MR imaging is one of the most commonly used imaging techniques to evaluate patients with hip pain. Intra-articular abnormalities of the hip joint are better assessed with recent advances in MR imaging technology, such as high-field strength scanners, improved coils, and more signal-to-noise ratio-efficient sequences. This article discusses the causes of early hip joint degeneration and the current use of morphologic and physiologic MR imaging techniques for evaluating the articular cartilage of the hip joint. The article also discusses the role of MR arthrography in clinical cartilage imaging.
Hip pain is a common complaint seen in clinical practice and can be caused by intra-articular and extra-articular causes. The intra-articular causes of hip pain include acetabular labral tears, loose bodies, synovitis, ligamentum teres injuries, osteoarthritis, and osteochondral lesions. More recently, many of these intra-articular abnormalities have been shown to be related to underlying femoroacetabular impingement. Magnetic resonance imaging (MR imaging) is one of the most commonly used imaging methods to evaluate patients with hip pain. Intra-articular abnormalities of the hip joint are better assessed with recent advances in MR imaging technology, such as high-field strength scanners, improved coils, and more signal-to-noise ratio (SNR)-efficient sequences. The volume of hip arthroscopy has exploded over the past decade allowing correlation between hip findings seen at arthroscopy and MR imaging.
The hip joint is one of the most common sites of debilitating osteoarthritis. Osteoarthritis of the hip joint is not limited to the elderly population but may also occur in middle-aged adults and even in young individuals. Surgical treatment of osteoarthritis includes cartilage debridement and correction of deformities of the femoral head or acetabulum in patients with early joint degeneration and total hip replacement in patients with advanced disease. Early detection of cartilage damage is paramount for proper patient selection to help identify individuals who may benefit from early medical and surgical intervention. This article discusses the causes of early hip joint degeneration and the current use of morphologic and physiologic MR imaging techniques for evaluating the articular cartilage of the hip joint. The article also discusses the role of MR arthrography in clinical cartilage imaging.
Factors influencing the detection of cartilage lesions on MR imaging
Accurate measurements of articular cartilage thickness have become increasingly important in clinical practice. Osteoarthritis and hip joint injuries can result in changes in cartilage morphology. There is increasing interest in measuring and monitoring changes of articular cartilage thickness in the management of patients with prior injury or findings of femoroacetabular impingement.
MR imaging evaluation of articular cartilage within the acetabulum and femoral head can be difficult. The hip joint is located off isocenter in the MR imaging scanner, which can decrease image quality. The femoral head and acetabulum are closely apposed in the normal hip, making the separate articular surfaces difficult to discriminate from each other. Additionally, the articular cartilage is thin, which also poses difficulty in the detection of cartilage lesions. Leg traction technique during MR imaging and MR arthrography has been used to allow separation of the acetabular and femoral articular surfaces. However, in many cases, the joint space between the femoral and acetabular articular cartilage is narrow despite traction.
Recently, hip cartilage thickness and volumes measurement have been described in cadaver hip joint, within the living human hip joint, and before and after periacetabular osteotomy using MR imaging, MR arthrography, and computed tomography (CT) arthrography. In the study performed by Wyler and colleagues, MR arthrography and CT arthrography had similar accuracy for measuring hip cartilage thickness in the coronal plane. Cartilage thickness could also be measured in the sagittal and axial planes using CT arthrography but not MR arthrography. These imaging techniques have been shown to be reproducible and sensitive to submillimeter changes in cartilage thickness and may be useful in monitoring morphologic changes caused by disease progression in patients with osteoarthritis of the hip joint.
Causes of early hip osteoarthritis
The etiology of osteoarthritis of the hip joint may be primary (some underlying abnormality of articular cartilage) or secondary (congenital or developmental abnormality). Recently, primary osteoarthritis of the hip joint is thought to also be secondary to subtle developmental abnormalities that have been described as femoroacetabular impingement. Femoroacetabular impingement is a cause of premature osteoarthritis in the hip joint. The most frequent location for femoroacetabular impingement is the anterosuperior rim region.
Two types of femoroacetabular impingement have been described. Cam-type femoroacetabular impingement is more prevalent in young men. It is caused by a nonspherical shape of the femoral head at the femoral head-neck junction and decreased depth of the femoral waist leading to contact of the femoral head-neck junction against the acetabular rim. Pincer-type femoroacetabular impingement is more prevalent in middle-aged women and is secondary to acetabular overcoverage, which limits the range of motion of the hip and leads to a contact between the acetabulum and femur. Most individuals have a combination of these two mechanisms and are classified as mixed cam-pincer impingement.
The pattern of damage to the articular cartilage depends upon the shape of the hip joint. With cam femoroacetabular impingement, the articular cartilage is commonly damaged within the anterosuperior aspect of the acetabulum. With pincer impingement, damage to the articular cartilage occurs more circumferentially, typically with only a narrow strip of involved cartilage within the posteroinferior acetabulum. Following cartilage injury in cam impingement, tears or detachment of the anterosuperior labrum can occur. Pincer impingement initially results in a labral tear or degeneration, which is the first structure to fail, followed by cartilage injury. The femoral head articular cartilage remains uninvolved over a long period in pincer impingement and only late in the process will the cartilage damage occur within the posterior inferior femoral head or acetabulum called the “contrecoup lesion.”
It is important to recognize the type of femoroacetabular impingement because the surgical treatment differs for each type. In cam femoroacetabular impingement, the surgical technique performed is geared toward reshaping the femoral waist and restoring the spherical shape of the femoral head; whereas, in pincer impingement, the surgical technique is aimed at reducing the acetabular overcoverage by trimming the acetabular rim. Surgical interventions for femoroacetabular impingement include labral repair or debridement along with femoral and acetabular osteochondroplasty, and acetabular osteotomy. Performing these procedures before the development of advanced joint degeneration is essential for their long-term success. The goals for surgical intervention are to relieve pain, enhance activity and function, and preserve the natural hip joint over time. Recent review of the literature of hip impingement surgery has shown early relief of pain and improved function following treatment. The most important role of MR imaging in evaluating patients with femoroacetabular impingement is to assess the exact extent of joint degradation.. Thus, early detection of cartilage degeneration with MR imaging can help identify patients with hip pain who may benefit from early surgical intervention.
Femoroacetabular impingement is well recognized after total hip arthroplasty. It is known to also occur in individuals with abnormal hip anatomy, such as Legg-Calve-Perthes disease, slipped capital femoral epiphysis, developmental dysplasia, or posttraumatic deformity where there is a mismatch between the femoral head-neck junction and the acetabulum. Other causes of early osteoarthritis of the hip include inflammatory diseases (such as rheumatoid arthritis, ankylosing spondylitis, reactive arthritis, or lupus), as well as crystalline arthropathies, diffuse skeletal hyperostosis, and hemochromatosis. Damage to cartilage from infection, pigmented villonodular synovitis, synovial chondromatosis, and osteonecrosis can also lead to early osteoarthritis. Other congenital causes of early osteoarthritis of the hip joint include multiple epiphyseal dysplasia and spondyloepiphyseal dysplasia.
Causes of early hip osteoarthritis
The etiology of osteoarthritis of the hip joint may be primary (some underlying abnormality of articular cartilage) or secondary (congenital or developmental abnormality). Recently, primary osteoarthritis of the hip joint is thought to also be secondary to subtle developmental abnormalities that have been described as femoroacetabular impingement. Femoroacetabular impingement is a cause of premature osteoarthritis in the hip joint. The most frequent location for femoroacetabular impingement is the anterosuperior rim region.
Two types of femoroacetabular impingement have been described. Cam-type femoroacetabular impingement is more prevalent in young men. It is caused by a nonspherical shape of the femoral head at the femoral head-neck junction and decreased depth of the femoral waist leading to contact of the femoral head-neck junction against the acetabular rim. Pincer-type femoroacetabular impingement is more prevalent in middle-aged women and is secondary to acetabular overcoverage, which limits the range of motion of the hip and leads to a contact between the acetabulum and femur. Most individuals have a combination of these two mechanisms and are classified as mixed cam-pincer impingement.
The pattern of damage to the articular cartilage depends upon the shape of the hip joint. With cam femoroacetabular impingement, the articular cartilage is commonly damaged within the anterosuperior aspect of the acetabulum. With pincer impingement, damage to the articular cartilage occurs more circumferentially, typically with only a narrow strip of involved cartilage within the posteroinferior acetabulum. Following cartilage injury in cam impingement, tears or detachment of the anterosuperior labrum can occur. Pincer impingement initially results in a labral tear or degeneration, which is the first structure to fail, followed by cartilage injury. The femoral head articular cartilage remains uninvolved over a long period in pincer impingement and only late in the process will the cartilage damage occur within the posterior inferior femoral head or acetabulum called the “contrecoup lesion.”
It is important to recognize the type of femoroacetabular impingement because the surgical treatment differs for each type. In cam femoroacetabular impingement, the surgical technique performed is geared toward reshaping the femoral waist and restoring the spherical shape of the femoral head; whereas, in pincer impingement, the surgical technique is aimed at reducing the acetabular overcoverage by trimming the acetabular rim. Surgical interventions for femoroacetabular impingement include labral repair or debridement along with femoral and acetabular osteochondroplasty, and acetabular osteotomy. Performing these procedures before the development of advanced joint degeneration is essential for their long-term success. The goals for surgical intervention are to relieve pain, enhance activity and function, and preserve the natural hip joint over time. Recent review of the literature of hip impingement surgery has shown early relief of pain and improved function following treatment. The most important role of MR imaging in evaluating patients with femoroacetabular impingement is to assess the exact extent of joint degradation.. Thus, early detection of cartilage degeneration with MR imaging can help identify patients with hip pain who may benefit from early surgical intervention.
Femoroacetabular impingement is well recognized after total hip arthroplasty. It is known to also occur in individuals with abnormal hip anatomy, such as Legg-Calve-Perthes disease, slipped capital femoral epiphysis, developmental dysplasia, or posttraumatic deformity where there is a mismatch between the femoral head-neck junction and the acetabulum. Other causes of early osteoarthritis of the hip include inflammatory diseases (such as rheumatoid arthritis, ankylosing spondylitis, reactive arthritis, or lupus), as well as crystalline arthropathies, diffuse skeletal hyperostosis, and hemochromatosis. Damage to cartilage from infection, pigmented villonodular synovitis, synovial chondromatosis, and osteonecrosis can also lead to early osteoarthritis. Other congenital causes of early osteoarthritis of the hip joint include multiple epiphyseal dysplasia and spondyloepiphyseal dysplasia.
Imaging technique and diagnostic performance of cartilage imaging sequences
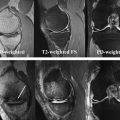
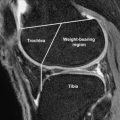
Both conventional MR imaging ( Fig. 1 ) and MR arthrography ( Fig. 2 ) are commonly used to diagnose internal derangements of the hip joint. MR imaging of the hip joint is best performed on 1.5-T or 3.0-T scanners because higher-field strength provides improved SNR, which is critical for high-resolution imaging. The need for a large field of view and the absence of specialized coils for evaluating the hip joint results in images with low spatial resolution. Contrary to many investigations reporting excellent results when imaging the articular cartilage of the knee joint, evaluation of the articular cartilage of the hip joint is more difficult. Hip imaging should be performed with either a surface-phased array coil or a multichannel cardiac coil. Intermediate echo time fast spin-echo sequences with an effective echo time of approximately 34 milliseconds at 1.5 T and 28 milliseconds at 3.0 T are recommended. The inherent magnetization transfer contrast of fast spin-echo techniques will yield differential contrast between the low signal intensity fibrocartilaginous labrum, intermediate signal intensity articular cartilage, and high signal intensity synovial fluid. Coronal images best demonstrate the femoral head articular cartilage within the suprafoveal region. Sagittal images best assess the articular cartilage within the anterosuperior and posterosuperior acetabulum and femoral head; whereas, axial oblique images best depict the articular cartilage of the anterior and posterior walls of the acetabulum (see Fig. 2 ).
Conventional MR imaging and MR arthrography
Two-dimensional fast spin-echo and 3-dimensional spoiled gradient-echo (SPGR) sequences have been used to evaluate the articular cartilage of the hip joint in clinical practice. Mintz and colleagues consider conventional MR imaging as having similar accuracy to MR arthrography in the detection of cartilage lesions of the hip joint. In their study using multi-planar, 2-dimensional fast spin-echo sequences with 0.6-mm x 1.2-mm in-plane resolution and 5.0-mm slice thickness, they reported sensitivity between 86% and 93% and specificity between 72% and 85% for detecting surgically confirmed cartilage lesions in 92 subjects. Nishii and colleagues evaluated 3-dimensional fat-suppressed SPGR images of the hip joint with 0.6-mm x 0.6-mm in-plane spatial resolution and 1.5-mm slice thickness and reported sensitivity between 49% and 67% and specificity between 76% and 89% for detecting surgically confirmed cartilage lesions. Possible explanations for the difference in diagnostic performance of MR imaging for evaluating the hip joint in these two studies include differences in image quality, subject population, or perhaps reader experience. The use of sequences with higher in-plane resolution and decreased slice thickness may potentially improve the detection of cartilage lesions within the hip joint, although further study is needed.
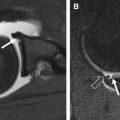
MR arthrography is considered superior to conventional MR imaging performed without intra-articular contrast material for evaluating the hip joint ( Figs. 3–5 ). The main sequences that are used in MR arthrography are fat-suppressed T1-weighted fast spin-echo sequences in the coronal, sagittal, and axial oblique planes (see Fig. 2 ). A fluid sensitive sequence and a nonfat-suppressed T1-weighted fast spin-echo sequence should also be included as part of the MR arthrogram protocol. MR arthrography has higher diagnostic performance than conventional MR imaging in the detection of labral tears. However, MR arthrography has low diagnostic performance for evaluating the articular cartilage of the hip joint. In the study by Hodler and colleagues, they correlated the anatomic and MR arthrogram measurements of femoral and acetabular cartilage thickness using a T1-weighted fast spin-echo sequence with frequency-selective fat suppression. The investigators found a significant correlation between the anatomic and MR arthrogram measurements of cartilage thickness. However, they concluded that the imaging technique was not sufficiently accurate with regard to the diagnosis for a specific patient because of the relevant scattering of data. The study by Nakanishi and colleagues found that the joint space remained narrow during MR arthrography with traction in subjects with severe osteoarthritis but not in subjects with osteonecrosis, hip dysplasia, or normal hips. Schmid and colleagues evaluated the diagnostic performance of MR arthrography for detecting cartilage lesions in subjects with suspected femoroacetabular impingement or labral abnormalities. Sensitivity and specificity for detecting surgically confirmed cartilage lesions within the anterosuperior acetabulum was 65% to 100% and 40% to 80%, posterior superior acetabulum was 30% to 70% and 63% to 89%, anterior inferior acetabulum was 58% to 83% and 63% to 80%, and posteroinferior acetabulum was 20% to 60% and 91% to 94%. The sensitivity and specificity for detecting cartilage lesions of the femoral head was 40% to 60% and 88% to 91%. The study by Byrd and colleagues compared conventional MR imaging and MR arthrography for evaluating the articular cartilage of the hip joint. The sensitivity and specificity for detecting surgically confirmed cartilage lesions was 41% and 100% for MR arthrography and 18% and 100% for conventional MR imaging. Furthermore, the sensitivity for detecting acetabular cartilage delamination in subjects with femoroacetabular impingement was as low as 22% for both imaging techniques.