smet P, Penders W, et al. Supracondylar elbow fractures with impaction of the medial condyle in children. J Pediatr Orthop. 1995;15:444–448.
16. Pirone AM, Graham HK, Krajbich JI. Management of displaced extension-type supracondylar fractures of the humerus in children. J Bone Joint Surg Am. 1988;70:641–650.
17. Skaggs DL, Mirzayan R. The posterior fat pad sign in association with occult fracture of the elbow in children. J Bone Joint Surg Am. 1999;81:1429–1433.
18. Webb AJ, Sherman FC. Supracondylar fractures of the humerus in children. J Pediatr Orthop. 1989;9:315–325.
19. Flynn JC, Matthews JG, Benoit RL. Blind pinning of displaced supracondylar fractures of the humerus in children. Sixteen years’ experience with long-term follow-up. J Bone Joint Surg Am. 1974;56:263–272.
20. Millis MB, Singer IJ, Hall JE. Supracondylar fracture of the humerus in children. Further experience with a study in orthopaedic decision-making. Clin Orthop Relat Res. 1984;188: 90–97.
21. Sabharwal S, Tredwell SJ, Beauchamp RD, et al. Management of pulseless pink hand in pediatric supracondylar fractures of humerus. J Pediatr Orthop. 1997;17:303–310.
22. Bickel WE, Perry RE. Comminuted fractures of the distal humerus. JAMA. 1963;184:553–557.
23. Miller WE. Comminuted fractures of the distal end of the humerus in the adult. J Bone Joint Surg Am. 1964;46:644–657.
24. Gabel GT, Hanson G, Bennett JB, et al. Intraarticular fractures of the distal humerus in the adult. Clin Orthop Relat Res. 1987;216:99–108.
25. Riseborough EJ, Radin EL. Intercondylar T fractures of the humerus in the adult. A comparison of operative and non-operative treatment in twenty-nine cases. J Bone Joint Surg Am. 1969;51:130–141.
26. Henley MB. Intra-articular distal humeral fractures in adults. Orthop Clin North Am. 1987;18:11–23.
27. Knight RA. Fractures of the humeral condyles in adults. South Med J. 1955;48:1165–1173.
28. Milch H. Fractures and fracture dislocations of the humeral condyles. J Trauma. 1964;15:592–607.
29. Adams JE. Injury to the throwing arm. A study of traumatic changes in the elbow joints of boy baseball players. Calif Med. 1965;102:127–132.
30. Gugenheim JJ Jr, Stanley RF, Woods GW, et al. Little League survey: the Houston study. Am J Sports Med. 1976;4:189–200.
31. DaSilva MF, Williams JS, Fadale PD, et al. Pediatric throwing injuries about the elbow. Am J Orthop. 1998;27:90–96.
32. Larson RL, Singer KM, Bergstrom R, et al. Little League survey: the Eugene study. Am J Sports Med. 1976;4:201–209.
33. Klingele KE, Kocher MS. Little league elbow: valgus overload injury in the paediatric athlete. Sports Med. 2002;32:1005–1015.
34. Gill TJt, Micheli LJ. The immature athlete. Common injuries and overuse syndromes of the elbow and wrist. Clin Sports Med. 1996;15:401–423.
35. Hang DW, Chao CM, Hang YS. A clinical and roentgenographic study of Little League elbow. Am J Sports Med. 2004; 32:79–84.
36. Woods GW, Tullos HS. Elbow instability and medial epicondyle fractures. Am J Sports Med. 1977;5:23–30.
37. Ireland ML, Andrews JR. Shoulder and elbow injuries in the young athlete. Clin Sports Med. 1988;7:473–494.
38. Kocher MS, Waters PM, Micheli LJ. Upper extremity injuries in the paediatric athlete. Sports Med. 2000;30:117–135.
39. Farsetti P, Potenza V, Caterini R, et al. Long-term results of treatment of fractures of the medial humeral epicondyle in children. J Bone Joint Surg Am. 2001;83:1299–1305.
40. Anderson SE, Otsuka NY, Steinbach LS. MR imaging of pediatric elbow trauma. Semin Musculoskelet Radiol. 1998;2:185–198.
41. Wilson FD, Andrews JR, Blackburn TA, et al. Valgus extension overload in the pitching elbow. Am J Sports Med. 1983;11: 83–88.
42. Rettig AC. Traumatic elbow injuries in the athlete. Orthop Clin North Am. 2002;33:509–522, v.
43. Khurana JS, Kattapuram SV, Becker S, et al. Galeazzi injury with an associated fracture of the radial head. Clin Orthop Relat Res. 1988;234:70–71.
44. Hotchkiss RN, Weiland AJ. Valgus stability of the elbow. J Orthop Res. 1987;5:372–377.
45. Morrey BF, An KN. Articular and ligamentous contributions to the stability of the elbow joint. Am J Sports Med. 1983;11: 315–319.
46. Pribyl CR, Kester MA, Cook SD, et al. The effect of the radial head and prosthetic radial head replacement on resisting valgus stress at the elbow. Orthopedics. 1986;9:723–726.
47. Mason ML. Some observations on fractures of the head of the radius with a review of one hundred cases. Br J Surg. 1954;42:123–132.
48. Hotchkiss RN. Displaced fractures of the radial head: internal fixation or excision? J Am Acad Orthop Surg. 1997;5:1–10.
49. Broberg MA, Morrey BF. Results of delayed excision of the radial head after fracture. J Bone Joint Surg Am. 1986;68:669–674.
50. O’Dwyer H, O’Sullivan P, Fitzgerald D, et al. The fat pad sign following elbow trauma in adults: its usefulness and reliability in suspecting occult fracture. J Comput Assist Tomogr. 2004; 28:562–565.
51. Shmueli G, Herold HZ. Compression screwing of displaced fractures of the head of the radius. J Bone Joint Surg Br. 1981;63:535–538.
52. McKay PL, Katarincic JA. Fractures of the proximal ulna olecranon and coronoid fractures. Hand Clin. 2002;18:43–53.
53. Morrey BF. Current concepts in the treatment of fractures of the radial head, the olecranon, and the coronoid. Instr Course Lect. 1995;44:175–185.
54. Karlsson MK, Hasserius R, Karlsson C, et al. Fractures of the olecranon: a 15- to 25-year followup of 73 patients. Clin Orthop Relat Res. 2002;403:205–212.
55. Regan W, Morrey B. Fractures of the coronoid process of the ulna. J Bone Joint Surg Am. 1989;71:1348–1354.
56. Salvo JP, Rizio L 3rd, Zvijac JE, et al. Avulsion fracture of the ulnar sublime tubercle in overhead throwing athletes. Am J Sports Med. 2002;30:426–431.
57. Conway JE, Jobe FW, Glousman RE, et al. Medial instability of the elbow in throwing athletes. Treatment by repair or reconstruction of the ulnar collateral ligament. J Bone Joint Surg Am. 1992;74:67–83.
58. Parr TJ, Burns TC. Overuse injuries of the olecranon in adolescents. Orthopedics. 2003;26:1143–1146.
59. Aoki Y, Yasuda K, Tohyama H, et al. Magnetic resonance imaging in stress fractures and shin splints. Clin Orthop Relat Res. 2004;421:260–267.
60. Engber WD. Stress fractures of the medial tibial plateau. J Bone Joint Surg Am. 1977;59:767–769.
61. Sullivan D, Warren RF, Pavlov H, et al. Stress fractures in 51 runners. Clin Orthop Relat Res. 1984;187:188–192.
62. Martin SD, Healey JH, Horowitz S. Stress fracture MRI. Orthopedics. 1993;16:75–78.
63. Stafford SA, Rosenthal DI, Gebhardt MC, et al. MRI in stress fracture. AJR Am J Roentgenol. 1986;147:553–556.
64. Lee JK, Yao L. Stress fractures: MR imaging. Radiology. 1988;169:217–220.
65. Froelich JW. Imaging of fractures: stress and occult. J Rheumatol. 1991;18:4–6.
66. Slocum DB. Classification of elbow injuries from baseball pitching. Tex Med. 1968;64:48–53.
67. King J, Brelsford HJ, Tullos HS. Analysis of the pitching arm of the professional baseball pitcher. Clin Orthop Relat Res. 1969;67:116–123.
68. Suzuki K, Minami A, Suenaga N, et al. Oblique stress fracture of the olecranon in baseball pitchers. J Shoulder Elbow Surg. 1997;6:491–494.
69. Chan D, Aldridge MJ, Maffulli N, et al. Chronic stress injuries of the elbow in young gymnasts. Br J Radiol. 1991;64:1113–1118.
70. Fines BP, Stacy S. Stress fracture of the ulna in an adolescent baton twirler. Skeletal Radiol. 2002;31:116–118.
71. Chen FS, Rokito AS, Jobe FW. Medial elbow problems in the overhead-throwing athlete. J Am Acad Orthop Surg. 2001; 9:99–113.
72. Petschnig R, Wurnig C, Rosen A, et al. Stress fracture of the ulna in a female table tennis tournament player. J Sports Med Phys Fitness. 1997;37:225–227.
73. Brukner P. Stress fractures of the upper limb. Sports Med. 1998;26:415–424.
74. Farquharson-Roberts MA, Fulford PC. Stress fracture of the radius. J Bone Joint Surg Br. 1980;62:194–195.
75. Ahluwalia R, Datz FL, Morton KA, et al. Bilateral fatigue fractures of the radial shaft in a gymnast. Clin Nucl Med. 1994; 19:665–667.
76. Eisenberg D, Kirchner SG, Green NE. Stress fracture of the distal radius caused by ‘wheelies.’ South Med J. 1986;79:918–919.
77. Loosli AR, Leslie M. Stress fractures of the distal radius. A case report. Am J Sports Med. 1991;19:523–524.
78. Orloff AS, Resnick D. Fatigue fracture of the distal part of the radius in a pool player. Injury. 1986;17:418–419.
79. Takahara M, Shundo M, Kondo M, et al. Early detection of osteochondritis dissecans of the capitellum in young baseball players. Report of three cases. J Bone Joint Surg Am. 1998;80: 892–897.
80. Bradley JP, Petrie RS. Osteochondritis dissecans of the humeral capitellum. Diagnosis and treatment. Clin Sports Med. 2001;20:565–590.
81. Fritz RC. MR imaging of osteochondral and articular lesions. Magn Reson Imaging Clin N Am. 1997;5:579–602.
82. Steinbach LS, Palmer WE, Schweitzer ME. Special focus session. MR arthrography. Radiographics. 2002;22:1223–1246.
83. Peiss J, Adam G, Casser R, et al. Gadopentetate-dimeglumine–enhanced MR imaging of osteonecrosis and osteochondritis dissecans of the elbow: initial experience. Skeletal Radiol. 1995;24:17–20.
84. Stubbs MJ, Field LD, Savoie FH 3rd. Osteochondritis dissecans of the elbow. Clin Sports Med. 2001;20:1–9.
85. Stoane JM, Poplausky MR, Haller JO, et al. Panner’s disease: x-ray, MR imaging findings and review of the literature. Comput Med Imaging Graph. 1995;19:473–476.
86. Schenck RC Jr, Goodnight JM. Osteochondritis dissecans. J Bone Joint Surg Am. 1996;78:439–456.
87. Nagura S. Osteochondritis dissecans of the hip joint and its etiology [in German]. Arch Orthop Unfallchir. 1969;65:371–374.
88. Takahara M, Ogino T, Takagi M, et al. Natural progression of osteochondritis dissecans of the humeral capitellum: initial observations. Radiology. 2000;216:207–212.
89. Takahara M, Ogino T, Sasaki I, et al. Long term outcome of osteochondritis dissecans of the humeral capitellum. Clin Orthop Relat Res. 1999;363:108–115.
90. Janarv PM, Hesser U, Hirsch G. Osteochondral lesions in the radiocapitellar joint in the skeletally immature: radiographic, MRI, and arthroscopic findings in 13 consecutive cases. J Pediatr Orthop. 1997;17:311–314.
91. Miller JH, Beggs I. Detection of intraarticular bodies of the elbow with saline arthrosonography. Clin Radiol. 2001;56: 231–234.
92. Attarian DE, Guilak F. Observations on the growth of loose bodies in joints. Arthroscopy. 2002;18:930–934.
93. Andrews JR, Timmerman LA. Outcome of elbow surgery in professional baseball players. Am J Sports Med. 1995;23:407–413.
94. Ogilvie-Harris DJ, Schemitsch E. Arthroscopy of the elbow for removal of loose bodies. Arthroscopy. 1993;9:5–8.
95. O’Driscoll SW. Elbow arthroscopy for loose bodies. Orthopedics. 1992;15:855–859.
96. O’Driscoll SW, Morrey BF. Arthroscopy of the elbow. Diagnostic and therapeutic benefits and hazards. J Bone Joint Surg Am. 1992;74:84–94.
97. Quinn SF, Haberman JJ, Fitzgerald SW, et al. Evaluation of loose bodies in the elbow with MR imaging. J Magn Reson Imaging. 1994;4:169–172.
98. Lynch GJ, Meyers JF, Whipple TL, et al. Neurovascular anatomy and elbow arthroscopy: inherent risks. Arthroscopy. 1986; 2:190–197.
99. Boe A, Molster A. Arthroscopy of the elbow [in Norwegian]. Tidsskr Nor Laegeforen. 1992;112:493–494.
100. Brossmann J, Preidler KW, Daenen B, et al. Imaging of osseous and cartilaginous intraarticular bodies in the knee: comparison of MR imaging and MR arthrography with CT and CT arthrography in cadavers. Radiology. 1996;200:509–517.
101. Chandnani VP, Harper MT, Ficke JR, et al. Chronic ankle instability: evaluation with MR arthrography, MR imaging, and stress radiography. Radiology. 1994;192:189–194.
102. Guma M, Teitel AD. Adolescent presentation of congenital radioulnar synostosis. Clin Pediatr (Phila). 1996;35:215–217.
103. Mital MA. Congenital radioulnar synostosis and congenital dislocation of the radial head. Orthop Clin North Am. 1976;7:375–383.
104. Cleary JE, Omer GE Jr. Congenital proximal radioulnar synostosis. Natural history and functional assessment. J Bone Joint Surg Am. 1985;67:539–545.
105. Kitoh H, Nogami H, Oki T, et al. Antley-Bixler syndrome: a disorder characterized by congenital synostosis of the elbow joint and the cranial suture. J Pediatr Orthop. 1996;16:243–246.
106. Okrent DH, McFadden JC. Radiologic case study. Congenital radioulnar synostosis. Orthopedics. 1986;9:1452, 1455–1456.
107. Sachar K, Mih AD. Congenital radial head dislocations. Hand Clin. 1998;14:39–47.
108. Mizuno K, Usui Y, Kohyama K, et al. Familial congenital unilateral anterior dislocation of the radial head: differentiation from traumatic dislocation by means of arthrography. A case report. J Bone Joint Surg Am. 1991;73:1086–1090.
109. Miura T. Congenital dislocation of the radial head. J Hand Surg (Br). 1990;15:477–481.
110. Kelly DW. Congenital dislocation of the radial head: spectrum and natural history. J Pediatr Orthop. 1981;1:295–298.
111. Agnew DK, Davis RJ. Congenital unilateral dislocation of the radial head. J Pediatr Orthop. 1993;13:526–528.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree