Cartilage abnormalities in the knee and ankle are a common source of pain and are often difficult to diagnose clinically or radiographically. MR imaging is a valuable tool for diagnosing and characterizing cartilage lesions of both the knee and ankle. An understanding of the appearance of cartilage, and an understanding of how and when to report cartilage injury in the knee and ankle based on current grading systems allows the radiologist to provide the most helpful reports to referring clinicians. This article presents the range of cartilage pathologies in the knee and ankle and provides clinically relevant guidelines.
Introduction to cartilage lesions
Clinical Background
Cartilage lesions of the knee and ankle are common problems that are not easily detected by routine physical examination. In addition, cartilage lesions may be overlooked as the source of many joint symptoms, especially in the setting of a joint comorbidity. It is important for clinicians to diagnose cartilage disease correctly, as these abnormalities can be the cause of significant short and long-term morbidity. Cartilage has minimal repair capability, and untreated lesions can lead to persistent joint pain and dysfunction. Moreover, alterations in joint forces related to cartilage lesions are thought to accelerate osteoarthritis of both the knee and the ankle. Fortunately, there are new techniques for both the diagnosis and surgical treatment of cartilage lesions that have demonstrated good outcomes in recent years.
Diagnosing cartilage lesions with the “gold standard,” invasive technique of arthroscopy, is not practical for all patients. Magnetic resonance (MR) imaging of articular cartilage is an alternative that has been found to be a valuable tool not only for lesion detection but also for preoperative planning and postoperative assessment. Accurate characterization of cartilage lesions with state-of-the-art MR imaging techniques allows clinicians to choose optimal treatments for their patients. Therefore, understanding the appearance of normal articular cartilage, the spectrum of cartilage lesions, and the treatment options for these lesions in the knee and ankle will allow radiologists to more effectively guide treatment decisions.
Knee Cartilage Versus Ankle Cartilage
There are many differences between the articular cartilage of the knee and ankle. Having some understanding of these differences may help the radiologist to better appreciate the differences in the types of lesions seen clinically, as well as their imaging appearance.
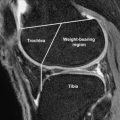
Biomechanical studies suggest that variations between the articular cartilage of the knee and ankle cannot be explained by anatomic and biomechanical differences alone; rather, there are many intrinsic differences between knee and ankle cartilage. Ankle cartilage is significantly thinner than knee cartilage, with a mean thickness of approximately 1.1 mm (range, 0.4–2.1 mm), whereas knee cartilage can be up to 5 mm thick. It has been suggested that more congruent joints such as the hip and ankle support compressive loads with a thinner cartilage because the load is spread over a greater area. The collagenous organization of knee and ankle articular cartilage is similar; however, the chondrocyte distribution is different. In the superficial zone of ankle cartilage, chondrocytes are arranged in clusters, whereas they are distributed as single chondrocytes in the superficial zone of the knee. Ankle cartilage has been shown to have significantly higher glycosaminoglycan (GAG) content than knee cartilage. Most important, the stiffness of ankle cartilage allows for better resistance to damage than that of knee cartilage.
Although cartilage has limited repair potential, ankle cartilage has a more favorable biochemical response to injury than knee cartilage. In multiple studies, chondrocytes of the ankle were found to be more metabolically active than those of the knee after controlled mechanical stress was applied. Specifically, ankle chondrocytes produced larger amounts of proteoglycans and collagen, an overall anabolic response, whereas the knee chondrocytes produced an overall catabolic response. Thus, although thinner, ankle cartilage has many features that make it more resistant and resilient to trauma and wear. These properties may explain why the types of cartilage lesions seen in the knee and ankle differ. Idiopathic osteoarthritis is commonly seen in the knee, whereas osteochondral lesions are more commonly seen in the ankle.
MR imaging appearance of normal knee and ankle cartilage
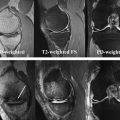
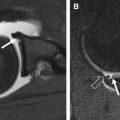
Articular cartilage has a layered appearance on MR imaging composed of a low-signal deep layer, a thicker intermediate to bright middle layer, and a thin low-signal surface layer. This trilaminate appearance is best seen with high-resolution, high–field-strength imaging ( Fig. 1 ). With lower resolution imaging techniques or very short echo time (TE) acquisitions, normal cartilage may appear homogeneously intermediate to bright, as the deep and superficial layers may not be distinctly seen; this is especially true for the thin cartilage of the ankle ( Fig. 2 ). Fat suppression can further decrease the conspicuity of the deep short T2 layer of cartilage because the subjacent subchondral bone and suppressed marrow fat may have similar signal intensity ( Fig. 3 ). Cartilage normally demonstrates regional variations in signal intensity, largely due to variations in T2 caused by the orientation of the collagen fibrils relative to the magnetic field. Normal variation in cartilage signal is smooth, whereas true cartilage abnormalities usually demonstrate abrupt signal change. Linear regions of fluid signal intensity within cartilage usually represent fissures whereas larger regions indicate cartilage loss. Focal regions of low T2 signal may also represent cartilage damage, often fissures, as shown in a recent small case series. Knowledge of the normal variations of signal within the articular cartilage of the knee and ankle can help radiologists to differentiate normal regions of low and high signal from true cartilage abnormalities.