Traumatic spinal injuries are common and carry a high risk for severe morbidity and mortality. While computed tomography remains the primary screening imaging method for acute spinal trauma, MR imaging plays an important complementary role in emergency management and triage for cervical spine trauma. This review examines the benefits and limitations of MR imaging, focusing on its indications, structured assessment of spinal stability, and evolving role for evaluation of spinal cord injuries.
Key points
- •
MR imaging is advantageous for the evaluation of traumatic cervical spinal instability in select patients and essential for evaluating patients with suspected traumatic cervical spinal cord injury.
- •
Evaluation for spinal instability with MR imaging relies on knowledge of spinal anatomy and key MR imaging findings indicative of spinal tension band disruption.
- •
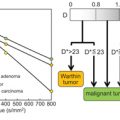
Both axial and sagittal MR imaging features of traumatic spinal cord contusion correlate with injury severity and neurologic outcome.
- •
The presence and length of intramedullary spinal cord hemorrhage as assessed with MR imaging is the most robust imaging-based predictor of spinal cord injury severity.
- •
Diffusion imaging techniques may complement conventional MR imaging sequences for characterizing spinal cord injury.
| AD | axial diffusivity |
| ADC | apparent diffusion coefficient |
| ALL | anterior longitudinal ligament |
| ASIA | American Spinal Injury Association |
| CSF | cerebrospinal fluid |
| DTI | diffusion tensor imaging |
| DWI | diffusion-weighted imaging |
| FA | fractional anisotropy |
| ISL | interspinous ligament |
| LF | ligamentum flavum |
| PLC | posterior ligamentous complex |
| PLL | posterior longitudinal ligament |
| SCI | spinal cord injury |
| ss-EPI | single-shot echo-planar imaging |
| SSL | supraspinous ligament |
| STIR | short tau inversion recovery |
| tSCI | traumatic spinal cord injury |
Introduction
Published more than 100 years ago, Dr Charles A. Elburg’s 1916 classic and revolutionary text, Diagnosis and Treatment of Surgical Diseases of the Spinal Cord and Its Membranes , highlighted the importance of imaging for diagnosing and treating traumatic injuries of the spine. In reference to early management of suspected acute spinal cord injury, Dr Elburg notes, “As soon as possible, X-ray pictures of the spine must be taken.” Even with the rudimentary imaging technology of the early twentieth century, the crucial role of imaging for diagnosis and management of traumatic cervical spine injury was established.
Development and improvements in imaging technology, especially MR imaging, have further elevated the role of imaging in cervical spine trauma patient care. As described in Dr Elburg’s seminal text, the combination of careful neurologic examination and imaging remains the cornerstone for modern care of patients with acute traumatic cervical spine injury. In this review, the appropriateness and complementary roles of computed tomography (CT) and MR imaging for imaging patients with suspected cervical spine trauma will be highlighted with focus on MR imaging protocols tailored for evaluating traumatic spinal pathology. In the context of the most up-to-date traumatic spine injury classification systems, a practical and algorithmic approach to image interpretation will be reviewed. Key diagnostic and neuroprognostic imaging features of traumatic spinal cord injury (tSCI) along with both conventional and advanced quantitative diffusion MR imaging techniques for evaluating traumatic spinal cord disruption will also be discussed.
Background and epidemiology
Approximately 4% of polytrauma patients experience acute cervical spine injuries, with vertebral fractures being the most reported. Ligamentous injuries are less frequently identified, potentially due to under-diagnosis and the necessity of MR imaging for accurate diagnosis. tSCI affects a subset of spinal trauma patients, with an estimated annual incidence of 54 cases per million in the United States, translating to roughly 18,000 new cases each year. Over recent decades, there has been a demographic shift, with more elderly individuals sustaining these injuries. , Although acute traumatic spinal cord injury (SCI) accounts for a small percentage of polytrauma cases, the associated emotional, physical, and psychological impacts are beyond measure.
Assessment of acute spinal trauma, including for potential tSCI, relies on a comprehensive clinical history and detailed physical examination. Various neurologic and functional assessment tools help classify injuries. The American Spinal Injury Association (ASIA) developed the International Standards for the Neurologic Classification of Spinal Cord Injury, which includes a neurologic evaluation and uses the ASIA Impairment Scale. This 5-point scale ranges from complete motor and sensory injury (Grade A) to a normal examination (Grade E). Along with motor and sensory scores, this score predicts 1-year functional recovery.
Despite the importance of clinical evaluation, early assessment can be challenging due to co-morbid conditions such as traumatic brain injury, severe pain, or the use of sedatives among other factors. These can complicate evaluation, making imaging examinations crucial for objective injury assessment in the presence of confounding conditions.
Imaging appropriateness for cervical spine trauma
The National Emergency X-Radiography Utilization Study and the Canadian Cervical Rules are well validated screening instruments for clinical decision making. , Both tools are sensitive for detecting clinically significant cervical spine injuries. While both reference plain radiography for initial imaging, many fractures readily visible on CT scans remain occult on standard radiographs. Consequently, CT has become the recommended method for the initial assessment of suspected spinal injuries due to its superior ability to visualize skeletal damage and is the reference standard for imaging in patients meeting screening criteria. ,
The indications for MR imaging in cervical spinal trauma evaluations are less clearly defined and can be more contentious than those for CT. The American College of Radiology has developed appropriateness criteria based on a review of existing literature and expert consensus, suggesting that MR imaging is typically appropriate in various scenarios, particularly for patients with confirmed or suspected spinal cord or nerve root injuries, regardless of CT results. Furthermore, MR imaging is recommended as a supplementary examination alongside CT for patients with potential mechanically unstable spine injuries who are candidates for surgery. MR imaging is considered the imaging gold standard for evaluating disco-ligamentous spinal injuries.
Routine use of MR imaging as the initial imaging technique for blunt spinal trauma, however, is not typically advised. The utility of MR imaging following a negative cervical spine CT—whether in alert or obtunded patients—is questionable. Several studies, including cost-effectiveness analyses, have indicated that MR imaging rarely reveals soft-tissue injuries necessitating surgery that are not already identified by CT, and thus should not be standard practice when CT results are negative. The decision to use MR imaging in setting of negative cervical spine CT heavily depends on clinical judgment. Patients with ongoing neck pain or limited range of motion, as well as those with mild CT findings like stable fractures or prevertebral edema, may or may not need further MR imaging evaluation. Future controlled studies are essential to enhance evidence-based decision-making in these contexts.
MR imaging protocols for blunt cervical spine trauma
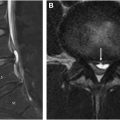
A typical MR imaging protocol for blunt cervical spinal trauma includes sagittal T1-weighted (T1-W), axial and sagittal T2-weighted (T2-W), sagittal fat-suppressed T2-W, and axial T2∗-weighted (T2∗-W) sequences. Increasingly, diffusion-weighted imaging (DWI) sequences, in either axial or sagittal orientation, are being incorporated to complement T2-W images for assessing the injured spinal cord. If there is concern for vascular injury, MR angiography and/or fat-suppressed T1-W/black-blood sequences may be added.
This standard MR imaging protocol for spinal trauma relies heavily on various T2 sequences, each offering distinct advantages and limitations in evaluating the spine. While T2-W signal abnormality in the spinal cord is not specific to the underlying injury pathophysiology, T2 imaging is highly sensitive for detecting acute spinal cord contusion. Both axial and sagittal T2 imaging of the spinal cord provide complementary views that help assess the injury severity and prognosis of acute spinal cord injuries. T2-W imaging is also valuable for identifying blood products in the spinal cord, which appear as hypointense areas due to phase dispersion and T2 shortening caused by intraparenchymal blood products shortly after trauma.
Fat suppression, when added to T2 sequences, may slightly reduce the signal-to-noise ratio and introduce artifacts, but enhances sensitivity to injury of important spinal structures, such as the paraspinal muscles, disc-ligamentous structures, and acute bone injuries. Typically, sagittal T2-W images with fat suppression are obtained using techniques like DIXON or short tau inversion recovery (STIR), allowing a thorough evaluation for spinal cord, spinal column, and paraspinous injury. Axial T2-W images may then be acquired without fat suppression for optimal spinal cord evaluation without the limitations of fat suppression.
Increasingly, cervical MR imaging protocols incorporate high-resolution sagittal 3-dimensional (3D) T2-W sequences, which supplement T1-W images to offer detailed anatomic delineation of spinal structures, particularly for assessing the integrity of disc-ligamentous structures and cerebrospinal fluid (CSF) spaces. T2∗-W and susceptibility-weighted imaging sequences are particularly sensitive to intramedullary blood products. It is important to realize that T2∗-W sequences enhance intrinsic contrast between spinal cord gray and white matter with mildly hyperintense gray matter as a normal feature, which may obscure mild central cord injuries or result in the misinterpretation of normal gray matter as abnormal edema.
Several recent studies have demonstrated the benefit of early spinal decompression for treatment of acute tSCI. , Thus, “time is spine” is an emerging mantra in management of acute tSCI. As a result, there is increasing interest in developing rapid MR imaging protocols tailored to address only the most emergent surgical questions such as identifying the level of spinal cord compression. A code activation protocol was recently implemented for acute tSCI patients at Zuckerberg San Francisco General Hospital, which involves rapid notification and engagement of multiple clinical services including spine surgery, anesthesia, neurocritical care, respiratory therapy, and radiology. The rapid MR imaging spine protocol utilized as part of this activation requires less than 15 minutes of scan time and involves sagittal T2 DIXON fat suppressed survey of the entire spine with axial T2-W spin echo imaging targeted to levels of acute injury or cord compression. Rapid imaging may enable more efficient patient triage leading to earlier surgical decompression and stabilization. Impact on patient outcomes remains to be determined. While rapid, these protocols do lack sequences that can be useful for detailed assessment of ligamentous structures, such as 3D T2 sequences. Further, incidental findings, such as nontraumatic T2-hyperintense bone marrow abnormalities, may be difficult to fully characterize. One approach to mitigate this limitation is to utilize the “fat-only” images from the Dixon acquisition to provide a “T1-like” fat-sensitive sequence for identifying fat-containing tissues, both normal and pathologic.
A structured approach to interpreting cervical MR imaging for spine trauma
Spinal Instability
It is important to recognize both strengths and weaknesses of MR imaging with respect to diagnosing blunt discoligamentous injury. Studies correlating MR imaging findings of soft tissue injury with intraoperative assessment have demonstrated high sensitivity for MR imaging, thus validating its role for traumatic soft tissue injury screening. , However, specificity for intervertebral disk, interspinous ligament (ISL), and ligamentum flavum (LF) disruption was found to be moderate to low. MR imaging-based overdiagnosis of posterior ligamentous complex (PLC) disruption has also been described. These few studies suggest that MR imaging tends to overestimate the extent of disruptive injury of spinal soft tissue structures when compared to intraoperative findings and caution is advised when using MR imaging for operative decision making. , With advances in MR imaging technology and improved techniques, such as 3D T2 sequences as detailed earlier, diagnostic limitations may be overstated. Nevertheless, the potential for overdiagnosis with MR imaging should be carefully considered by the radiologist and spinal surgeon along with the patient’s clinical condition, especially when MR imaging findings are ambiguous for clear ligamentous disruption.
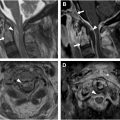
Panjabi and White defined spinal stability as the spine’s ability to maintain proper vertebral alignment under physiologic loads, without causing damage or irritation to the spinal cord or nerve roots, and without leading to deformity or pain. Translating this biomechanical concept into imaging criteria for instability for the subaxial cervical spine has led to the development of numerous traumatic injury classification systems. One of the best known is the Denis classification, which divides the spine into 3 columns: the anterior column (comprising the anterior two-thirds of the vertebral body and discs), the middle column (posterior third of the vertebral body and discs), and the posterior column (spinal posterior elements). The Denis classification system has limitations. Namely, it does not incorporate ligamentous injuries and it has been shown to inaccurately classify for stability based on bony column involvement alone.
The Arbeitsgemeinschaft für Osteosynthesefragen classification builds on the Denis model by categorizing injuries according to mechanical forces: Type A (compressive injuries), Type B (distraction injuries), and Type C (injuries from axial torque). Each of these injury types is further subdivided into divisions and sub-divisions, creating a highly detailed but arguably overcomplex and cumbersome system to apply in routine clinical practice.
To address complexities and limitations of existing systems, the Spine Trauma Study Group introduced the Subaxial Cervical Injury Classification system. This system categorizes injuries based on 3 criteria: injury morphology, the integrity of the PLC, and neuroaxis involvement. Each category is assigned numeric values to help guide surgical management based on the total score. Complexity, low inter-rater reliability, and the heavy reliance on MR imaging for assessing PLC integrity have been identified as limitations to this system.
In response to these challenges, the AOSpine Trauma Knowledge Forum developed more streamlined AOSpine Thoracolumbar and Subaxial Cervical Spine Classifications in 2013 and 2016, which have gained adoption in clinical practice. These systems use imaging-based criteria to classify injuries into 3 major morphologic categories: Type A (compression), Type B (tension-band), and Type C (translational) injuries, with further subtypes within each of these categories. Key additions to classification include the incorporation of patient neurologic status and specific modifiers based on individual conditions, such as spinal ankylosis. Separate classification for cervical facet joint injuries is also defined. The AOSpine cervical subaxial cervical and thoracolumbar injury systems categorize stabilizing structures of the spine into anterior and posterior tension bands, with the anterior band including the vertebral bodies, discs, and connecting ligaments of the vertebral bodies, including the anterior longitudinal ligament (ALL) and posterior longitudinal ligament (PLL). The posterior tension band includes the posterior vertebral bony elements and posterior ligamentous complex comprised by the LF, ISL, supraspinous ligament (SSL), and facet joint capsules. The AOSpine cervical injury system has been criticized for leaving “gray areas” in decision-making, particularly due to ongoing reliance on MR imaging, which is not always readily available. Nevertheless, it offers a structured and clinically relevant framework for evaluating spinal stability and informing MR imaging interpretation, as will be further explored further in the next section ( Table 1 ).
| Type A | Type B | Type C |
|---|---|---|
| A0: Minor/nonstructural fractures involving spinal processes, lamina, etc. | B1: Bony posterior tension band disruption (“Chance” type fracture) | C: Translational injury with displacement/translation of one vertebral body relative to another and associated anterior and posterior tension band disruption |
| A1: Wedge-compression fracture involving a single vertebral endplate | B2: Capsuloligamentous disruption of the posterior tension band | |
| A2: Vertically oriented “Split” fracture involving both endplates with sparing of the anterior and dorsal walls. | B3: Anterior tension band disruption related to hyperextension injury | |
| A3: Incomplete burst fracture involving a single vertebral body endplate and the posterior vertebral body wall. | ||
| A4: Complete burst fracture involving both endplates and the posterior vertebral body wall |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree