Figure 23.1 Inflicted fracture and neglect in a disabled child. AP view of the humerus in a one-year-old child with Down syndrome receiving physical therapy for spasticity demonstrates a mature callus about the humeral shaft. The pattern is consistent with both proximal epiphyseal separation and extensive subperiosteal hemorrhage. Widespread skeletal injuries involving the long bone shafts and metaphyses, typical of abuse, were identified. (Courtesy of Walter Berdon MD.)
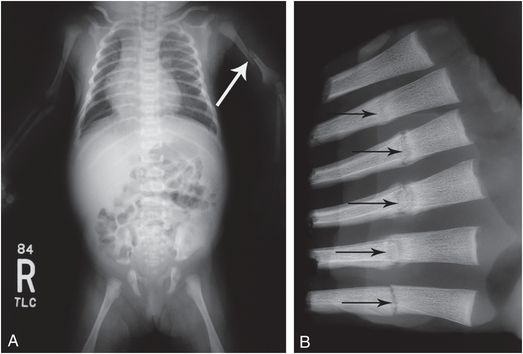
Figure 23.2 Down syndrome – missed abuse fatality. At 19 days the infant presented with a left humeral fracture. A, The “babygram” is very limited, but does show the acute left humeral fracture (arrow). The infant died at two months of age with a fatal head injury. B, Specimen radiograph of the left third-to-eighth anterolateral ribs demonstrates multiple healing fractures (arrows), not evident on the earlier study. The father, who reportedly resented the child, allegedly struck the infant multiple times. There were also posteromedial rib fractures and CMLs (not shown).
Children with osteogenesis imperfecta (OI) suffer fractures due to increased bone fragility (see Chapter 9). They may also be victims of abuse, but it can be difficult to differentiate inflicted fractures from those occurring with normal activity, accidents, and, occasionally, birth trauma (34) Figure 23.3 illustrates a child with OI who died from head injuries. The mother admitted to fatally injuring the child, as well as shaking her other normal infant.
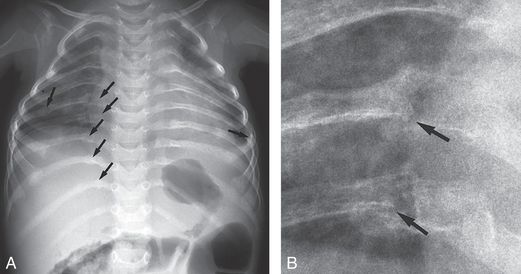
Figure 23.3 Abuse and OI. A, Postmortem AP view of the chest in a 1½-year-old child with type I OI demonstrates gracile ribs with multiple fractures (arrows). B, Magnified view of the right seventh and eighth ribs shows healing fractures near the costovertebral junctions (arrows). Additional rib fractures as well as intracranial injuries were found at postmortem examination. The mother admitted to swinging the child into a stove, causing the fatal injuries.
Physical abuse is particularly difficult to diagnose in institutionalized children (35, 36). Differentiation from accidental or self-induced injury is often impossible without a witness or admission of the abuser. This problem is evident in the case shown in Fig. 23.4, which illustrates the imaging findings in an institutionalized, neurologically disabled patient who developed vomiting and dehydration. An upper gastrointestinal (UGI) series and abdominal sonogram revealed evidence of a duodenal hematoma. There was no history of injury, and the origin of this lesion was presumed but not confirmed to be due to occult inflicted trauma.
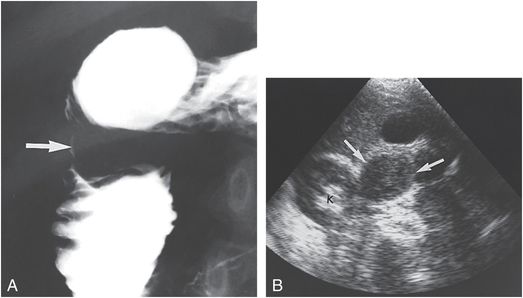
Figure 23.4 Duodenal hematoma in an institutionalized patient. Seventeen-year-old mentally retarded patient presented with intermittent vomiting for 10 days. A, An UGI series demonstrates evidence of fold thickening and an intraluminal mass (arrow) in the second portion of the duodenum. B, A transverse abdominal sonogram shows a well-defined echogenic mass (arrows) anterior and medial to the right kidney (k). A follow-up sonogram revealed the mass to be smaller and hypoechoic, consistent with a liquefying hematoma. An occult injury was suspected but never documented.
Neglect
More children are at risk of neglect more than any other form of child maltreatment. Infants and toddlers are particularly prone to suffer neglect than other forms of maltreatment and they are also at the greatest risk of death due to maltreatment. There is strong evidence that neglected infants and toddlers are exposed to greater environmental dangers, which may pose adverse consequences later in life (14, 37–39).
Nonorganic failure to thrive
Failure to thrive (FTT) is a significantly prolonged cessation of appropriate weight gain compared with recognized norms for age and gender after having achieved a stable pattern (40). Nonorganic FTT is the lack of normal growth and development secondary to a disturbed social and emotional environment. Although this condition is differentiated from organic FTT, in which a serious medical condition results in disturbed growth and development, it is clear that these two forms frequently overlap (40). An in-depth discussion of these forms of FTT is beyond the scope of this text; the reader is referred to several discussions of this subject in the overall context of child abuse and neglect, as well as a number of important focused articles (40–44).
From an imaging perspective, it is useful to consider a specific type of nonorganic FTT characterized by reversible pituitary and hypothalamic dysfunction. A variety of terms have been used to describe this condition, including the syndrome of maternal deprivation, psychosocial dwarfism, psychosocial short stature, deprivational dwarfism, abuse dwarfism, and the Kasper–Hauser syndrome (45–61). Classically, these children show unusual eating habits, depression, self-mutilation, sleep disturbances, lack of response to pain, enuresis, encopresis, and poor performance on cognitive tests. The condition is commonly thought to reflect the lack of a positive mother–child relationship. All the symptoms, including deficient IQ and delayed puberty, may be reversible with a positive change of environment (52).
A variety of radiologic findings have been described. The most frequent abnormalities are retarded bone age, osteopenia, and diminished subcutaneous fat. Classically, the delay in bone age is commensurate with the abnormal height age (62, 63). Retarded skeletal maturation is secondary to decreased somatotropin secretion, which simulates idiopathic hypopituitarism of organic origin. However, growth hormone secretion returns to normal when the children are removed from their abnormal home environment. Multiple parameters of “catch-up” growth are most apparent in the three months immediately following placement in foster care (64). Transient hypopituitarism should be differentiated from irreversible hypothalamic–pituitary dysfunctions secondary to traumatic head injury associated with abusive assaults (65, 66).
Capitanio and Kirkpatrick (67) noted widening of the cranial sutures in a group of children undergoing treatment for psychosocial dwarfism (Fig. 23.5). The radiologic features suggested increased intracranial pressure, but the authors noted no abnormal neurologic findings. The enlarging head circumference (HC) paralleled the accelerated growth period. The authors concluded that similar rapid growth of the brain resulted in splitting of the cranial sutures. Other investigators have confirmed Capitanio and Kirkpatrick’s observations (68–73).
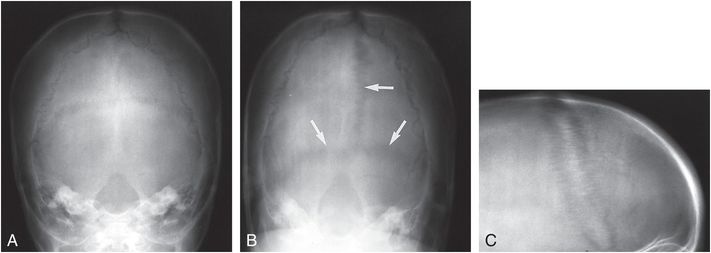
Figure 23.5 Split cranial sutures with reversiable somatatropin deficiency. A, Towne’s projection of the skull in a 2½-year-old child with FTT reveals normal sutures. Repeat Towne’s (B), and coned lateral (C), views 81 days after hospitalization demonstrate split sutures (arrows). (From Sondheimer FK, Grossman H, Winchester P. Suture diastasis following rapid weight gain: pseudopseudotumor cerebri. Arch Neurol. 1970 23:314–18.)
The age at which the sutural widening is noted ranges from 10 weeks to 6 years. It is most frequently discovered around two years of age, at which time psychosocial dwarfism is recognized and treated. The sutures are characteristically normal at diagnosis, and sutural widening becomes evident once considerable weight gain occurs. Occasionally, however, the sutures may be wide at diagnosis (71). The sutural widening is generalized and varies from a slight diastasis to 4 mm of separation of the bony margins. The appearance of the sutures can be expected to return to normal in 2–3 months. The rapid increase in HC and sutural widening may suggest post-traumatic increased intracranial pressure due to subdural hematoma (SDH) or communicating hydrocephalus. Computed tomography (CT) or magnetic resonance imaging (MRI) should allow differentiation.
Other manifestations of neglect
Another unusual phenomenon that occurs in neglected children is acute gastric distention (74–76). These patients are usually below the third percentile in height and weight and have a voracious appetite. Marked upper abdominal distention is noted that may simulate hepatosplenomegaly or some other intra-abdominal mass. A supine view of the abdomen supports the presence of an upper abdominal mass, and an upright or cross-table lateral view usually reveals an air–fluid level (Fig. 23.6). This entity is a form of gastric atony that occurs in a variety of states, including chronic starvation. It appears to be due to structural and functional changes in the stomach secondary to inadequate nutrition, and classically develops after ingestion of a large meal. Gastric rupture in physically abused children typically occurs with large amounts of gastric contents after ingestion of a meal. Thus, it is possible that gastric atony and distention may predispose to gastric rupture after a blunt abdominal blow. Gastric distention also occurs with duodenal hematoma, and an UGI series, CT, or sonography will differentiate gastric atony from mechanical obstruction (see Chapter 22).
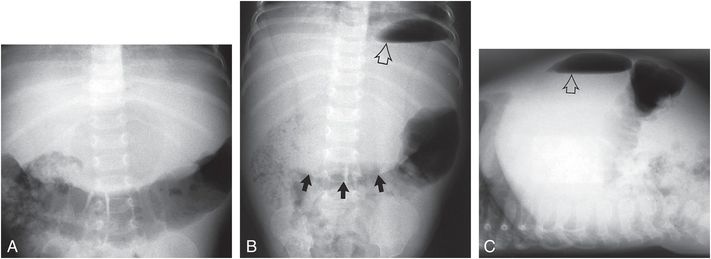
Figure 23.6 Acute gastric dilation. Supine (A), upright (B), and cross-table lateral (C) views of the abdomen in a five-month-old infant presenting with an upper abdominal mass. The infant, who was below the third percentile in height and weight, had recently ingested a large meal. The markedly dilated stomach produces a soft tissue mass (solid arrows) containing an air–fluid level (open arrow) in the middle and upper abdomen.
On occasion, well-intentioned parents may institute a variety of cult diets resulting in nutritional disturbances. In addition to kwashiorkor and marasmus, rickets has been described in infants and children placed on fad diets (77–79). A particularly difficult problem arises in the child with nutritional rickets. The imaging features may be strikingly manifest in multiple siblings (Fig. 23.7). When severe osteopenia is present, it may predispose to fracture, and it can be difficult to differentiate fractures occurring spontaneously due to weakened osseous structures from those with superimposed physical abuse (see Chapter 8). Widespread injuries at non-weight-bearing locations, such as the forearms and hands, are highly suspicious, particularly when fractures are encountered in a healing phase (Fig. 23.8). Profound nutritional deficiency may result, with overt physical consequences. Failure to address the child’s illness may constitute neglect, and cases of fatalities due to starvation associated with abusive injuries continue to be reported (Fig. 23.9) (80, 81). Mateju et al. described fatal neglect in a 46-month old-girl with Rapunzel syndrome, a rare and extreme form of trichobezoar formation, extending from the stomach to the small intestine (82). Fukunaga et al. have suggested that immunodeficiency secondary to neglect may have contributed to overwhelming sepsis and death in a six-year-old child with thymic involution and T/B-cell deficiency (83). A somewhat similar case has been described by Senati et al. (84).
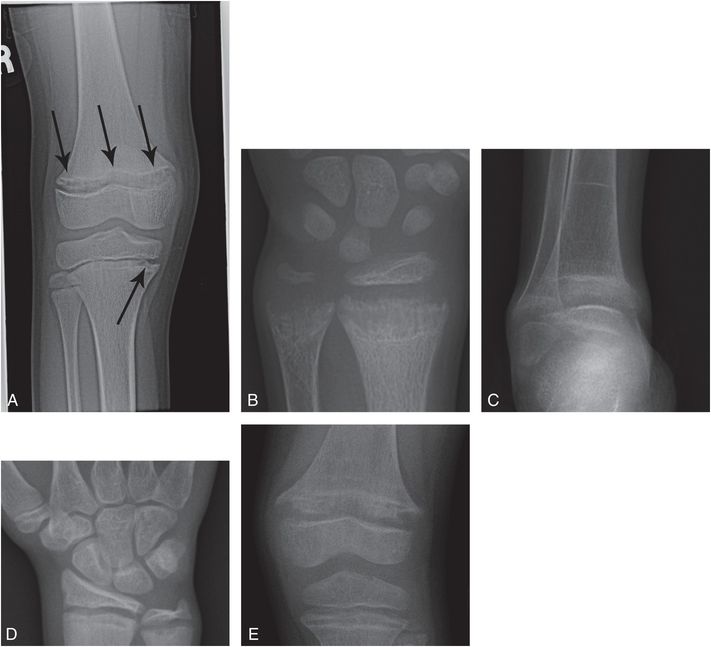
Figure 23.7 Nutritional rickets in multiple siblings. Nine-year-old brought to the ER following an episode of syncope. Total serum calcium was 5.5 mg/dL; ionized calcium was 4.5 mg/dL. Serum phosphate was normal; alkaline phosphatase was 606 U/L. A, AP radiograph of the right knee reveals widening and irregularity (arrows) of the distal femoral physis with less evident changes in the proximal tibia. PA view of the left wrist (B) and AP view of the right ankle (C) in the 7-year-old sibling, PA view of the right wrist (D) in the 12-year-old sibling and an AP view of the left knee (E) in the 6-year-old sibling all show varying degrees of physeal widening and irregularity characteristic of rickets. The index child and the siblings all had chemical evidence of rickets and were all on a rigid unsupplemented vegan diet. The parents refused admission and left the ER against medical advice. The Department of Youth Services determined neglect and placed the children in foster care.
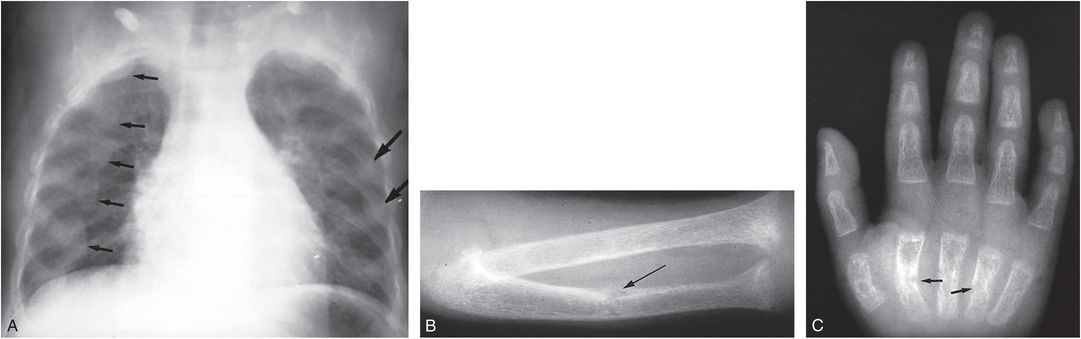
Figure 23.8 Dietary rickets with superimposed fractures. A, Frontal view of the chest in a 20-month-old child of Rastafarian parents who was confined indoors. There is diffuse demineralization; widening of the ends of the ribs, producing a “ricketic rosary” (small arrows); and healing rib fractures (large arrows). B, A view of the forearm demonstrates demineralization, cupping of the metaphyses, and loss of the normal dense zone of provisional calcification indicating rickets. A healing fracture of the ulna is noted (arrow). C, A view of the hand shows diffuse demineralization and healing metacarpal fractures (arrows). At a minimum, these findings point to neglect, and superimposed traumatic injury should be suspected. (Courtesy of Paul A. Nancarrow MD.)
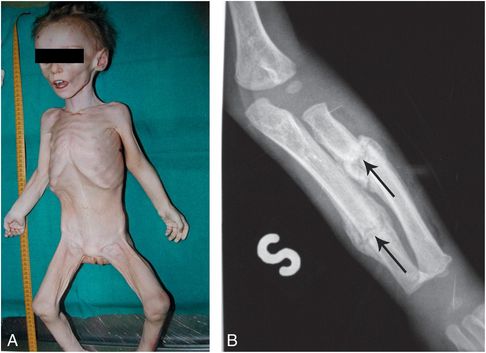
Figure 23.9 Starvation associated with abusive injuries. Sixteen-month-old female found unconscious by her stepfather and subsequently dead on arrival to the ER. The body was cachectic with multiple bruises. The mother stated that the child had not been “eating well” that week, A, View of the victim prior to autopsy shows severe wasting. B, Frontal radiograph of the left forearm shows radial and ulnar diaphyseal fractures (arrows) with hard callus/SPNBF. (From Solarino B, Grattagliano I, Catanesi R, Tsokos M. Child starvation and neglect: a report of two fatal cases. J Forensic Leg Med. 2012;19:171–4.)
As indicated earlier, mixed forms of organic and inorganic FTT are well described (85), and any physical disorder may be complicated by neglect. This can result in exacerbation of the primary manifestations of the disease or produce atypical features. Indications of overt physical abuse and neglect may also be superimposed upon imaging features of the underlying organic disorder (86). Celiac disease has been associated with neglect and abuse (87, 88). Neglect of ulcerative colitis resulted in the death of a 15½-year-old-girl (89). However, care must be taken to avoid a misdiagnosis of abuse based on the primary signs of GI disorders (61, 90). The case complexities demand a multidisciplinary approach to these forms of child maltreatment and their mimics.
Lastly, injuries and deaths to children from attacks by dogs and other potentially aggressive pets may constitute neglect, and on occasion the assaults may be accompanied by imaging abnormalities, particularly in infants and young children. It may be difficult to differentiate antemortem from postmortem canine injuries (91, 92).
Poisoning and orally inserted foreign bodies
Intentional childhood poisoning can occur in a variety of clinical settings. Harmful substances and objects may be administered with a clear attempt to injure the child or to produce a factitious disease leading to medical attention, falling within the spectrum of Munchausen syndrome by proxy (see below) (93–110).
Foreign body administration may result in dramatic alterations on imaging studies. As noted in Chapter 22, the mouth is often the target of a physical assault (111), and some may entail insertion of a digit or other sharp object that causes pharyngeal or esophageal perforation. A wide variety of objects and foreign substances may be introduced through the mouth and result in acute illness. Medical attention may be delayed, and when care is sought, diagnosis may be obscured owing to misleading or inadequate history. Furthermore, symptoms related to the foreign bodies may resolve, and the objects may be discovered incidentally during the imaging evaluation for suspected natural illness.
Coin ingestions are well-described accidental events in older infants and young children. When encountered in young infants, they should be regarded as suspicious for abuse (95–97, 103). From experience with accidental ingestions, it is clear that coins may be present for days or even weeks with only modest symptoms. The infant may take liquid feedings normally and symptoms may become apparent only as the coins begin to erode the esophageal mucosa. This results in edema within the esophageal wall and surrounding tissues, producing feeding difficulties and increased secretions due to esophageal obstruction. Esophageal foreign bodies may produce mainly respiratory symptoms on presentation, in particular, inspiratory stridor. The site of impaction is usually at the thoracic inlet or at the level of the aortic arch. Nolte noted multiple coins in a infant who subsequently died (Fig. 23.10) (103). Coins were first identified and removed at 4½ months of age, but abuse was not suspected. The child died one month later, and additional coins were found at multiple levels in the esophagus with evidence of esophageal injury. The precise cause of death was unclear, but the case was judged to be a homicide. In the older infant and young child foreign body ingestions are usually voluntary; care should be taken to avoid assignment of an abusive etiology to the serious and sometimes fatal consequences of coin ingestion. Dahiya and Denton reported a three-year-old boy who died from exsanguination due to an esophago-aortic fistula (112). At autopsy, a coin which was lodged posteriorly in the esophagus had eroded into the aorta. Based on the initial presentation, child abuse was suspected, but there was no other evidence to support that consideration and the death was considered accidental.
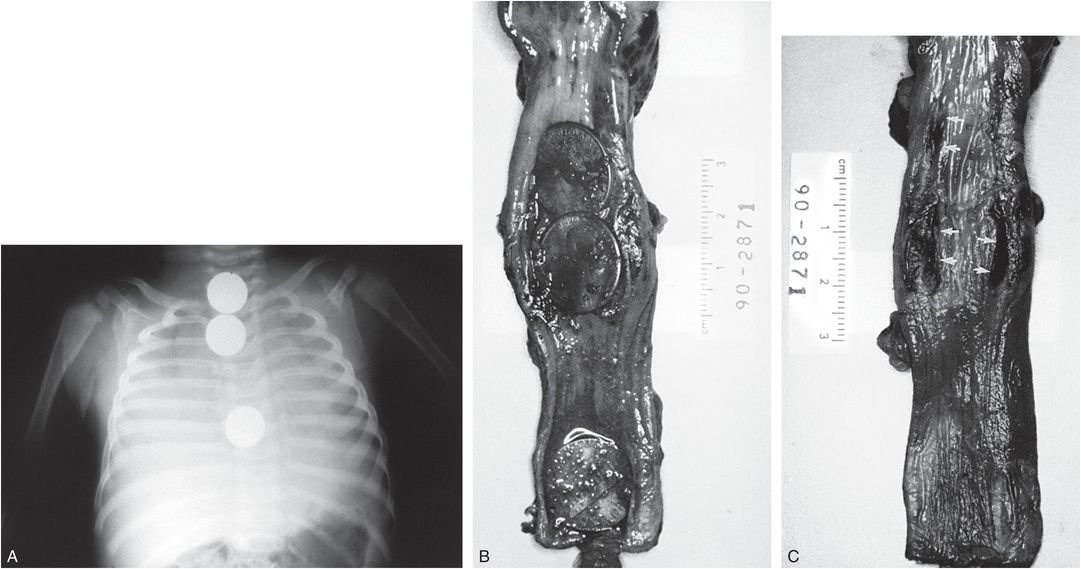
Figure 23.10 Esophageal foreign bodies. A, A postmortem chest radiograph shows three coins in the esophagus. B, A specimen shows three pennies in the esophagus. C, With the coins removed, shallow esophageal ulcers are apparent (arrows). (From Nolte KB. Esophageal foreign bodies as child abuse: potential fatal mechanisms. Am J Forensic Med Pathol. 1993;14:323–6.)
Baker and Berdon described a variety of foreign bodies, including safety pins and a light bulb, in a child with multiple healing fractures (Fig. 23.11) (93). The mother was an alcoholic and was reported to have assaulted the child only during episodes of intoxication. Friedman reported a six-month-old infant who had been fed multiple foreign bodies, including a thumb tack, a screw, and a carpet tack (98). In a more recent case, Medatwal et al. described endoscopic removal of a coin, safety pin, screw, cotton ball, plastic fragment, and four pieces of glass from the esophagus, and extraction of a gastric glass fragment from a 12-day-old infant (108). Several additional glass fragments were recovered from the stool. The infant subsequently deteriorated and died. The attendants and relatives denied “deliberate introduction of foreign bodies in the mouth of the newborn.” Wadhera et al. described a two-year-old with a bolt in the pharynx and two nuts in the abdomen (113). The bolt was removed by rigid hypopharyngoscopy, but the abdominal foreign bodies passed spontaneously. The mother admitted that she had pushed three foreign bodies into the throat of the child, due to marital conflict.
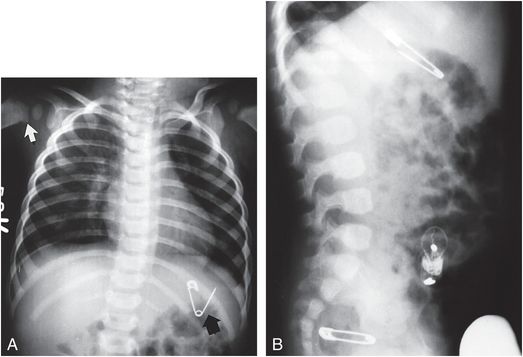
Figure 23.11 Poisoning by foreign bodies. A, A supine chest view of an abused child with a fractured humerus (white arrow) shows an open safety pin within the stomach (black arrow). B, Lateral view of the abdomen also demonstrates a light bulb, and a closed safety pin in the rectum. The mother had reportedly fed the child these foreign bodies during periods of intoxication. (From Baker DH, Berdon WE. Special trauma problems in children. Radiol Clin North Am. 1966;4:289–305.)
Orally inserted foreign bodies that have extended through the oropharyngeal wall may migrate into the adjacent soft tissues. Bakshi et al. described a seven-month-old girl with respiratory distress with a rounded opacity evident radiographically in the parapharyngeal region (Fig. 23.12) (106). At endoscopy, a chronic mucosal rent at the level of the cricoid was noted. Subsequent surgical exploration revealed a marble in the parapharyngeal soft tissues. The authors concluded that the foreign body had been forcefully inserted by the father who resented the child. Although orally inserted foreign bodies usually end up in the GI tract or surrounding soft tissues, a foreign body may rarely lodge in the tracheobronchial tree. Wadhera and others described a sharp metallic foreign body in the right main stem bronchus of an infant with cough and respiratory distress (Fig. 23.13) (109). A nail was removed at bronchoscopy. After initial denial, the mother admitted that she had pushed a nail in the throat of the child following a “tiff” with her husband.
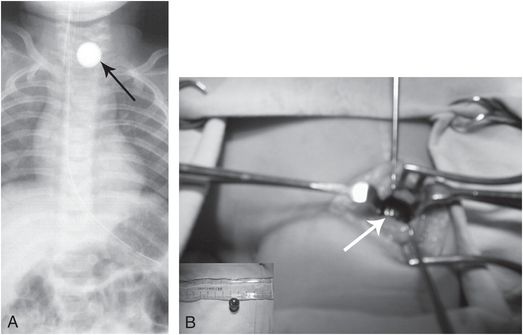
Figure 23.12 Migratory foreign body in neck. Seven-month-old with respiratory distress. A, Frontal radiograph of the chest reveals a rounded foreign body (arrow) above the thoracic inlet. B, Intraoperative photograph showing 1.5 cm diameter marble at level of cricoid (arrow) lying deep to the strap muscles. The marble had passed through a rent in the hypopharynx into the parapharyngeal soft tissues. (From Bakshi J, Verma RK, Karuppiah S. Migratory foreign body of neck in a battered baby: a case report. Int J Pediatr Otorhinolaryngol. 2009;73:1814–16.)
Figure 23.13 Bronchial foreign body. Four-month-old male infant with cough and difficulty breathing for two days. Frontal radiograph of the chest reveals a nail in the right main stem bronchus, which was confirmed and removed at bronchoscopy. (From Wadhera R, Gulati SP, Garg A, Ghai A. Bronchial foreign body: an unusual form of child abuse. Int J Pediatr Otorhinolaryngol. 2008;72:133–5.)
The hazards of accidental ingestion of small alkaline batteries are well known (94, 107, 114). These objects generally pass freely through the GI tract, but occasionally complications occur. Temple and McNeese described a 12-year-old child who ingested a mercury battery from a watch as part of an alleged poisoning attempt by an uncle (Fig. 23.14) (105). Thirty-six hours after ingestion, the battery ruptured, and impending perforation of the gastric mucosa was found at surgery. An intestinal battery may be encountered incidentally on skeletal survey (SS) in a child with fractures and other inflicted injuries (see Fig. 22.41). In the young infant, the finding points to forced attempted poisoning, but the circumstances surrounding the ingestion in the older child are more difficult to ascertain.
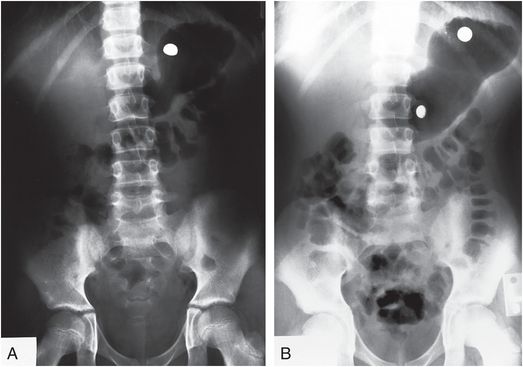
Figure 23.14 Battery poisoning. A, Supine view of the abdomen in a 12-year-old boy who ingested a mercury watch battery as part of an alleged poisoning attempt. An intact battery is noted in the gastric fundus. B, Follow-up film 36 hours later demonstrates disassociation of the battery components. (From Temple DM, McNeese MC. Hazards of battery ingestion. Pediatrics. 1983;71:100–3.)
Caustic substances may be administered as an overt homicidal act or as a component of Munchausen syndrome by proxy (see below). Lye, a well-known agent in accidental poisoning, may also be intentionally administered orally, or rarely rectally, by an abusive caretaker (98, 100). This results in severe acute and chronic inflammation of the esophagus. The feeding of a scalding liquid will lead to an esophageal burn similar to that resulting from a caustic chemical agent (Fig. 23.15) (115, 116).
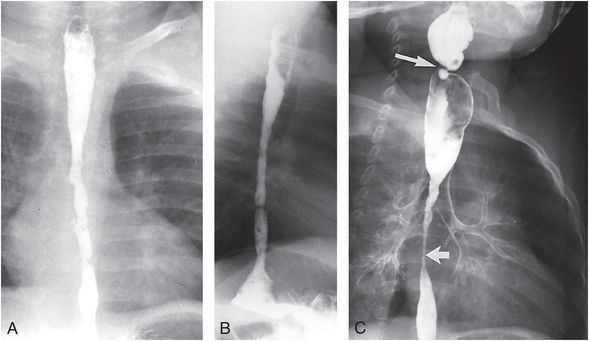
Figure 23.15 Poisoning by caustic ingestion. The mother of this six-month-old infant had fed the child scalding milk in an alleged poisoning attempt. Frontal (A) and lateral (B) views of a barium swallow demonstrate spasm and mucosal irregularity of the middle and distal esophagus. C, A follow-up study 10 months later shows high-grade strictures involving the cervical and midthoracic esophagus (arrows) with evidence of gross aspiration into the tracheal bronchial tree. The patient was subsequently treated with a colonic interposition. (Courtesy of Nancy Geneiser MD.)
A contrast esophagram in the acute phase demonstrates esophageal ulceration and spasm, and follow-up studies may show varying degrees of esophageal stricture. Other forced caustic ingestions may produce damage to the mouth, pharynx, and esophagus. Gotschlich and Beltran described a 21-month-old infant with stridor and respiratory distress (99). Radiography was not performed, but laryngoscopy demonstrated an erythematous swollen upper airway and epiglottis consistent with acute epiglottitis. Subsequently it was learned that the babysitter had forced the infant to ingest muriatic acid.
A rare case of pulmonary consolidation due to parental poisoning was described by Saulsbury and colleagues (104). The mother of an 11-month-old boy had introduced a naphtha variety hydrocarbon into the child’s intravenous line during the patient’s hospitalization. The child suffered an abrupt respiratory arrest, and during resuscitation a strong odor of hydrocarbon was noted. Radiographs demonstrated bilateral infiltrates that showed gradual resolution over subsequent days (Fig. 23.16).
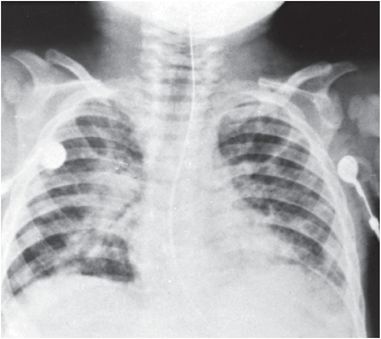
Figure 23.16 Poisoning by hydrocarbon. Pulmonary infiltrate secondary to poisoning of an infant whose mother injected naphtha into the child’s IV line during hospitalization. A radiograph on admission was interpreted as normal. This radiograph obtained 36 hours after admission demonstrates bilateral patchy pulmonary infiltrates consistent with hydrocarbon ingestion. (From Saulsbury FT, Chobanian MC, Wilson WG. Child abuse: parental hydrocarbon administration. Pediatrics. 1984;73:719–21.)
Impalement
Needles and other sharp objects may be inserted into a child’s body with overt abuse or as a ritual act (28, 110, 117–123). Swadia and colleagues described a child whose mother had inserted multiple needles into his chest and abdomen. The needles had been inserted over the preceding six weeks, but the child was only brought to attention when one of the needles had perforated the cecum, resulting in an acute abdomen (Fig. 23.17) (121). In a letter to the editor, Gadodia and Seithbhalla described a one-month-old with neck swelling and multiple sewing needles in the neck evident radiographically and on CT (Fig. 23.18) (110). One needle extended to the fourth cervical vertebra. Two additional needles were noted in the abdomen on the SS, but no fractures were identified.
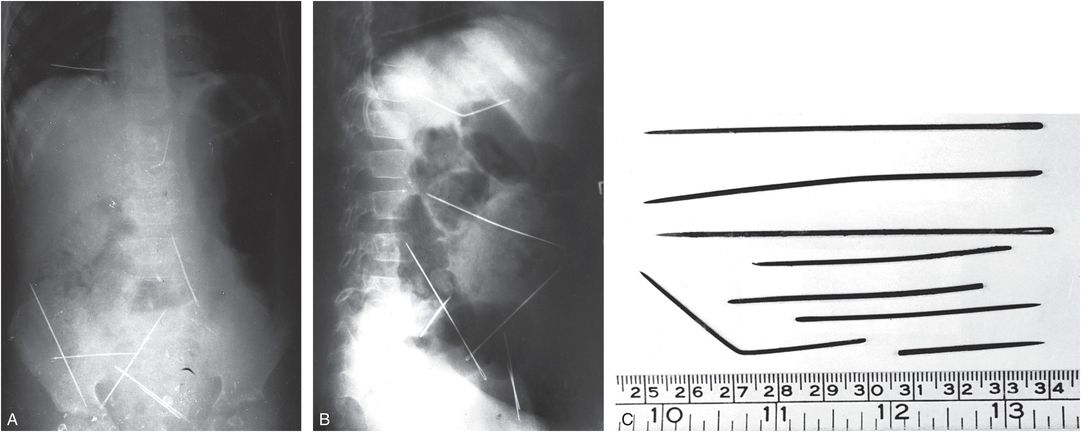
Figure 23.17 Impalement. A, B, Supine and lateral abdominal radiographs of an 11-year-old boy demonstrate multiple needles within the chest and abdomen. C, Seven needles, one broken, were removed at surgery. One needle had perforated the cecum and the second had pierced the left lobe of the liver. The mother admitted to inserting these needles during the preceding six weeks. (From Swadia ND, Thakore AB, Patel BR, Bhavani SS. Unusual form of abuse presenting as an acute abdomen. Br J Surg. 1981;68:668.)
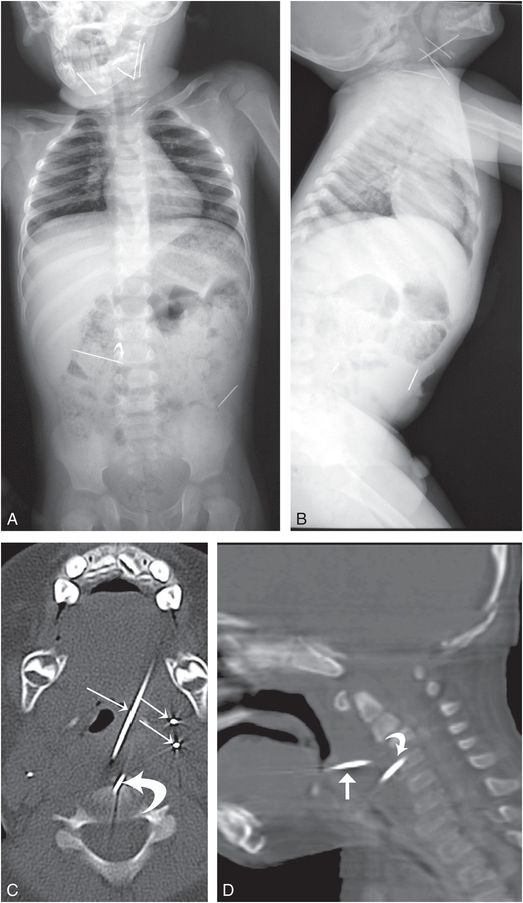
Figure 23.18 Sewing needle insertions. A, One-month-old male child was referred to the hospital with neck swelling for last three days. On examination, a hard foreign body was palpated, but the overlying skin was normal. There was no history of trauma; the parents indicated that the pregnancy was unwanted. AP (A) and lateral (B) radiographs show multiple metallic foreign bodies (sewing needles) in the neck and abdomen. C, D, Axial CT (C) of the neck and sagittal reformat (D) confirms multiple needles in the soft tissues (straight arrows). One of the needles extends into the C4 vertebral body (curved arrows). (From Gadodia A, Seithbhalla A. Letter Re: migratory foreign body of neck in a battered baby: a case report. Int J Pediatr Otorhinolaryngol. 2010;74:432–3.)
Sola and others described a three-month-old brought to the emergency room (ER) for “ear pain” (Fig. 23.19) (122). Subxiphoid erythema was noted and a needle was palpated and confirmed radiographically in the subcutaneous tissues. CT showed a needle extending into the heart, and at surgery a sewing needle entering the right ventricle was successfully removed. Care was complicated by the development of hydrocephalus, pseudo-meningocele, and a growing comminuted occipital skull fracture due to an earlier head injury from a reported fall. Lukefahr and others reported a 13-month-old with reluctance to walk and irritability. A SS done because of facial bruising showed multiple radiopaque needles in the scrotum and buttocks, and fragments of small nails or tacks in the heels (124).
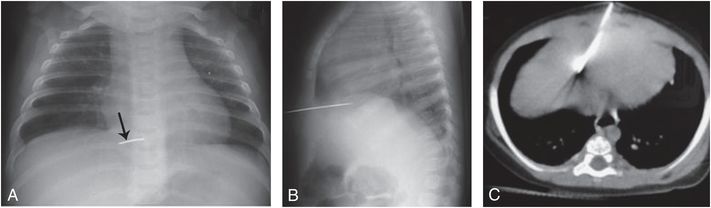
Figure 23.19 Penetrating cardiac injury. Three-month-old with “ear pain” and a foreign body palpated below the xiphoid. A, B, Frontal and lateral radiographs of the chest demonstrate a metallic foreign body penetrating lower thorax approximating the heart. C, CT shows a metallic foreign body extending to the heart. At surgery a sewing needle was found entering the right ventricle. (With permission from Sola JE, Cateriano JH, Thompson WR, Neville HL. Pediatric penetrating cardiac injury from abuse: a case report. Pediatr Surg Int. 2008;24:495–7.)
In a fascinating report from Iran, Amirjamshidi et al. described six patients, including two children aged six and seven years, with “attempted homicide” by intracranial sewing needle insertion (Fig. 23.20) (125). They reviewed the 26 previously reported cases, many of whom were also from Iran. Although most cases were adults, the needles were presumably inserted via the fontanels during childhood. The authors noted that this form of child abuse is well known in the Iranian community and they made reference to the practice described in a famous Iranian historical novel (126).

Figure 23.20 Sewing needle insertion. Six-year-old asymptomatic child with incidentally noted intracranial needles. Lateral radiograph of the skull shows four needles extending from the anterior fontanel. The child was subsequently under “close watch.” (From Amirjamshidi A, Ghasvini AR, Alimohammadi M, Abbassioun K. Attempting homicide by inserting sewing needle into the brain. Report of 6 cases and review of literature. Surg Neurol. 2009;72:635–41.)
Hadley and associates described six Zulu children, all but one of whom were girls, in whom sewing needles were allegedly inserted by the “tikoloshe” (127). The “tikoloshe” is believed to be a creature whose origins are deeply rooted in the local Zulu culture and causes mischief through an ill-defined relationship with the sangoma (witch doctor). The concept crosses all socioeconomic boundaries. These authors described one case in which a needle perforated the bladder and formed the nidus of a large calculus (Fig. 23.21). They noted other needles perforating the liver, abdominal wall, paravertebral region, neck, flank, umbilical hernia, ileum, and mesentery. An unexplained fracture of the humerus was seen in one of their patients.
Figure 23.21 Needle insertion. AP view of the pelvis in a two-year-old child demonstrates a large bladder calculus (black arrow) surrounding a needle that was inserted into the bladder. Other needles were present (white arrow). The parent blamed the injury on the “tikoloshe.” (From Hadley GP, Bosenberg AT, Wiersma R, Grant H. Needle implantation ascribed to “tikoloshe.” Lancet. 1993;342:1304.)
Munchausen syndrome by proxy
Munchausen syndrome by proxy (MSBP) is a condition in which a parent or caretaker fabricates or produces an illness in the child for which repeated medical attention is sought (128, 129). A vast array of signs, symptoms, and laboratory findings have been described in relation to the syndrome, and occasionally these have been associated with abnormalities seen on imaging studies (130–132). Because the diagnosis is usually obscure initially, the children may undergo extensive medical investigations that frequently entail imaging. UGI series, abdominal sonography, and abdominal and cranial CT and MRI are commonly used to identify an organic basis for a child’s signs and alleged symptoms. In a study of 10 cases of MSBP presenting to pediatric surgeons, Lacey and associates found that each child had undergone an average of 2 diagnostic imaging studies. All but one child had an UGI series examination (133). The elusiveness of the diagnosis of MSBP is well-illustrated in patients with symptoms and signs suggesting urologic and renal disease in a report by Feldman et al. (134). They noted 5 children aged 3–10½ years of age with a variety of signs, symptoms, and laboratory studies suggesting a urologic disorder, including artifactual hematuria, recalcitrant urinary infections, dysfunctional voiding, perineal irritation, glucosuria, and “nutcracker syndrome,” as well as alleged sexual abuse. Falsifications included incorrect or exaggerated history, specimen contamination, and induced illness. Several of the children underwent uroradiologic procedures.
It is evident that although radiology occasionally aids in the diagnosis of MSBP, the greatest impact of imaging in these cases may be the escalation of costs and risks related to unnecessary diagnostic procedures and their consequences. Furthermore, imaging studies may lead to the detection of inconsequential or false positive findings that lend credence to the caretaker’s assertions, perpetuating the cycle of injury and denial, and significantly delaying proper diagnosis and treatment.
Failure to diagnose MSBP may result in death. Estimates of mortality range as high as 33% (135). One of the most serious forms of this syndrome is factitious apnea, generally maternally induced. These children may undergo UGI series to assess for anatomic abnormalities and gastroesophageal reflux, or neuroimaging studies to exclude a central basis for the alleged apnea. These features may coexist with more overt forms of physical abuse associated with shaking and blunt impact when primary apnea is alleged to be the cause of the neurologic abnormalities (136–146). As stressed earlier, there is frequently overlap between miscellaneous forms of abuse and neglect, and MSBP is no exception. These children may also show other signs and symptoms of physical abuse (147).
Most victims of this syndrome are infants and toddlers. Diagnosis is often delayed by months to years. The perpetrator, usually the mother, frequently becomes adept and highly sophisticated at obscuring the facts. In-hospital video surveillance has been used to document the injurious episodes, particularly when factitious apnea is present (144, 148). Victims of MSBP may also be alleged by the offender to be victims of sexual or physical abuse. These children, who range from three to nine years of age, are generally older than those with the usual form of this syndrome, and these children are also at risk for undergoing inappropriate diagnostic imaging studies.
When poisonings, in particular toxic ingestions, are employed to produce illness, radiologic findings may be striking and similar to those seen with overt poisonings described earlier. Other poisonings include ipecac-induced cardiomyopathy and hemorrhagic colitis (149), gastric pneumatosis and portal venous gas (148), GI ulceration with recurrent sepsis (151), bacteremia, and septic arthritis (152–155).
Polymicrobial sepsis due to surreptitious introduction of bacteria into a child is a rare but well-documented type of MSBP (157, 158). Al-Owain et al. reported a 19-month-old girl with hepatosplenomegaly, anemia, thrombocytopenia, and recurrent septicemia. She was initially thought to have a myelodysplastic syndrome, and subsequently Gaucher disease was considered. The child improved after the mother was separated from the infant. The mother eventually indicated that she was spitting in local herbs and then injecting the material into the central vascular line (157).
Another striking case has been described with hepatic abscesses and multifocal osteomyelitis (Fig. 23.22) (158, 159). The three-year-old boy had a red and swollen right knee, and knee aspirates as well as blood cultures grew Fusobacterium necrophorum. Abdominal CT showed liver abscesses, which were drained. Parental injection of maternal saliva was determined to be the origin of the bacteremia in this case.
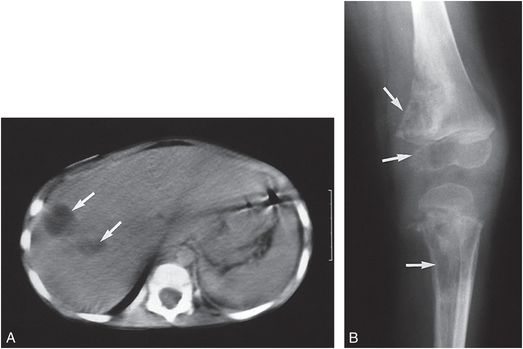
Figure 23.22 Munchausen syndrome by proxy. A, CT of the abdomen in a three-year-old child demonstrates several low-density areas in the right lobe of the liver, representing hepatic abscesses (arrows). B, An oblique radiograph of the knee shows destructive lesions (arrows) involving the metaphysis and epiphysis of the distal femur as well as the metaphysis of the proximal tibia, consistent with osteomyelitis. The mother admitted to injecting saliva intravenously into the child. The organism was Fusobacterium necrophorum. (From Van Dyke DC, Alexander RC, Perlman S, Smith Jr WJ, Dekowski SA. Fusiform bacterial sepsis: metastases with osteomyelitis and hepatic abscess occurring in a chaotic family. Clin Pediatr. 1989;28:423–5.)
Genitourinary foreign bodies are not uncommon findings in young children and may be noted with sexual abuse (see below), but radiologic studies are rarely of value. One exception is a case of MSBP reported in 1995 in which a 2-year-old boy was found to have stones inserted into his urethra by his mother (160).
Other miscellaneous manifestations of physical injury
Hair pulling
Although the skin and subcutaneous tissues are one of the most frequent sites of inflicted injury, other than nonspecific soft tissue swelling and bruising, cutaneous abnormalities are rarely noted on imaging studies. Scalp swelling may occur with hair pulling, and when there is massive subgaleal fluid without underlying cranial or intracranial injury, the possibility of hair pulling should be considered (Fig. 22.23) (161, 162). Care should be taken to differentiate abusive hair pulling from subgaleal hematoma due to vigorous hair combing and braiding, as well as scalp swelling due to underlying medical issues (163, 164).
Figure 23.23 Subgaleal hemorrhage secondary to hair pulling. CT scan of the head in a seven-year-old girl demonstrates diffuse subgaleal low attenuation (long arrows) with focal areas of higher attenuation (short arrow) consistent with blood in varying stages of evolution. There is underlying cerebral atrophy. (Courtesy of Sarah G. Klein MD.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree