Chapter Outline
Motility disorders of the esophagus are an important cause of esophageal complaints, especially when symptoms are not readily explained by a structural abnormality. An understanding of esophageal anatomy and physiology is required for proper radiographic evaluation of normal and abnormal esophageal function. This chapter reviews the normal anatomy and physiology of the esophagus before discussing the radiographic evaluation of esophageal motility and the various esophageal motility disorders.
Normal Esophageal Anatomy
The esophagus is a muscular tube measuring 20 to 24 cm in length; it is composed of outer longitudinal and inner circular muscle fibers and is lined by stratified squamous epithelium. Striated muscle predominates in the upper third of the esophagus, with smooth muscle in the lower two thirds. The transition from striated to smooth muscle varies but usually occurs at the level of the aortic arch. Although this transitional zone is not evident on barium esophagography, certain motility disorders (e.g., collagen vascular diseases) may selectively involve the striated or smooth muscle portions of the esophagus.
Opening and closing of the upper and lower ends of the esophagus are regulated by the upper esophageal sphincter (UES) and lower esophageal sphincter (LES), respectively. The UES is located at the pharyngoesophageal junction and is formed primarily by the cricopharyngeal muscle, the horizontal portion of the inferior pharyngeal constrictor. The LES is not a distinct muscular entity but is defined manometrically as a high-pressure zone measuring 2 to 4 cm in length in the esophagogastric region. This physiologic sphincter corresponds in location to the anatomic esophageal vestibule.
Normal Esophageal Physiology
In the resting state, the esophageal body is normally collapsed, and the UES and LES are closed to prevent retrograde flow of esophageal and gastric contents. The major function of the esophagus is the transport of solids and liquids from the oral cavity to the stomach. The chief mechanism of bolus transport is esophageal peristalsis, which is assisted by gravity in the upright position. Radiographic evaluation of esophageal peristalsis is therefore usually performed with the patient recumbent to eliminate the effect of gravity.
Primary esophageal peristalsis is initiated by swallowing. A rapid wave of inhibition (not apparent radiographically) is followed by a slower wave of contraction, which traverses the entire esophagus ( Fig. 18-1 ). Relaxation of the UES occurs within 0.2 to 0.3 second of the initiation of swallowing, and relaxation of the LES occurs several seconds later. The LES remains relaxed as the oncoming bolus approaches the distal esophagus, returning to its contracted state shortly after the bolus reaches the stomach. The primary peristaltic contraction wave propagates through the esophagus in 6 to 8 seconds.

Secondary peristalsis and nonperistaltic contractions (NPCs) are other types of esophageal functional activity. Secondary peristalsis is initiated by local esophageal stimulation or distention, but is otherwise similar to primary peristalsis, propagating aborally. In contrast, NPCs (also known as tertiary contractions) are not propagated aborally. They typically involve the smooth muscle segment of the esophagus, occurring spontaneously or during swallowing. NPCs may be single or multiple, simultaneous or repetitive, and feeble or strong. Severe NPCs may narrow or obliterate the esophageal lumen, producing a characteristic corkscrew appearance on barium studies ( Fig. 18-2 ). NPCs are nonspecific and may be related to a variety of motility disorders involving the esophagus.

Individual variations in esophageal function are primarily related to aging. In young adults, most wet swallows initiate a complete peristaltic sequence, followed invariably by LES relaxation. NPCs are rare in this age group. However, older patients often exhibit incomplete peristaltic sequences during swallowing, with occasional LES dysfunction and a higher prevalence and severity of NPCs, a condition known as presbyesophagus. The amplitude of peristalsis, as recorded manometrically, also decreases with age. Thus, mild functional disturbances of the esophagus that are observed in older adults must be interpreted with caution and correlated with the clinical findings.
Radiographic Evaluation
Radiographic evaluation of esophageal motility includes an examination of the esophageal body and both sphincters. During swallowing, the UES relaxes and the pharyngoesophageal segment opens in response to bolus distention. Incomplete relaxation of the UES may be manifested on barium studies by a persistent indentation on the posterior aspect of the pharyngoesophageal junction resulting from the contracted cricopharyngeal muscle (see Chapter 15 ). This finding is often associated with other signs of pharyngeal dysmotility, such as aspiration or stasis of barium within the valleculae and piriform sinuses. Motion-recording techniques (using videotape or a digital recording device) facilitate evaluation of the pharynx and UES.
The fluoroscopic examination can be used to evaluate esophageal motility, but motion-recording techniques facilitate assessment of the findings. The patient is placed in the prone right anterior oblique (RAO) position and instructed to take single swallows of barium. At least five barium swallows are required for adequate evaluation of esophageal peristalsis and LES relaxation. Single swallows must be observed because a second swallow taken before completion of a primary contraction wave inhibits the propagating wave, so it can erroneously be mistaken for a peristaltic abnormality. In contrast, rapid, repetitive swallowing does not assess primary esophageal peristalsis but distends the esophagus maximally for structural evaluation ( Fig. 18-3 ).

As barium is propelled into the esophagus through the relaxed UES, a normal primary peristaltic sequence is seen as an aboral contraction wave that obliterates the esophageal lumen and progressively strips the barium bolus from the esophagus ( Fig. 18-4 ). This lumen-obliterating wave imparts an inverted V configuration to the top of the barium column, corresponding to the peristaltic pressure peak observed at manometry. In younger individuals, the peristaltic contraction wave normally strips all of the swallowed barium from the esophagus. Occasionally, so-called proximal escape of barium occurs at the level of the aortic arch ( Fig. 18-5 ). This age-related phenomenon is caused by a low-amplitude pressure trough at the transition zone between the striated and smooth muscle portions of the esophagus, which prevents closure of the esophageal lumen and allows retrograde flow of barium. In almost all cases, proximal escape can readily be differentiated from true esophageal motility disorders.


Esophageal Motility Disorders
Esophageal motility disorders may be classified as primary or secondary ( Table 18-1 ). Primary motility disorders mainly involve the esophagus, whereas secondary esophageal motility disorders result from a wide variety of systemic diseases or from physical or chemical injury of the esophagus. Esophageal motility disorders may also be classified manometrically into four groups: (1) inadequate LES relaxation (classic achalasia); (2) uncoordinated contraction (diffuse esophageal spasm); (3) hypercontraction (nutcracker esophagus and hypertensive LES); and (4) hypocontraction (nonspecific esophageal motility disorders, presbyesophagus, and secondary esophageal motility disorders). Because this classification of esophageal motility disorders is based on manometric findings that cannot be adequately quantified on barium studies, we have instead chosen to classify primary and secondary esophageal motility disorders conceptually in this chapter (see Table 18-1 ).
| PRIMARY MOTILITY DISORDERS (NEWER CLINICAL CATEGORIES) |
|
| SECONDARY MOTILITY DISORDERS (MANY WITH HYPOCONTRACTION) |
|
Primary Motility Disorders
Achalasia
Achalasia is a well-recognized esophageal motility disorder characterized by a combination of absent peristalsis in the esophagus and impaired LES opening in response to deglutition. Two forms of achalasia have been described, primary and secondary. Primary achalasia (also known as idiopathic achalasia) is caused by degeneration and loss of myenteric ganglia in the wall of the esophagus. The cause is unknown but is postulated to be secondary to viral or autoimmune disease. In contrast, secondary achalasia (also known as pseudoachalasia) is a less common form caused by extraesophageal conditions (usually malignant tumors) that induce an achalasia-like motility disorder by a variety of proposed mechanisms. Long-standing primary achalasia may also be a precursor of esophageal carcinoma. The association with carcinoma varies, but in one study the risk of carcinoma was 9 to 28 times greater than that in the general population. For the remainder of this chapter, the term achalasia is used to denote primary achalasia.
Achalasia occurs equally in both genders and usually affects patients during the middle decades of life. Most patients seek medical attention because of long-standing, slowly progressive dysphagia for solids and liquids, often associated with regurgitation of bland, undigested food and saliva. Painful swallowing and chest pain are less common. Weight loss may occur in severe cases. Patients with chronic regurgitation may develop recurrent episodes of coughing, choking, and aspiration pneumonia. If dysphagia has a recent onset and is rapidly progressive in older patients with radiographic or manometric findings of achalasia, secondary achalasia caused by malignancy should be strongly suspected (see Chapter 24 ).
Achalasia is characterized manometrically by the absence of primary peristalsis, elevated or normal resting LES pressures, and incomplete or absent LES relaxation in response to deglutition ( Fig. 18-6 ). However, the presence and degree of LES relaxation on manometry are unreliable because some patients with typical clinical and radiographic findings of achalasia are found to have complete manometric relaxation of the LES. Other patients may have variants of achalasia, with atypical manometric findings. A debated variant, vigorous achalasia, is characterized by high-amplitude, simultaneous, and repetitive contractions. These patients may present with chest pain and have less esophageal dilation. Another controversial variant, early achalasia, is characterized by aperistalsis, with normal LES relaxation. Patients with early achalasia also have less esophageal dilation and tend to be younger. Both these variants may represent transitional motility disorders evolving toward classic achalasia.

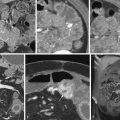
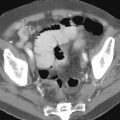
Achalasia is characterized on barium esophagography by the absence of primary peristalsis on all swallows. The distal esophagus typically has a smooth, tapered, beaklike appearance at the level of the esophageal hiatus ( Fig. 18-7 ) because of LES dysfunction and failure of the barium bolus to distend the tonically contracted sphincter. The degree of esophageal dilation is variable, and some patients with early achalasia have little or no esophageal dilation. Others with vigorous achalasia have repetitive NPCs associated with typical findings of achalasia. Over time, the esophagus becomes increasingly distended, and retained food, secretions, and barium in the dilated esophagus ( Fig. 18-8A ) may obscure underlying esophagitis or even developing esophageal carcinomas. In such cases, the fluoroscopist can use a water flush technique in which the patient swallows tap water at the end of the fluoroscopic examination to clear residual barium from the distal esophagus and facilitate the detection of tumor. Advanced achalasia may be recognized on chest radiographs when marked esophageal dilation produces a double contour of the right mediastinal border, and little or no gas enters the stomach ( Fig. 18-8B ). Eventually, some patients with long-standing disease develop a massively dilated esophagus that has a tortuous distal configuration, also known as the sigmoid esophagus of end-stage achalasia ( Fig. 18-9 ).



Achalasia must be differentiated from other causes of narrowing in the distal esophagus ( Table 18-2 ). In particular, an underlying carcinoma of the esophagogastric region must be excluded ( Fig. 18-10 ). Although most malignant tumors in this region are characterized radiographically by mucosal irregularity or mass effect (see Fig. 18-10B ), carcinoma of the cardia and other malignant tumors causing secondary achalasia may be manifested on barium studies by smooth, tapered narrowing of the distal esophagus and aperistalsis, mimicking the findings of primary achalasia (see Fig. 18-10A and Chapter 24 ). Peptic strictures are another common cause of distal esophageal narrowing, but such strictures are rarely associated with aperistalsis, and affected individuals almost always have accompanying hiatal hernias, an unusual finding in achalasia. Scleroderma is another cause of marked esophageal dilation, but these patients typically have a patulous, gaping esophagogastric junction, enabling differentiation from achalasia. Occasionally, peptic strictures complicating scleroderma may produce an appearance simulating that of achalasia, but the correct diagnosis is usually suggested by the presence of an associated hiatal hernia.