Fig. 1.1
Clinical survey. (a) (1, 2) Skin deformation (b) Nipple retraction
Diagnostic accuracy of clinical examination in revealing benign breast changes in men and women does not exceed 65 %, and in the detection of breast cancer, 50–60 %. The sensitivity of clinical examination for breast carcinoma in women is 40–69 %, with a specificity of 88–95 % (Todua 1980; Korzhenkova 2004; Sencha et al. 2010a, b).
The experience of our clinic and literature analysis demonstrated that mistakes in the diagnosis of breast cancer arose in approximately 30 % of patients who saw the doctor for the first time for this purpose. Being aware of breast oncology often prevents incorrect medical decisions. It is necessary to remember this during routine examinations of men, especially for men older than 50–60 years.
Palpation of abnormal breast tissue is capable of revealing lesions (often of cartilaginous density) with rough contours that are located centrally behind the nipple or areola, or near to them. A detected lesion requires a more careful palpation of this area to determine the size, shape, consistency, motility of the mass, and status of the skin over the mass. The relatively thin layer of subcutaneous fat in men, as compared with women, and the affinity of the gland to the skin and underlying tissues mean that the tumor attaches early to the anterior thoracic wall and the skin, and the skin becomes wrinkled. However, palpation of a small breast tumor at early stages is often difficult, and the revelation of such tumors is often incidental.
The study of the status of steroid hormone receptors shows that receptors to estrogen and progesterone are often observed in men. The incidence of estrogen-positive malignant breast tumors in men is 65–100 %. Clinically significant levels can be registered in greater than 85 % of cases. Nevertheless, the expression of receptor-positive tumors in men does not increase with age, as compared with women. There is a correlation between clinically significant levels of estrogen receptors and the effects of hormone therapy.
1.2 Mammography
X-ray mammography is one of the most informative methods for the diagnosis of breast diseases, breast cancer in particular, in men and women (Khazov 1969; Todua 1980; Ostrovskaya and Yefimova 1985; Rozhkova 1993; Lindenbraten et al. 1997; Semiglazov 2002; Kharchenko and Rozhkova 2005; Komarova 2006).
Mammography is the technology of acquisition of negative images (digital or analog), which characterize the penetration of X-rays through tissue. A mammogram is a two-dimensional image of the breast. It permits the analysis of the density of the glandular tissue and the detection and assessment of the location, shape, margins, and dimensions of lesions. The spatial relationships of abnormal foci can be analyzed through obtaining images in several projections. Mammography can be performed as mammography screening, targeted mammography, axillography, pneumocystography, and ductography.
Mammography has the following advantages:
Detection of impalpable breast lesions
High diagnostic value
Possibility of invasive and noninvasive diagnostic procedures
Objective documented data accessible for dynamic analysis
The disadvantages of mammography are as follows:
Ionizing radiation
Low value in dense and irregular structures of the breast, including X-ray-negative carcinoma, infiltration, inflammation, and fibrous changes
The indications for mammography in men are as follows:
Age older than 60 years
Suspicion or clinical features of breast cancer in any age group
Other chronic breast diseases, especially nodular types (e.g., nodular type of chronic gynecomastia)
The criteria of mammographic diagnosis of breast carcinoma in men do not differ from the criteria in women (Khazov 1969; Todua 1980; Ostrovskaya and Yefimova 1985; Semiglazov 2002; Kharchenko and Rozhkova 2005). The characteristic features of breast cancer in men are lesions of increased density with radiant, spiky, indistinct margins, irregular structure with hyperdense linear patterns, and, often, microcalcifications. Dense spots are located eccentrically, which differentiates them from areas of gynecomastia (Fig. 1.2). Diagnostic mistakes are caused basically by difficulties in the definition of the mass against the increased density of the breast parenchyma. Mammography often permits the differentiation of gynecomastia and breast carcinoma on the basis of the characteristic location of gynecomastia (the retropapillary area and the relative symmetry of structures) and the status of the regional lymph nodes.
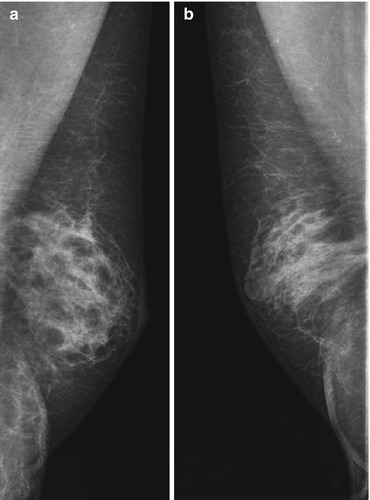
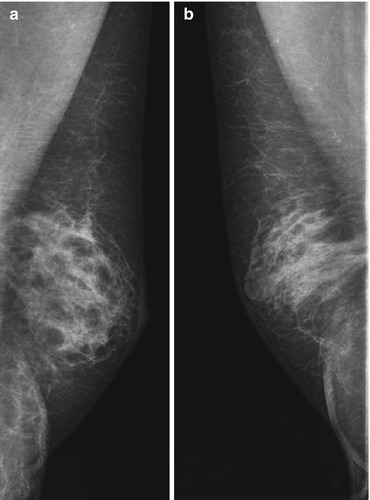
Fig. 1.2
Mammography. (a) Gynecomastia. (b) Breast cancer
The small thickness of the breast tissue layer in men often significantly complicates the performance of mammography, sometimes making it impossible, in comparison with women. Our experience shows that mammography in men is not always technically possible; however, it can be a beneficial addition to prophylactic medical examination with US. Some authors consider mammography a method of choice for the diagnosis of breast cancer in men and beneficial for the differential diagnosis of gynecomastia and breast carcinoma; others consider the efficacy of this method doubtful (Giordano 2005; Chen et al. 2006; Contractor et al. 2008; Khazov 1969; Todua 1980; Ostrovskaya and Yefimova 1985; Semiglazov 2002; Kharchenko and Rozhkova 2005; Dickson 2011).
The sensitivity of mammography for breast cancer in women is 50–93 %, with a specificity of up to 90 % and diagnostic accuracy up to 90 %. Impalpable carcinomas can be detected with mammography in 76–92 % of cases (Rozhkova et al. 1995; Chang et al. 1997; Korzhenkova 2004; Kharchenko and Rozhkova 2005; Letyagin 2006; Giordano 2005; Korde et al. 2010; Todua 1980). Ostrovskaya et al. (1988) consider that the optimal complex for the early diagnosis of breast carcinoma in men, as in women, is a classic triad of procedures: clinical observation, mammography, and cytology. This facilitates not only the correct diagnosis but also permits determination of the disease stage.
New technologies of mammography, a combination of analog, digital, and 3D-mammography with the introduction of digital tomosynthesis, open new prospects for radiology in the diagnosis of malignant breast pathology.
Ductography is seldom used in men. It is an X-ray modality that uses artificial contrasting of lactiferous ducts. It supplies information about the anatomy of lactiferous ducts: the type of branching, dilation, contours, and lumen condition. It permits assessment of intraductal lesions, their location, size, shape, and invasion.
1.3 Computed Tomography, Magnetic Resonance Imaging, and Positron Emission Tomography
Magnetic resonance imaging (MRI) is a valuable tool in the diagnosis of breast tumors in men and women (Pavic et al. 2004; Korzhenkova 2004; Mann et al. 2008; Serebryakova et al. 2011). Breast MRI enables T1- and T2-weighted imaging with complete acquisition sequences in all projections (axial, sagittal, and coronal). The technology of MRI analyzes data on the behavior of protons in hydrogen atoms. The motion of protons in one plane in a high-energy magnetic field is detected and analyzed to reconstruct an image. MRI enables the assessment of breast structure, including detection of abnormal foci and characterization of their capsules along with signs of invasion into surrounding tissues and visualization of lymph nodes. Dynamic MRI is a modality that is based on a series of variables, including different image characteristics (contrast, signal-to-noise ratio, resolution, time interval) and a series of other parameters. It allows the detection and interpretation of minimal changes in breast tissue (Fig. 1.3). Two important technical requirements of breast MRI are special magnetic coils and contrast agents.
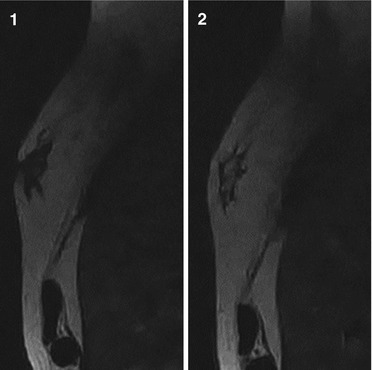
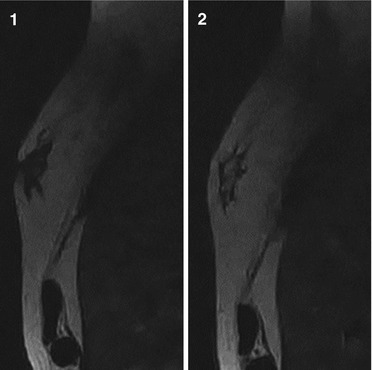
Fig. 1.3
(1, 2) MRI. T2-weighted fast relaxation, fast spin echo (T2FRFSE) sequence. Nodular gynecomastia
MRI is considered in individual cases. It is not a screening test. Nevertheless, it is applicable for the detection of pathological processes and dynamic observation in women in groups with a high risk of breast carcinoma, for example, with mutations of the BRCA 1 and 2 genes.
Contrast agents significantly increase the diagnostic value of breast MRI. The sensitivity of MRI with contrast enhancement in the diagnosis of breast tumors in men and women is 83–100 %, with a specificity of 29–97 % (Maryasheva 2003; Haylenko et al. 2005; Korzhenkova 2004).
MRI has the following advantages (Ternovoy et al. 1996; Kachanova 2000; Lukyanchenko and Gaurova 2001; Serebryakova et al. 2011):
High resolution and contrast of soft tissues of the breast
Possibility of acquisition of images in any plane without moving the patient
Noninvasiveness
Absence of ionizing radiation
Impressive possibilities of MRI in the detection of multifocal breast carcinoma were reported by Berg (2009). However, the high sensitivity of MRI in the diagnosis of breast pathology is accompanied by a low specificity and accuracy in revealing breast cancer. The high cost of the equipment forces the use of the technology only in difficult diagnostic cases (Haylenko et al. 2005).
Computed tomography (CT) is another modern radiological technology (Fig. 1.4). However, CT technology is not a screening modality for breast carcinoma because of significant radiation, high cost of examination, and low throughput. CT practically has no advantages in the early recognition of breast carcinoma as compared with mammography. However, the method is of great importance in the assessment of cancer invasion and is indicated to detect spreading of tumors into the retromammary space, metastases in lymph nodes, and remote metastases. The diagnostic value of CT in the detection of breast cancer is 60–62 %, the sensitivity is 100 %, and the specificity is 84 % (Dixon et al. 1993; Shevchenko 1997; Shishmareva 1997; Haylenko et al. 2005).
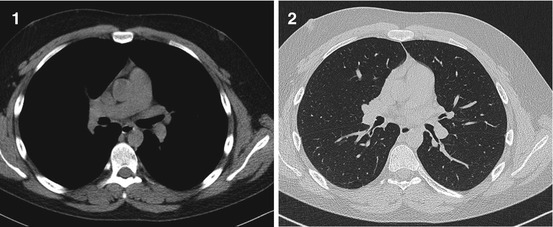
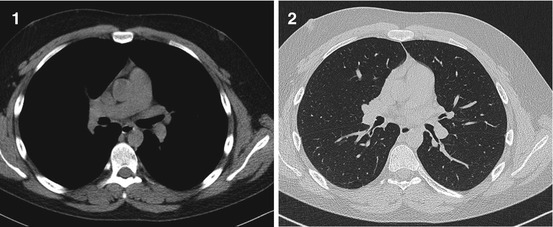
Fig. 1.4
(1, 2) CT. Breast carcinoma
Mammoscintigraphy is a method used for the functional diagnosis of breast pathology and is based on the assessment of the distribution of radiopharmaceuticals in breast tissues. 99mTc-MIBI, 99mTc-tehnetril, 99mTc-teoksim, 99mTc-tetrofosmin, and others can be used for the examination. Mammoscintigraphy, along with examinations of the breast, permits the assessment of isotope distribution in other chest structures, including axillary areas and other regions of possible metastases. The technology can be performed in two varieties: with a gamma chamber (planar scanning, emission gamma tomography) or positron emission tomography (PET). In those cases, it can be performed as an isolated breast scintigraphy, a polypositional scintigraphy of the chest, or as a single-photon emission CT scan of the breast area and thorax.
The sensitivity of mammoscintigraphy with 99mTc-tehnetril in primary breast tumors in men and women ranges from 62 to 96.7 %, with a specificity of 71–100 % (Svensson et al. 2000; Haylenko et al. 2005). Mammoscintigraphy with 99mTc-MIBI is not of great value in revealing primary breast carcinoma. Its sensitivity depends on the size of the lesion (Usov et al. 1997). The sensitivity of scintigraphy in the detection of metastases of breast carcinoma in axillary lymph nodes is 51–85 %, the specificity is 91–93 %, and the diagnostic accuracy is 76–93 % (Perre et al. 1997; Svensson et al. 2000).
Positron emission tomography (PET) is a nuclear medicine technology using various agents (monosaccharides, fatty acids, antibodies, peptides, etc.) marked with positron-emitting radionuclides. A modified gamma chamber is applied. It permits the detection of gamma photons, which result from the annihilation of positrons with electrons. Since gamma photons are emitted in opposite directions, it is possible to localize the place of their formation. Short-lived radioactive tracer isotopes, which are chemically incorporated into a biologically active molecule (frequently 18F-fluordeoxyglucose), allow the detection of areas with increased metabolic activity, which is often characteristic of malignant cells.
PET is not yet widely applied for the diagnosis of breast carcinoma. Nevertheless, it is quite a promising technology (Tyutin and Stanzhevsky 2003; Shiryaev et al. 2005). Indications for PET are limited because of its low diagnostic value in small cancers (smaller than 1 cm). However, PET surpasses all known anatomical imaging methods for the localization of centers of breast carcinoma in soft tissues. Its possibilities should be applied for individualization of therapy and monitoring, because tumor metabolism decreases much more rapidly than tumor size with effective treatment. Alternatively, an absence of changes in tumor metabolism after treatment may predict the inefficiency of the treatment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree