Inflammation of the hip may be due to infectious and noninfectious causes. Furthermore, involvement is categorized based on the origin and spread to adjacent structures involving the soft tissues, the joint, and underlying bone to refine the differential diagnosis. Magnetic resonance (MR) imaging is highly effective in establishing the presence and underlying cause of inflammatory and degenerative arthropathies. This article discusses the use of MR imaging for evaluation of various inflammatory conditions of the hip, both infectious and noninfectious. The number of hip prostheses is increasing, and inflammatory conditions involving the postoperative hip is also detailed separately.
Key Points
- •
Infection and other inflammatory processes involving the hip can look similar on imaging exams.
- •
Knowledge of MR imaging characteristics of the different conditions can help differentiate them.
- •
Hip prostheses are prone to various complications; MRI can be a useful adjunct to other modalities.
Introduction
Inflammation of the hip may be due to infectious and noninfectious causes. The various conditions are difficult to differentiate clinically and by most imaging examinations. A high suspicion for infection is necessary when an unexplained monarticular joint effusion is noted. Hip joint infections can potentiate a medical emergency because of the risk of joint damage as well as local and distant spread. Infections of the hip can occur in any demographic; however, high-risk populations include patients with comorbidities (ie, chronic arthritis, immunosuppression, sickle-cell disease, and diabetes) and postoperative patients. Patient outcomes are positively influenced by early, accurate diagnosis. Magnetic resonance (MR) imaging is highly effective in establishing the presence and underlying cause of inflammatory and degenerative arthropathies. This article discusses the use of MR imaging for the evaluation of various inflammatory conditions of the hip, both infectious and noninfectious.
Introduction
Inflammation of the hip may be due to infectious and noninfectious causes. The various conditions are difficult to differentiate clinically and by most imaging examinations. A high suspicion for infection is necessary when an unexplained monarticular joint effusion is noted. Hip joint infections can potentiate a medical emergency because of the risk of joint damage as well as local and distant spread. Infections of the hip can occur in any demographic; however, high-risk populations include patients with comorbidities (ie, chronic arthritis, immunosuppression, sickle-cell disease, and diabetes) and postoperative patients. Patient outcomes are positively influenced by early, accurate diagnosis. Magnetic resonance (MR) imaging is highly effective in establishing the presence and underlying cause of inflammatory and degenerative arthropathies. This article discusses the use of MR imaging for the evaluation of various inflammatory conditions of the hip, both infectious and noninfectious.
Infection
Modes of Inoculation
Hematogenous
Synovial tissue is highly vascularized and is particularly vulnerable to hematogenous seeding of microbes. Enriched synovial transudative joint fluid and hyaluronic acid from the synovial surface cells establish an ideal medium for pathogens. Blood-borne pathogens advance swiftly through synovial membranes, activating the inflammatory process. Elastases and collagenases released by pathogens and the body’s own polymorphonuclear neutrophils break down the protective properties of the articular cartilage matrix.
Contiguous extension
Paralyzed patients are prone to contiguous extension of infection arising from decubitus ulceration. Periarticular bursae, underlying bones, and the hip and sacroiliac joints are vulnerable to infection caused by communication with ulcers that commonly form over the adjacent ischeal tuberosity, sacrum, or greater trochanter. Infection arising in this manner often spread along fascial planes into the adjacent sciatic notch, through the gluteus musculature and along the bones of the pelvis and femur, resulting in extensive infection with abscess formation and necrosis. Infection may also extend along paraspinal muscles and fascia to the facet joints and even into the intervertebral disks.
Direct implantation
This mechanism is usually the result of surgical intervention. Interventions include hip arthroplasty (ie, arthroscopy, implantation of allograft material, arthrocentesis, and hemi and total hip replacements) and even misplaced attempts at vascular catheter insertion. Septic arthritis caused by hip joint injection is, however, exceedingly rare, with a frequency of 1:25,000. Septic processes anterior to the hip joint (such as pyomyositis or fasciitis) may mimic septic arthritis clinically, which may occur when attempts to aspirate what is actually a sterile joint may result in septic arthritis of the hip due to cross-contamination as pathogens are unintentionally introduced into a sterile joint space.
Postoperative
Introduction of a foreign material (ie, prosthetics) into the body may be a source of infection, either acutely due to contamination of the surgical bed or in delayed fashion as the implant serves as a nidus for hematogenous infection. Evaluation of computed tomographic (CT) and MR images is complicated by beam hardening and magnetic susceptibility artifact. Aspiration is often required to confirm the diagnosis. Other noninfectious processes such as particle disease and aseptic lymphocytic vasculitis-associated lesion (ALVAL) can cause effusion, synovitis, erosion, and mass effect, and can result in prosthesis loosening. These findings can also simulate infection.
Imaging Findings: Infection
Cellulitis
Cellulitis is defined as an acute infectious inflammation of the skin and subcutaneous tissues. MR imaging is useful in ruling out underlying myositis, abscess, sinus tract, fasciitis, septic arthritis, and osteomyelitis. Indicators of cellulitis on MR imaging include infiltration of subcutaneous tissues with edema signal due to the inflammatory response and production of serous exudate. Fat in the soft tissues is metabolized, leading to an ill-defined region of low T1 signal and high T2 signal. Contrast is useful to differentiate “bland” or noninflammatory edema from true cellulitis with associated hyperemia ( Fig. 1 ).
Infectious fasciitis
Infectious fasciitis is a life-threatening, invasive soft-tissue infection that is characterized by widespread, rapidly developing necrosis of the subcutaneous tissue and fascia. The severity of the infection and accelerated deterioration of the infection site warrants rapid surgical intervention including debridement and decompression, as well as aggressive antibiotic therapy. MR imaging is sensitive for the evaluation of this process, seen as fascial edema and enhancement; however, without appropriate clinical context fascial edema is not specific for infection and is seen in many conditions ( Fig. 2 ). In addition, sick patients with renal compromise may not be able to tolerate intravenous gadolinium contrast. Therefore, unless clinical suspicion is high or soft-tissue gas is seen on radiographs, fascial edema is normally attributed to innocuous causes. Considering that true infectious fasciitis is a surgical emergency, the long acquisition time of MR imaging may preclude the modality as a sufficient diagnostic tool in this setting. Although MR imaging continues to be useful for evaluating the extent of infection and the existence of underlying abscess or osteomyelitis, CT may be the preferred diagnostic imaging study because of its wide availability, rapid acquisition, and high sensitivity for fascial gas.
Abscess
An abscess is a localized collection of necrotic tissue, fluid, and inflammatory cells that is walled off by a highly vascular and typically irregular inflammatory pseudocapsule. The surrounding soft tissue is also typically involved and displays a variable degree of edema/cellulitis.
On MR imaging, the central cavity of the abscess appears hypointense to muscle on T1-weighted images because of its liquefactive properties. Most abscesses are hyperintense on T2-weighted or short T1 inversion recovery (STIR) images with a variable degree of surrounding soft tissue edema (see Fig. 2 ). Fluid-sensitive sequences tend to show heterogeneous signal within the abscess. Owing to the hypervascular nature of the inflammatory tissue at the margins of the abscess, thick enhancement of the margins is demonstrated following contrast administration. The central portion remains hypointense, making the abscess cavity stand out on fat-suppressed, postcontrast images. The multiplanar capability of MR imaging and its soft-tissue contrast make it the ideal modality for planning of surgery or percutaneous drainage.
Heterotopic bone formation is important in the differential diagnosis for abscess in the pelvis, especially in paralyzed patients. In the early stages of development, heterotopic ossification demonstrates T2 hyperintensity and rim enhancement after gadolinium administration similar to abscess. Careful distinction is warranted in patients with spinal cord injury, who are concomitantly at increased risk of decubitus ulcers and thus abscess formation, as well as heterotopic bone formation. The use of gradient-echo images, which demonstrate blooming artifact with early rim calcification, as well as correlation with radiographs or CT, is useful ( Fig. 3 ).
Pyomyositis
Muscle is inherently resistant to infection. Therefore, hematogenous pyomyositis is relatively uncommon. The incidence is increased in the setting of acquired immunodeficiency syndrome or iatrogenic immunosuppression (associated with solid organ transplantation, bone marrow transplantation, or chemotherapy), as well as intravenous drug abuse. The most common site of involvement is the lower extremity, in particular the thigh. Multifocal involvement is seen in slightly less than half the cases. Secondary muscle infection may also occur as a result of contiguous spread from adjacent structures. MR imaging is highly sensitive for detecting pyomyositis. Hyperintensity is seen on T2-weighted or STIR images. Diffuse disease (stage 1) most commonly responds to conservative (antibiotic) therapy. On T1-weighted images, the muscle may appear enlarged but the signal may appear normal. Perifascial fat infiltration may be seen on both T1-weighted and T2-weighted sequences. Postcontrast imaging may show diffuse enhancement in the early stages of disease and therefore help separate this process from other entities such as diabetic myonecrosis. In later stages, however, superimposed necrosis may occur, resulting in abscess formation and subsequently heterogeneous enhancement. With disease progression, more focal fluid collections may be observed (stage 2 disease). Postcontrast images demonstrate rim enhancement, suggestive of small abscesses. Stage 2 disease often warrants a more aggressive approach, with surgical drainage and debridement of necrotic tissue. Contrast-enhanced sequences can often provide the surgeon with a roadmap, helping to delineate fluid collections, sinus tracts, and areas of necrosis (see Fig. 2 ). Stage 3 disease is defined as the extension to adjacent structures, resulting in septic arthritis, osteomyelitis, or septicemia. Pyomyositis of the muscle adjacent to the hip requires an accurate diagnosis, as it may be mistaken for septic arthritis of the hip and lead to complications if aspiration is attempted. Muscle edema on MR imaging is nonspecific and often results in a wide differential diagnosis including but not limited to injury, denervation, rhabdomyolysis, infarction, diabetic myonecrosis, polymyositis, and tumoral infiltration (sarcoma, lymphoma, or metastatic disease). Therefore, the value of clinical correlation is of utmost importance.
Septic bursitis
Hematogenous septic bursitis at the hip is rare; usually it is due to the contiguous spread of infection, especially in paralyzed patients at an increased risk for ulcers or patients with penetrating trauma. With respect to the hip, the greater trochanteric bursa is most frequently involved, secondary to trochanteric ulceration. Septic arthritis of the hip joint may decompress through the hip capsule into the iliopsoas bursa, causing iliopsoas septic bursitis ( Fig. 4 ). Bursae are lined by synovium similar to joints, making MR imaging manifestations of bursal infection similar to those seen in septic arthritis. Focal fluid signal corresponding to the bursal location with thick rim enhancement is characteristic. However, this finding is not specific, and mechanical bursitis or inflammatory bursitis related to rheumatoid arthritis can appear identical and should be ruled out by further evaluation. Obese patients often demonstrate small amounts of incidental fluid in the greater trochanteric bursae, generally bilateral and symmetric. Paralyzed patients are prone to the development of heterotopic ossification at the hip bursae, which, as mentioned in the abscess section earlier, may appear similar to infection with fluid signal and rim enhancement in its early stages.
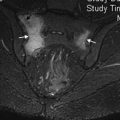
Septic arthritis
MR imaging is sensitive for the detection of joint effusion, which is a hallmark feature of any type of arthritis. In septic arthritis, fluid is often complex, particularly in chronic infection. However, complex effusion is also found in noninfectious inflammatory arthropathies such as rheumatoid arthritis. On postcontrast imaging thick rim enhancement is characteristic of septic arthritis. In a study examining transient synovitis and septic arthritis, the presence of signal alteration of normal bone marrow on both contrast-enhanced fat-suppressed T1-weighted and T2-weighted sequences was seen in septic arthritis and excluded the diagnosis of transient synovitis. The hyperemia induced in septic arthritis can lead to subchondral edema. Contrast use can help localize extra-articular collections and sinus tracts, helping to delineate extent of infection ( Fig. 5 ). Marrow edema and enhancement beyond the subchondral bone into the medullary cavity denotes possible osteomyelitis. MR imaging can assess the status of the articular cartilage, which is quickly eroded in septic arthritis. In later stages, erosions occur at the femoral neck and frank bone destruction may occur. Early detection and treatment of hip joint infection is essential to avoid chondrolysis and rapid development of osteoarthritis. Joint aspiration and antibiotic coverage is paramount in suspected septic arthritis of the hip.
Osteomyelitis
MR imaging is the ideal imaging modality for detection of marrow infection and extension because of its high tissue contrast resolution and multiplanar capability coupled with high spatial resolution. Sensitivity and specificity of MR imaging for detecting osteomyelitis reaches 90% to 100%. Osteomyelitis is demonstrated on T1-weighted images by marrow hypointensity (ie, replacement of marrow fat signal) with edema and enhancement (see Fig. 5 ).
Unlike infection, hematopoietic marrow is symmetrically distributed. It also retains minimal fat signal and enhances minimally, if at all. Clinical findings should be incorporated with the imaging features because cellular infiltration from tumor, as well as trauma and infarction, may produce similar T1 and T2 marrow signal abnormalities. A linear pattern of edema with enhancement along the outer cortex is characteristic of associated periosteal reaction. Periostitis is not as prominent in flat bones such as the iliac bone, so it may be absent in infection around the hip unless the proximal femoral shaft is involved. Bony destruction may be seen in later stages of disease progression, characterized by loss of the low-signal cortical line and mass effect from phlegmon or abscess.
For situations in which osteomyelitis requires surgical debridement, MR imaging is valuable in defining the extent of osseous involvement. Usually the margin of infected bone is well demonstrated on all sequences, although the extent may appear more prominent on STIR or fat-suppressed T2-weighted images compared with T1-weighted images, due to the high sensitivity of these sequences for reactive hyperemia of the surrounding bone. Soft-tissue extent may also be demonstrated, including sinus tracts, septic arthritis, and periarticular abscesses.
Despite the poor spatial resolution the STIR sequence is extremely sensitive to fluid. Thus, the absence of signal abnormality on STIR images or lack of pathologic contrast enhancement on fat-suppressed T1-weighted images effectively excludes the diagnosis of osteomyelitis. MR imaging may discern between a primary soft-tissue infection and secondary osteomyelitis or vice versa by paying attention to a few distinguishing features. In the former, a soft-tissue phlegmonous mass with cortical erosion and subcortical marrow abnormality can be seen. Absence of T2 signal abnormality virtually excludes superimposed osteomyelitis. Occasionally, reactive edema can extend into the medullary bone beyond the subchondral location. There is evidence that the brighter the T2 signal abnormality, the more likely the edema is secondary to osteomyelitis rather than to reactive hyperemia.
However, in this situation, the MR imaging examination must still be considered suspicious for osteomyelitis regardless of the intensity.
MR imaging is also useful for diagnosing active infection in areas complicated by trauma or prior surgery. Despite artifact, adjacent fluid collections, periostitis, and marrow replacement can be delineated. Contrast enhancement can be useful in this setting; precontrast and postcontrast imaging can be performed to detect subtle areas of hyperemia around areas of susceptibility. Contrast can also distinguish nonenhancing areas of infarction from rapidly enhancing hyperemia due to infection. In the setting of sickle-cell disease, the 2 are difficult to distinguish, because reactive hyperemic zones often marginate areas of infarction. These hyperemic zones enhance and may even have periosteal reaction if the infarct is acute.
Chronic osteomyelitis, commonly seen in paralyzed patients, can present with atypical patterns on MR imaging because of the wide spectrum of chronicity, activity, and the body’s response. It is often characterized radiographically by a mixed pattern of lysis, sclerosis, and cortical thickening, typically at the ischeal tuberosity, sacrum, and greater trochanter. Sclerosis may be a low signal on both T1-weighted and T2-weighted images, with granulation tissue representing active infection, demonstrating hyperintensity on T2-weighted images and enhancement on contrast-enhanced images. Sequestrum formation, which is seen as intraosseous foci of hypointensity on all sequences surrounded by enhancing inflammatory tissue, is important to recognize. These foci represent avascular fragments of necrotic bone that may be a source for continuous infection and often require debridement. Cortical thickening representing long-standing periostitis may also demonstrate low signal intensity; active periostitis, as earlier, is seen on MR imaging as linear edema and enhancement along the outer cortical margin. Sinus tracts are often present in patients with active chronic osteomyelitis, visualized as irregular, linear T2-hyperintense streaks through the soft tissues with surrounding fat replacement and tram-track enhancement. These tracts arise from ulcers and dissect through the soft tissues. Tracts often communicate with abscess cavities. Infections often extend far from the source; because of the complicated patterns of spread through the soft tissues, MR imaging is an essential part of the preoperative algorithm.
Infection of the Postoperative Hip
Infection is an uncommon complication after hip arthroplasty, seen after less than 1% of procedures. Patients may present shortly after surgery (assuming implantation) or in delayed fashion, presumably related to hematogenous spread, with the implant acting as a nidus. Patients present with pain and difficulty bearing weight. There may be a low-grade fever, but in early stages this is not common. Laboratory values such as sedimentation rate, leukocyte count, and other markers are nonspecific. Aspiration with fluid analysis is essential, but MR imaging is a useful adjunct to the workup.
Assessing a patient for suspected infection postoperatively can present as a challenge, particularly in cases of total hip arthroplasty. Imaging is problematic because of metallic susceptibility artifact. To reduce the effect of metallic artifact in such cases, various changes are applied to the imagining protocol :
- •
Maximizing bandwidth
- •
Using STIR instead of fat-saturated T2-weighted sequences
- •
Using fast-spin echo instead of spin echo (SE) sequences
- •
Avoiding gradient-echo sequences
- •
Lowering time to echo (TE) on STIR and fat-saturated SE sequences, that is, change to 30 to 40 ms
- •
Using a large field of view and increasing the matrix
- •
Performing precontrast and postcontrast T1-weighted non–fat-saturated sequences
Despite artifact, MR imaging remains useful for the evaluation of the periprosthetic soft tissues (particularly for detection of abscesses and sinus tracts) and the adjacent marrow, as well as for defining the spread of infection ( Fig. 6 ). By implementing metal artifact reduction techniques mentioned earlier, adequate images can be acquired with most prosthesis types. Equipment vendors are developing new metal artifact reduction sequences that will likely make this less of an issue in the future.