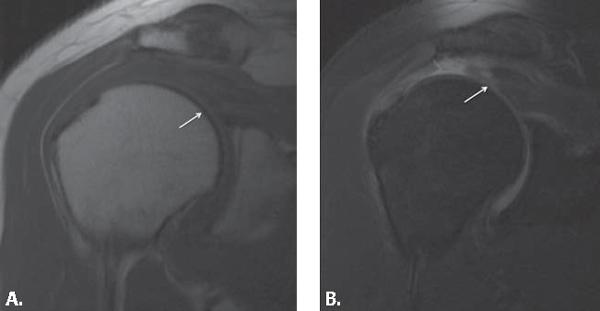
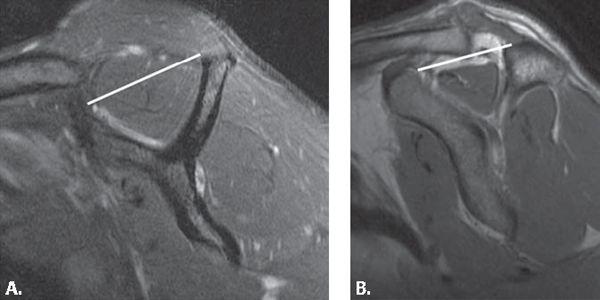
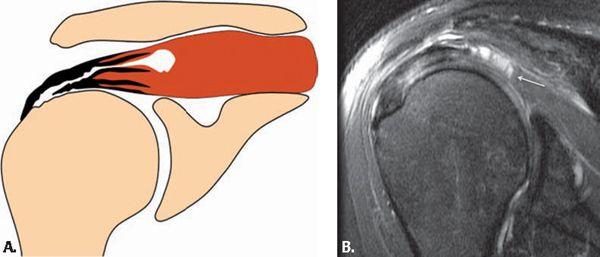
FIGURE 4.43 This partial articular tear with intratendinous extension (PAINT) lesion is well seen on fat-suppressed T1-weighted (A) coronal and (B) abduction and external rotation images obtained from an MR arthrogram. Notice the contrast extending into the tendon from the articular surface and then spreading through the tendon in a laminar fashion (arrow).
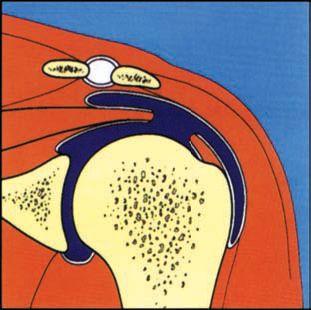
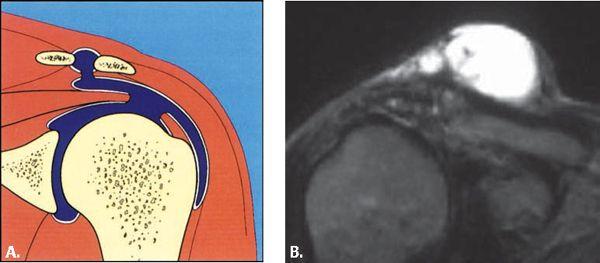
FIGURE 4.44 Schematic diagram demonstrating how a full-thickness tear extends from the glenohumeral joint through the superior tendon surface and communicates with the subacromial subdeltoid bursa (all in blue).
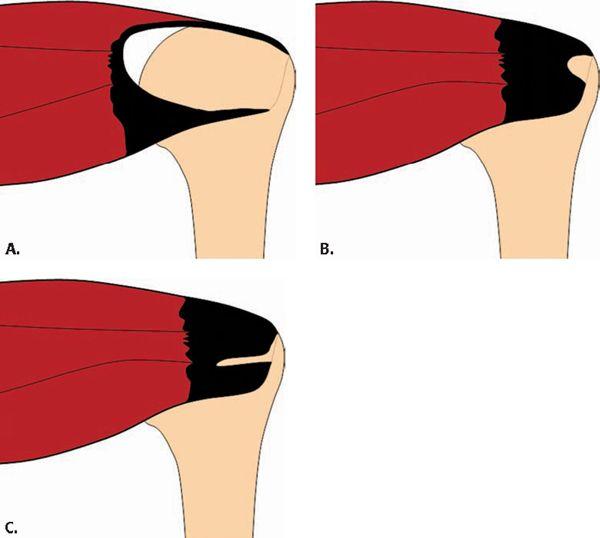
The size of the full-thickness tear should be reported in the medial to lateral direction on the coronal plane and anterior to posterior extent in the sagittal plane. The quality of tendon regarding fraying and signal intensity should also be reported. The shape of a rotator cuff tear has implications for surgical repair and appearance on MRI. Full-thickness tears fall into three different shapes on arthroscopy as viewed from the articular surface. These include the U-shaped, crescentic, and L-shaped tears (131, 132) (Fig. 4.45). U-shaped tears represent massive tears that extend medially to the level of the glenoid fossa. These are treated with side-to-side suturing of the anterior and posterior portions with reattachment of the transverse free margin to the bone. Crescentic tears are characterized by the tendon pulling away from the greater tuberosity without much retraction. These can be reattached to bone with minimal tension. L-shaped tears are massive tears with a longitudinal component along the plane of the rotator cuff fibers with a transverse component along the insertion of the tendon.
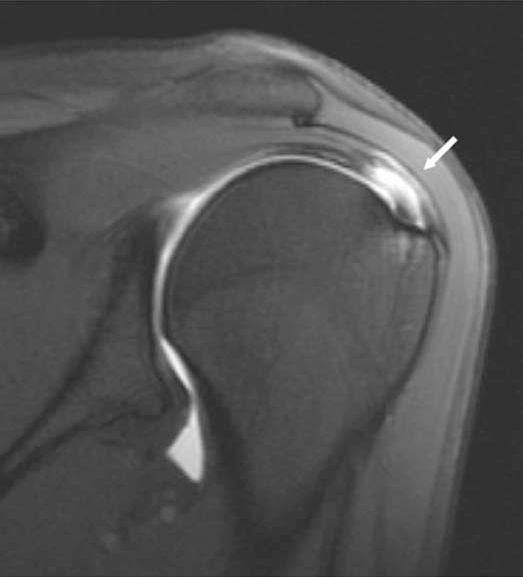
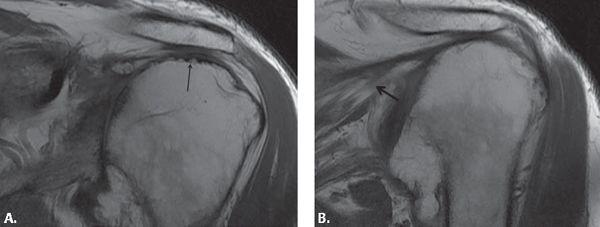
MR findings in full-thickness rotator cuff tears include one or more of the following signs: disruption of the low-signal–intensity tendon by an area of abnormally higher signal intensity on short tau inversion recovery (STIR), T1-, T2-, or T2*-weighted images (Fig. 4.46); tendon retraction (Fig. 4.47); muscle atrophy and fatty replacement (Figs. 4.47 and 4.48); absence of the tendon; acromiohumeral articulation; and fluid in the SASD bursa.
The size of the full-thickness rotator cuff tear has implications for surgical prognosis and repair and should be reported. One classification is based on the greatest dimension as either small (less than 1 cm), medium (1–3 cm), large (3–5 cm), or massive (greater than 5 cm) (133). Like with partial tears, it has also been shown in 10% of cases with full-thickness tears that fibrous and granulation tissue can fill in the tear producing low signal intensity on T2 weighting (77). In such cases, the imager can look for abnormal tendon morphology such as attenuation or irregularity of the rotator cuff tendon (77).
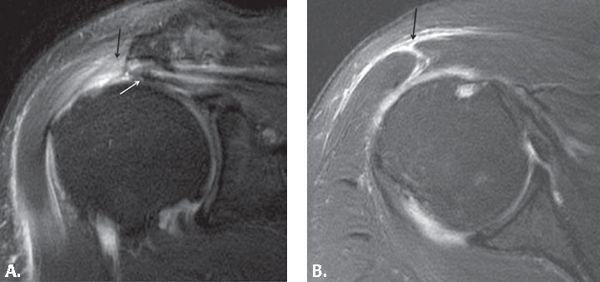
Full-thickness tears of the rotator cuff tendons can be accurately identified using conventional nonarthrographic MRI with high sensitivity and specificity (18, 41, 49, 78, 104). Increased signal intensity extending from the inferior to the superior surface of the tendon on all imaging sequences is an accurate sign of a full-thickness rotator cuff tear (76). Like with partial-thickness tears, use of the fat-saturation technique with fast spin-echo imaging can improve detection of full-thickness tears compared with standard spin-echo imaging techniques (122). In one study, the fat-saturation technique increased sensitivity for detection of full-thickness tears from 80% to 100% (122). MR arthrography can aid in separating a high-grade partial- from a full-thickness tear in equivocal cases (Fig. 4.48).
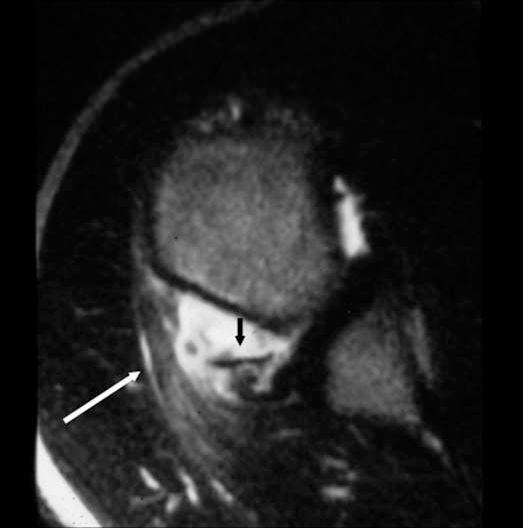
Tendon retraction is a specific sign of a full-thickness rotator cuff tear (41). The musculotendinous junction should lie no further medial than 15 degrees from a line drawn through the 12-o’clock position of the humeral head (41). Retraction can also be defined when the musculotendinous junction lies medial to the glenoid rim (Fig. 4.47). However, medial retraction may not represent true retraction, because physiological load on the tear margins with certain types of tears such as a U-shaped tear can make them look like they cannot be repaired, yet they are mobile on arthroscopy. One grading system that is used from the coronal plane is: stage 1, adjacent to the tendon insertion; stage 2, retraction superior to the humeral head; and stage 3, proximal retraction to the glenoid margin. Severe muscle atrophy and fatty replacement are common in patients with large rotator cuff tears (39, 111, 134). Absence of the tendon and acromiohumeral articulation are signs of a chronic rotator cuff tear.
FIGURE 4.45 Three different types of full-thickness tears as seen from the articular surface by arthroscopy include (A) U, (B) crescentic, and (C) L shapes.
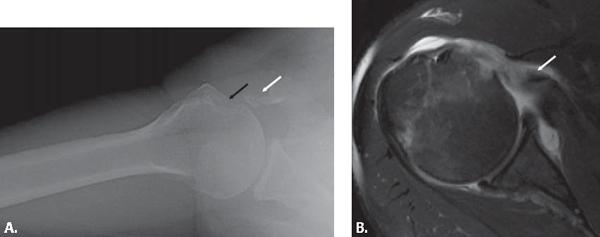
Massive rotator cuff tears that are not treated progress to rotator cuff arthropathy, which is characterized by acromiohumeral articulation, leading to bone erosions and humeral head collapse (Fig. 4.49). The conventional radiograph is useful for identifying acromiohumeral articulation. When the distance between the acromion and the humeral head is less than 7 mm, a rotator cuff tear is likely. There is no need to perform other studies to exclude a tear in this situation. However, additional studies such as MRI would be indicated if the referring clinician desires information about which tendons are torn as well as the general condition of other structures in and around the glenohumeral joint, including the muscles, labrum, and biceps tendon (Fig. 4.50). In addition to internal glenohumeral joint derangement, deltoid dehiscence is seen after massive rotator cuff tears (Fig. 4.50).
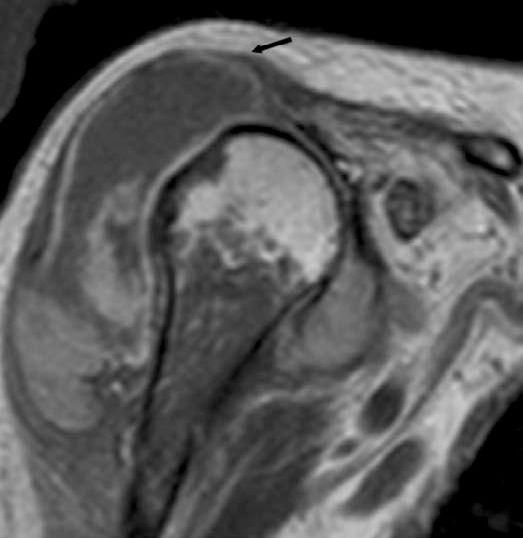
Muscle atrophy and fatty degeneration are separate features that should be assessed in cases of rotator cuff tear. Both of these abnormalities indicate a poorer surgical outcome, especially fatty infiltration. Muscle cross-sectional area can be assessed subjectively. The supraspinatus muscle can be more objectively evaluated using the scapular ratio and the “tangent sign,” which are both measured in the oblique sagittal plane at the level of the medial coracoid process (Fig. 4.51). The tangent sign is positive for supraspinatus muscle atrophy when the supraspinatus muscle does not extend above a line drawn from the superior margin of the coracoid process to the superior border of the scapular spine (135). The scapular ratio is determined by comparing the ratio of the cross-sectional area of the supraspinatus muscle with the area of the supraspinatus fossa at this level on the sagittal image. If the ratio is less than 50%, atrophy is present (136). Cross-sectional measurements can be done but are not practical for routine MRI. Such measurements correlate with muscle strength (137). Fatty infiltration is also a component related to poor surgical outcome with a likelihood of a recurrent tear. Fatty infiltration of the rotator cuff muscles is usually present in the setting of chronic rotator cuff tears but may occur also in cases of denervation and glenohumeral osteoarthritis without rotator cuff tear. Large anterosuperior rotator cuff tears are associated with fatty infiltration of the neighboring infraspinatus and subscapularis muscles in the absence of tears of those tendons (138, 139). This pattern of fatty infiltration also portends a poor prognosis for rotator cuff repair related to decreased depressor function, resulting in supraspinatus tendon impingement (140).
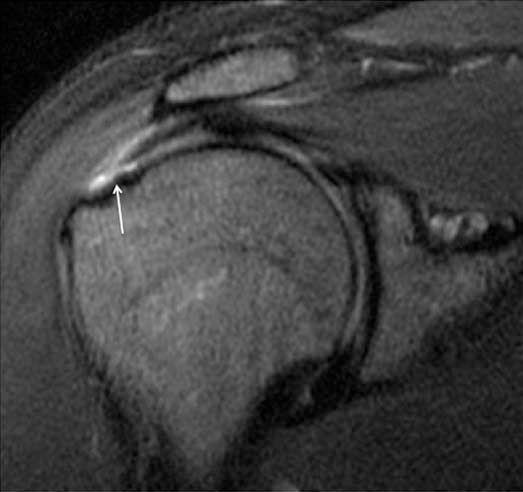
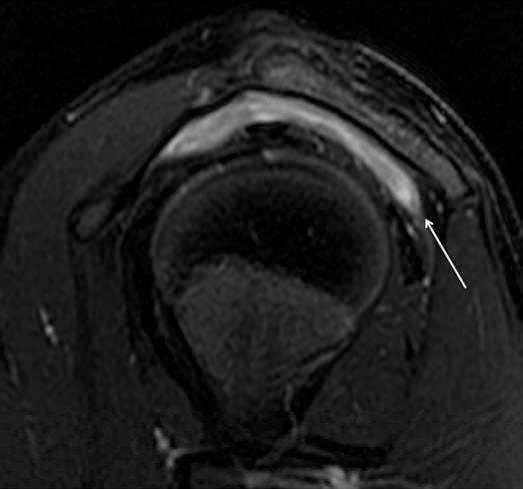
FIGURE 4.46 Small full-thickness tear of the supraspinatus tendon. The high-signal–intensity tear is located at the footprint on this coronal fat-suppressed T2-weighted image (arrow).
FIGURE 4.47 Large full-thickness supraspinatus tendon tear. (A) Coronal T1-weighted and (B) fat-suppressed T2-weighted images show the full-thickness gap with retraction of the musculotendinous junction medial to the glenoid (arrow).
Fluid in the SA-SD bursa is a sensitive but relatively nonspecific finding in patients with rotator cuff tears (41). The fluid escapes from the glenohumeral joint through the articular surface tear into the bursa that lies above the superior surface of the tear. Small amounts of fluid in the bursa can be seen as an isolated finding in asymptomatic patients (40, 42, 49, 97, 98, 141). Occasionally the fluid of the SA-SD bursa will communicate with a subcoracoid bursa. Because of this, the distended subcoracoid bursa is sometimes seen in association with a full-thickness rotator cuff tear.
Cases of isolated SA-SD bursitis without rotator cuff tear are identified after trauma and in association with inflammatory disorders such as rheumatoid arthritis or infection (Fig. 4.52). SA-SD bursitis is also common with impingement syndrome as described previously in this chapter. Injections can also produce fluid in the bursa.
If there is any question concerning the distinction of a full- and partial-thickness tear, MR arthrography is recommended (Fig. 4.48) (125). When gadolinium is injected into the glenohumeral joint, it fills a defect in the rotator cuff that extends to the articular surface, including partial-thickness undersurface tears. The fluid-sensitive sequences are used to show a partial tear in the substance or at the superior surface of the rotator cuff tendons during MR arthrography. The gadolinium imbibes into regions of tendinosis that are not torn. The contrast also fills in frayed and friable tendon margins. Tendons that imbibe contrast have increased signal intensity on fat-suppressed T1-weighted images. These tendons are often friable and swollen, related to degeneration and inflammation. Damaged tendon edges that imbibe contrast are débrided before repair of the cuff. If the tear is full thickness, the contrast enters the SA-SD bursa. On an MR arthrogram, the SA-SD bursa must be carefully evaluated for the presence of contrast in patients with equivocal full-thickness tears (Fig. 4.48). It is important to use fat suppression to decrease the signal from fat without affecting the high signal intensity of the gadolinium on T1-weighted images (125).
FIGURE 4.48 Full-thickness supraspinatus tendon tear on MR arthrogram. The contrast extends from the articular to the bursal side of the supraspinatus tendon with flow into the subacromial bursa, confirming that this is a full-thickness rather than a high-grade partial tear on this coronal fat-suppressed T1-weighted image (arrow).
FIGURE 4.49 Rotator cuff arthropathy with a high-riding shoulder. A: A supraspinatus tear is identified with absence of the tendon and acromiohumeral articulation (arrow). B: There is also a tear of the infraspinatus tendon with muscle atrophy and fatty infiltration (arrow) on these coronal T1-weighted images. The humeral head is irregular and flattened superiorly and there is glenohumeral joint narrowing with abnormal subchondral signal, cartilage loss, and an inferomedial humeral head osteophyte.
Infraspinatus, Teres Minor, and Subscapularis Tendon Tears
An increasing role is being placed on the infraspinatus tendon as a source of glenohumeral joint symptoms (142). Although commonly torn in association with supraspinatus tendon tears, isolated tears of the infraspinatus tendon are rare (143) (Fig. 4.53). Isolated tears are frequently related to posterior instability of the shoulder. Tears of the infraspinatus are more often seen in younger athletes who use overhead motion. Rare cases of rupture at the musculotendinous junction with muscle edema and eventual fatty atrophy have also been described producing acute pain and weakness in external rotation (144). Those patients are often young and have a high association of other pathology of the rotator cuff tendons, including HADD, tendinosis, and partial tears. Some of them have had injections, which may have disrupted the tendon. The infraspinatus tendon may also be affected by the previously described internal impingement syndrome. Tears of this tendon are best identified with the aid of all three imaging planes.
Subscapularis tendon tears are seen in patients with anterosuperior and subcoracoid impingement (Fig. 4.32) as well as in middle-aged and older patients with recurrent anterior shoulder dislocation or in association with massive tears of the other rotator cuff tendons (62, 63, 145–149). A recent article confirms the relationship between some subscapularis tendon abnormality and chronicity of supraspinatus tendon tears (150). Tears may also be seen after direct trauma to the anterior aspect of the shoulder and with hyperextension or external rotation of the adducted arm (151). In the latter case, the patient experiences pain and weakness when the arm is used below shoulder level.
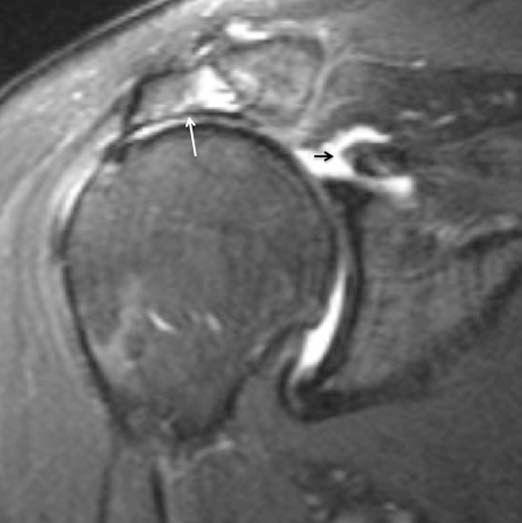
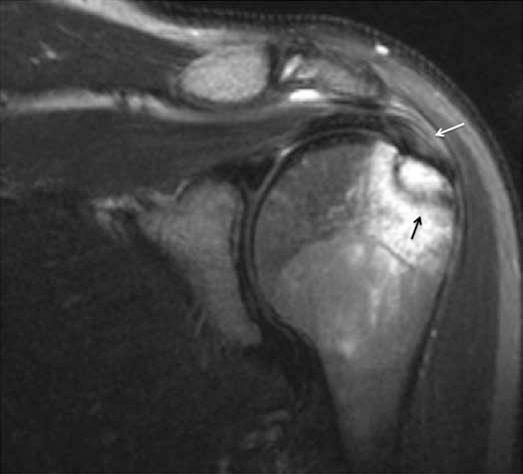
FIGURE 4.50 Massive supraspinatus tear with retraction (white arrow) and deltoid dehiscence (black arrows) seen on fat-suppressed T2-weighted (A) coronal and (B) axial images.
FIGURE 4.51 Tangent sign for supraspinatus atrophy. A: A normal supraspinatus muscle extends far above the tangent line drawn between the medial coracoid process and the scapular spine on the “y view.” B: The supraspinatus muscle is atrophied and lies below the tangent line in this patient who has a supraspinatus tear.
Partial tears of the subscapularis tendon are most frequent along the articular portion in the superior aspect of the tendon (Fig. 4.32). On MRI, subscapularis tendon tears are often identified on axial and oblique sagittal images. Partial tears can be subtle. Full-thickness tears are frequently seen at the attachment to the lesser tuberosity and are associated with retraction.
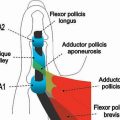
In the presence of a subscapularis tendon tear, the biceps tendon may sublux or dislocate out of the intertubercular groove. In approximately 30% of cases of partial subscapularis tendon tear, the biceps dislocates into the tear (Fig. 4.54) (148). The biceps tendon occasionally lies in front of the glenohumeral joint. This is because of a disruption of an extension of the coracohumeral ligament and subscapularis tendon over the intertubercular groove, formerly known as the transverse humeral ligament, which allows the tendon to escape the bicipital groove (152, 153).
FIGURE 4.52 Isolated subacromial subdeltoid bursitis in a patient with inflammatory arthropathy seen on a sagittal fat-suppressed T2-weighted image (arrow).
FIGURE 4.53 Isolated full-thickness infraspinatus tendon tear. The tendon is completely torn at the footprint with medial retraction (arrow).
FIGURE 4.54 Partial subscapularis tendon tear with biceps dislocation. The biceps tendon is dislocated into the partial tear of the subscapularis tendon (white arrow). The overlying extension of the subscapularis to the greater tuberosity is still intact on this fat-suppressed T1-weighted axial MR arthrogram (black arrow).
The subscapularis tendon may also avulse off of the lesser tuberosity. Osseous fragments lie anterior and medial to the humeral head and they may not be well seen on an MRI (Fig. 4.55).
Teres minor tendon tears are rare. The superior fibers may be involved when there is a massive rotator cuff tear that affects the other tendons. Teres minor tendon tears may also occur in association with infraspinatus tendon tears and posterior capsular trauma related to posterior dislocation (Fig. 4.56). It is important for the clinician to check the posterior labrocapsular structures for abnormalities when such a tear is present. Teres minor muscle strains may also be an important clue to underlying posterior glenohumeral instability.
Ancillary Findings Associated With Rotator Cuff Tears
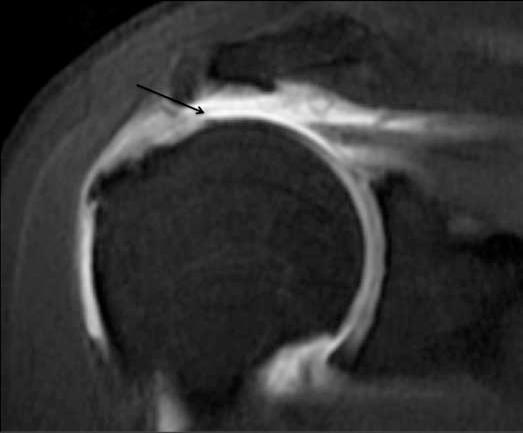
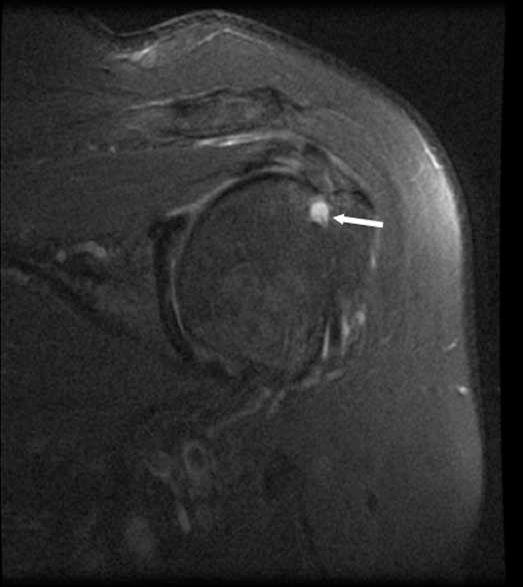
An intramuscular “sentinal” cyst may form in sheath or substance of the rotator cuff muscles when fluid from the joint propagates along a laminar partial or full-thickness tear into the musculotendinous junction (154, 155) (Fig. 4.57). These cysts present as a high-signal–intensity mass on T2-weighting and STIR images with rim enhancement after intravenous gadolinium injection. When seen on MRI, intramuscular rotator cuff cysts suggest that there a high likelihood of an underlying rotator cuff tendon tear. The cysts are more commonly seen in association with partial-thickness tears, comprising half of the tears in one study (155). It is interesting that in some cases, the cyst can propagate from a torn tendon into an adjacent rotator cuff muscle with an intact tendon related to interdigitation of tendons as they insert on the humerus. MR arthrography and ABER positioning may aid in demonstration of partial undersurface tears related to an intramuscular cyst, demonstrating intrasubstance propagation of the tear through delaminated layers of the torn tendon.
Large glenohumeral joint effusions are often seen with advanced rotator cuff abnormalities (65). In addition, the presence of a fluid-filled mass above the AC joint should prompt a search for a rotator cuff tear (156–158) (Fig. 4.58). AC joint cysts are rare, but usually occur when there is communication between the glenohumeral and AC joints in patients with full-thickness rotator cuff tears. It is believed that there is chronic friction between the high-riding humeral head and the AC joint leading to mechanical wear and tearing of the inferior articular capsule of the AC joint. This leads to passage of fluid from the glenohumeral joint through the rotator cuff tear and the subacromial bursa into the AC joint (157). The AC joint capsule dilates, resulting in a superior cystic mass. Simple aspiration of the cyst should be avoided, because recurrence is likely in the presence of a rotator cuff tear. Nonsurgical treatment is performed if the patient is elderly with acceptable function and without shoulder pain. In patients with functional impairment or chronic shoulder pain, the rotator cuff is repaired and the cyst removed. If the tear is massive and cannot be repaired, it is recommended that the cyst be excised accompanied by acromioplasty and distal clavicular resection. Alternatively, humeral head arthroplasty has been recommended as a treatment by some orthopaedists (159).
FIGURE 4.55 Subscapularis tendon avulsion. A: The axillary radiograph shows several fragments anterior and medial to the humeral head (white arrow) with a defect in the lesser tuberosity (black arrow). B: The retracted tendon and the attached low-signal avulsion fragment are seen on the axial T2-weighted MRI (arrow). The bicepsis still normally located in the groove.
FIGURE 4.56 Teres minor tendon tear caused by posterior instability. Besides the tear of the teres minor tendon seen on this axial fat-suppressed T2-weighted image (white arrow), there is an avulsion of the posterior capsule with an osseous fragment (black arrow).
A chronically high-riding humerus related to a massive rotator cuff tear can produce “faceting” or “acetabularization” of the acromial undersurface. The rounded humeral head produces chronic erosion of the normally straight or convex margin, resulting in a concave articular margin (Fig. 4.59). These findings correlated with large tears of the tendons and fatty infiltration of the infraspinatus muscle (160).
Deltoid tearing and dehiscence are also seen with a chronic high-riding shoulder related to the contact between the humeral head and this muscle and tendon (161). Deltoid muscle and tendon tears may be associated with intramuscular cysts or ganglia and subcutaneous edema or fluid-like signal intensity overlying the deltoid (162) (Fig. 4.60). “Cuff arthropathy” is the term used for an end stage of rotator cuff failure where there is a high-riding humerus related to massive rotator cuff tears, glenohumeral joint degenerative change with significant cartilage loss, and osteophytes, effusions, bodies, and subluxation. There is a strong correlation between rotator cuff tears and articular cartilage degeneration (163) (Fig. 4.61). The cartilage is subjected to abnormal joint mechanics as a result of loss of the normal stabilizing function of the rotator cuff. There is also impaired cartilage nutrition resulting from leakage of synovial fluid and joint immobility, producing atrophy and subchondral osteoporosis. Cartilage damage is not exclusive to end-stage rotator cuff disease. In one study, glenohumeral cartilage lesions were found in up to a third of patients referred for MR arthrography for subacromial impingement syndrome (164). Biceps tendon tears proximal to the intertubercular groove are also common with tears of the supraspinatus and subscapularis tendons and with high-riding shoulder in general (165).
FIGURE 4.57 An intramuscular cyst in the rotator cuff is often associated with laminar partial- or full-thickness rotator cuff tear. A: Diagram and (B) fat-suppressed T2-weighted MR image of a partial articular-sided tear extending in a laminar fashion toward the muscle, resulting in an intramuscular cyst (arrow).
FIGURE 4.58 A: Schematic diagram and (B) oblique coronal T2-weighted MR image demonstrate an acromioclavicular joint cyst in association with a full-thickness tear of the supraspinatus tendon. The fluid extends from the glenohumeral joint through the tendon tear into the subacromial–subdeltoid bursa and then into the acromioclavicular joint, which communicates with the bursa as a result of friction of the high-riding humeral head in the setting of a rotator cuff tear against the acromial surface. B courtesy of Suzanne Anderson, MD.
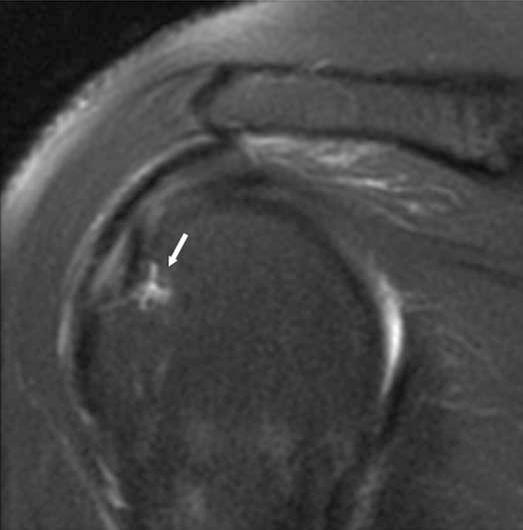
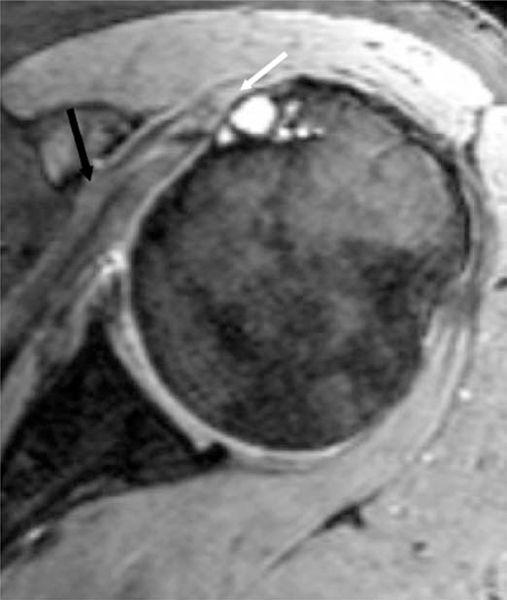
Cystic changes at the supraspinatus tendon footprint on the anterior greater tuberosity are correlated with disorders of the supraspinatus tendon (166). Although not always correlated with supraspinatus tendon pathology, cysts of the anterior greater tuberosity are seen more commonly in patients with partial–thickness, articular-sided tears, suggesting that synovial fluid intrusion may play a role (Fig. 4.62). Posterior cysts are more common than anterior greater tuberosity cysts and are not usually associated with rotator cuff pathology, although they can be seen in the setting of posterosuperior glenoid impingement. Vessels are common in the posterolateral humeral head as well and these should not be mistaken for abnormality (Fig. 4.63). Although sometimes idiopathic, cysts in the lesser tuberosity are frequently seen in the setting of subscapularis tendon tears and muscle fatty atrophy (149). This may also be the result of impingement of the lesser tuberosity (subcoracoid impingement) or fluid intrusion through cortical infractions (Fig. 4.64). Patient age also plays a role in the presence of cysts along the humeral tuberosities and may therefore indicate some degenerative change in the bone as part of the aging process.
FIGURE 4.59 Faceting (acetabularization) of the acromion. This remodeling of the acromion (white arrow) is seen in the setting of high-riding humerus related to a large rotator cuff tear. Notice the significant retraction of the supraspinatus tendon (black arrow).
FIGURE 4.60 Deltoid dehiscence with hematoma in a patient who had a large rotator cuff tear and who was also on Coumadin. This coronal T1-weighted image shows the hematoma with areas of high signal methemoglobin occupying the space of the torn deltoid (arrow).
FIGURE 4.61 Cartilage loss on the superior aspect of the humeral head (arrow) seen on a fat-suppressed oblique coronal T2-weighted image in the setting of a large supraspinatus tendon tear.
FIGURE 4.62 Anterior greater tuberosity cyst associated with a supraspinatus tendon partial tear on this fat-suppressed oblique coronal image (arrow).
FIGURE 4.63 Vessels are frequently present in the posterior humeral head (arrow) and are seen on a fat-suppressed T2-weighted oblique coronal image.
Fractures of the greater tuberosity can simulate a rotator cuff tear clinically. Usually seen in the patient younger than 40 years of age (167), the radiograph may be normal with the fracture line and surrounding bone marrow reactive change only seen on the MRI (168). This type of fracture is usually treated conservatively. The adjacent rotator cuff tendons may demonstrate abnormal signal intensity related to contusion and reactive changes (Fig. 4.65). A partial supraspinatus tendon tear frequently accompanies these fractures, but it can be difficult to separate from the reactive cuff contusion. In these cases, it is wise to wait before diagnosing partial tears of the tendons based only on signal intensity. If the fracture fragment is displaced, it is usually pulled posterosuperiorly. Displacement of greater than 5 mm is associated with a rotator cuff tear that may require open reduction and internal fixation. The lesser tuberosity may also avulse in cases of acute trauma with violent hyperextension or external rotation of the adducted arm as well as posterior shoulder dislocation, as mentioned previously and in the chapter on shoulder instability (Fig. 4.55). These subscapularis tendon avulsions are usually seen in younger patients (169).
Statistical Considerations Regarding Magnetic Resonance Imaging of Rotator Cuff Tears
Conventional MRI has been shown to be variably sensitive, specific, and accurate for the diagnosis of full-thickness rotator cuff tears as seen in studies performed during the last 2 decades (18, 41, 134, 170, 171). In a study by Zlatkin et al. (170), which evaluated MR findings in shoulders of 40 patients with surgical and arthrographic correlation, MR was 91% sensitive, 88% specific, and 89% accurate for demonstrating all types of rotator cuff tears. Another study that looked at arthroscopic or surgical correlation in full-thickness cuff tears in 91 patients found that MRI had a sensitivity of 100% and a specificity of 95% (134). Burk et al. (18) reported a similar sensitivity of 92% for MRI and arthrography for the diagnosis of rotator cuff tears. In an investigation by Rafii et al. (77) of 80 patients with shoulder pain and surgical evaluation, 47 of whom had either full- or partial-thickness tears, MRI was 95% and 84% accurate in demonstrating full-thickness and partial-thickness tears, respectively. For full-thickness tears, of which there were 37 in the study, there was a sensitivity of 97% and specificity of 94%. In a different study, MR scans of 87 consecutive patients with arthroscopic correlation showed a sensitivity of 91% and specificity of 95% for full-thickness tears and a sensitivity of 74% and specificity of 87% for partial-thickness tears using combined spin-echo and T2*-weighted gradient echo MRI (172). A study by Quinn et al. (171) evaluated fat-suppressed MRI with arthroscopic correlation in 100 patients. With data combined for complete and partial tears of the rotator cuff, MRI had an accuracy of 93%, a sensitivity of 84%, and a specificity of 97%. A study by Singson et al. (173) shows a 100% sensitivity for full-thickness tears. Reinus et al. (122) have shown that using the fat-saturation technique with conventional MRI improves detection of both full-thickness and partial-thickness tears compared with standard spin-echo imaging techniques. They also found that detection of partial-thickness tears was poor with both techniques. A study by Sonin et al. (174) on 26 patients with surgical correlation showed a sensitivity of 89%, a specificity of 94%, and a diagnostic accuracy of 92% using fast spin-echo T2-weighted sequences.
FIGURE 4.64 Lesser tuberosity cysts are often a sign of subscapularis pathology. In this case, there are multiple cysts in the lesser tuberosity associated with a full-thickness tear of the subscapularis tendon (black arrow) related to subcoracoid impingement on an axial gradient echo image.
FIGURE 4.65 Nondisplaced, radiographically occult greater tuberosity fracture (black arrow). There is some increased signal intensity in the supraspinatus tendon on this fat-suppressed oblique coronal T2-weighted image, which represented reactive change related to the fracture rather than a tear.
MR arthrography is useful for the diagnosis of partial-thickness tears, particularly articular-sided tears, and can distinguish a high-grade partial tear from a full-thickness tear by showing contrast entering the subacromial subdeltoid bursa through the tear in the case of a full-thickness tear (125). In one study, a direct comparison between MRI and MR arthrography found a sensitivity of 90.2% for MRI and 100% for MR arthrography for the detection of full-thickness tears (175). These authors found that MR arthrography allowed for a more accurate assessment of size and morphology of the tear when compared with the surgical gold standard. Another study showed that MR arthrography had an 84% sensitivity and 96% specificity for demonstrating partial articular-sided tears (176).
MR arthrography with the arm in abduction and external rotation can also increase accuracy for detecting and characterizing partial articular-sided tears of the supraspinatus and infraspinatus tendons (127, 177). One study showed that ABER MR arthrographic studies significantly improved detection of articular-sided tears when compared with oblique coronal MR arthrographic views with the arm at the side (127).
Treatment of Partial- and Full-thickness Rotator Cuff Tears
Treatment planning can be influenced by the type of rotator cuff abnormality seen on MRI and other associated abnormalities, including those that are the result of shoulder instability. Decisions should be based on careful evaluation of the MR findings with close clinical correlation, especially because rotator cuff repair surgery usually requires 6 to 9 months of rehabilitation.
Many factors are used to decide whether a tear should be treated conservatively, with primary repair, or with subacromial decompression or distal clavicular resection. Treatment philosophies also vary between institutions. Initial treatment of a symptomatic rotator cuff with tendinosis or a partial tear is usually conservative without surgical intervention. However, at some centers, a partial-thickness tear is explored and débrided or repaired. Partial intrasubstance tears can be difficult, if not impossible, to identify during surgery. Preoperative knowledge of the existence of intrasubstance partial tears gained from an MRI can alter the surgical approach leading to a probe of the undersurface of the rotator cuff in the region of the intrasubstance tear. The surgeon may then enter the tear and débride it, often with successful results.
Distinction between a high-grade partial-thickness tear and a small full-thickness tear may not be necessary, because both are usually treated in a similar fashion (173). A full-thickness tear may be repaired depending on different circumstances, including the patient’s age, level of activity, and the degree of retraction and muscle atrophy. It is possible for an arthroscopist to underdiagnose a full-thickness tear of the cuff if only one side of the cuff is directly visualized (24). If the patient has an underlying lesion related to shoulder instability, which may lead to or exacerbate a rotator cuff tear, the lesions relating to instability can be addressed.
References
1. Roh MS, Wang VM, April EW, et al. Anterior and posterior musculotendinous anatomy of the supraspinatus. J Shoulder Elbow Surg. 2000;9:436–440.
2. Petersilge CA, Witte DH, Sewell BO, et al. Normal regional anatomy of the shoulder. MRI Clin North Am. 1997;5:667–681.
3. Burkhart SS, Esch JC, Jolson RS. The rotator crescent and rotator cable: an anatomic description of the shoulder’s ‘suspension bridge.’ Arthroscopy. 1993;9:611–616.
4. Kask K, Kolts I, Lubienski A, et al. Magnetic resonance imaging and correlative gross anatomy of the ligamentum semicirculare humeri (rotator cable). Clin Anat. 2008;21:420–426.
5. Morag Y, Jacobson JA, Lucas D, et al. US appearance of the rotator cable with histologic correlation: preliminary results. Radiology. 2006;241:485–491.
6. Gleason PD, Beall DP, Sanders TG, et al. The transverse humeral ligament: a separate anatomical structure or a continuation of the osseous attachment of the rotator cuff? Am J Sports Med. 2006;34:72–77.
7. Clark JM, Harryman DT. Tendons, ligaments, and capsule of the rotator cuff. J Bone Joint Surg Am. 1992;74:713–725.
8. Cone RO III, Resnick D, Danzig L. Shoulder impingement syndrome: radiographic evaluation. Radiology. 1984;150:29–33.
9. Kilcoyne RF, Reddy PK, Lyons F, et al. Optimal plain film imaging of the shoulder impingement syndrome. AJR Am J Roentgenol. 1989;153:795–797.
10. Newhouse KE, El-Khoury GY, Nepola JV, et al. The shoulder impingement view: a fluoroscopic technique for the detection of subacromial spurs. AJR Am J Roentgenol. 1988;151:539–541.
11. Petersson CJ, Redlund-Johnell I. The subacromial space in normal shoulder radiographs. Acta Orthop Scand. 1984;55: 57–58.
12. Mink JH, Harris E, Rappaport M. Rotator cuff tears: evaluation using double-contrast shoulder arthrography. Radiology. 1985;157:621–623.
13. Sullivan T. Rotator cuff disease [letter]. AJR Am J Roentgenol. 1995;165:1554–1555.
14. Freiberger R. Best test for detection of rotator-cuff tear (answer to question). AJR Am J Roentgenol. 1995;164:1018–1019.
15. Middleton WD. Sonographic detection and quantification of rotator cuff tears. AJR Am J Roentgenol. 1993;160:109–110.
16. Wiener SN, Seitz WH. Sonography of the shoulder in patients with tears of the rotator cuff. AJR Am J Roentgenol. 1993;160:103–107.
17. Bretzke CA, Crass JR, Craig EV. Ultrasonography of the rotator cuff: normal and pathologic anatomy. Invest Radiol. 1985;20:311–315.
18. Burk DL Jr, Karasick D, Mitchell DG, et al. Rotator cuff tears: prospective comparison of MR imaging with arthrography, sonography, and surgery. AJR Am J Roentgenol. 1989;152:87–92.
19. Soble MG, Kaye AD, Guay RC. Rotator cuff tear: clinical experience with sonographic detection. Radiology. 1989; 173:319–321.
20. Drakeford MK, Quinn MJ, Simpson SL, et al. A comparative study of ultrasonography and arthrography in evaluation of the rotator cuff. Clin Orthop Relat Res. 1990;253:118–122.
21. Mack LA, Matsen FA III. US evaluation of the rotator cuff. Radiology. 1985;157:205–209.
22. Kim HM, Dahiya N, Teefey SA, et al. Sonography of the teres minor: a study of cadavers. AJR Am J Roentgenol. 2008; 190:589–594.
23. van Holsbeeck MT, Kolowich PA, Eyler WR, et al. US depiction of partial-thickness tear of the rotator cuff. Radiology. 1995;197:443–446.
24. Mack LA, Gannon MK, Kilcoyne RF. Sonographic evaluation of the rotator cuff: accuracy in patients without prior surgery. Clin Orthop Relat Res. 1988;234:21–27.
25. Crass JR, Craig EV, Bretzke CA. Ultrasonography of the rotator cuff. Radiographics. 1985;5:941–953.
26. Middleton WD, Reinus WR, Totty WG, et al. Ultrasonographic evaluation of the rotator cuff and biceps tendon. J Bone Joint Surg Am. 1986;68:440–450.
27. Strobel K, Hodler J, Meyer DC, et al. Fatty atrophy of supraspinatus and infraspinatus muscles: accuracy of US. Radiology. 2005;237:584–589.
28. Khoury V, Cardinal E, Brassard P. Atrophy and fatty infiltration of the supraspinatus muscle: sonography versus MRI. AJR Am J Roentgenol. 2008;190:1105–1111.
29. Bureau NJ, Beauchamp M, Cardinal E, et al. Dynamic sonography evaluation of shoulder impingement syndrome. AJR Am J Roentgenol. 2006;187:216–220.
30. Farin PU, Jaroma H, Harju A, et al. Shoulder impingement syndrome: sonographic evaluation. Radiology. 1990;176:845.
31. Patten RM, Mack LA, Wang KY, et al. Nondisplaced fractures of the greater tuberosity of the humerus: sonographic detection. Radiology. 1992;182:201–204.
32. Magee T, Williams D. 3.0-T MRI of the supraspinatus tendon. AJR Am J Roentgenol. 2006;187:881–886.
33. Neer CS. Anterior acromioplasty for the chronic impingement syndrome in the shoulder. J Bone Joint Surg Am. 1972;54:41–50.
34. Codman EA. Rupture of the supraspinatus tendon. Boston Medical and Surgical Journal. 1911;clxiv:708–710.
35. Neer CS. Impingement lesions. Clin Orthop Relat Res. 1983;173:70.
36. Codman EA. The shoulder. In: Rupture of the Supraspinatus Tendon and Other Lesions In or About the Subacromial Bursa. Brooklyn, NY: G. Miller, 1934.
37. Ozaki J, Fujimoto S, Nakagawa Y, et al. Tears of the rotator cuff of the shoulder associated with pathological changes in the acromion. A study in cadavers. J Bone Joint Surg Am. 1988;70:1224–1230.
38. Kieft GJ, Bloem JL, Rozing PM, et al. Rotator cuff impingement syndrome: MR imaging. Radiology. 1988;166:211–214.
39. Seeger LL, Gold RH, Bassett LW, et al. Shoulder impingement syndrome: MR findings in 53 shoulders. AJR Am J Roentgenol. 1988;150:343–347.
40. Chandnani V, Ho C, Gerharter J, et al. MR findings in asymptomatic shoulders: a blind analysis using symptomatic shoulders as controls. Clin Imaging. 1992;16:25–30.
41. Farley TE, Neumann CH, Steinbach LS, et al. Full–thickness tears of the rotator cuff of the shoulder: diagnosis with MR imaging. AJR Am J Roentgenol. 1992;158:347–351.
42. Liou JTS, Wilson AJ, Totty WG, et al. The normal shoulder: common variations that simulate pathologic conditions at MR imaging. Radiology. 1993;186:435–441.
43. Watson M. Rotator cuff function in the impingement syndrome. J Bone Joint Surg Br. 1989;71:361–366.
44. Morrison DS, Bigliani LU. The clinical significance of variations in acromial morphology. Orthop Trans. 1986;11:234.
45. Edelson JG, Taitz C. Anatomy of the coracoacromial arch. Relation to degeneration of the acromion. J Bone Joint Surg Br. 1992;74:589.
46. Gill TJ, McIrvin E, Kocher MS, et al. The relative importance of acromial morphology and age with respect to rotator cuff pathology. J Shoulder Elbow Surg. 2002;11:327–330.
47. Hirano M, Ide J, Takagi K. Acromial shapes and extension of rotator cuff tears: magnetic resonance imaging evaluation. J Shoulder Elbow Surg. 2002;11:576–578.
48. Mudge MK, Wood VE, Frykman GK. Rotator cuff tears associated with os acromiale. J Bone Joint Surg Am. 1984;66:427–429.
49. Kaplan PA, Bryans KC, Davick JP, et al. MR imaging of the normal shoulder: variants and pitfalls. Radiology. 1992; 184:519–524.
50. Bigliani LU, Morrison DS, April EW. The morphology of the acromion and its relationship to rotator cuff tears. Orthop Trans. 1986;10:228.
51. Farley TE, Neumann CH, Steinbach LS, et al. The coracoacromial arch: MR evaluation and correlation with rotator cuff pathology. Skeletal Radiol. 1994;23:641–645.
52. Vanarthos WJ, Monu JU. Type 4 acromion: a new classification. Contemp Orthop. 1995;30:227–229.
53. Zuckerman JD, Kummer FJ, Cuomo F, et al. Interobserver reliability of acromial morphology classification: an anatomic study. J Shoulder Elbow Surg. 1997;6:286–287.
54. Chang EY, Moses DA, Babb JS, et al. Shoulder impingement: objective 3D shape analysis of acromial morphologic features. Radiology. 2006;239:497–505.
55. Mayerhoefer ME, Breitenseher MJ, Roposch A, et al. Comparison of MRI and conventional radiography for assessment of acromial shape. AJR Am J Roentgenol. 2005;184:671–675.
56. Edelson JG. The ‘hooked’ acromion revisited. J Bone Joint Surg Br. 1995;77:284–287.
57. Getz JD, Recht M, Piraino DW, et al. Acromial morphology: relation to sex, age, symmetry, and subacromial enthesophytes. Radiology. 1996;199:737–742.
58. Epstein RE, Schweitzer ME, Frieman BG, et al. Hooked acromion: prevalence on MR images of painful shoulders. Radiology. 1993;187:479–481.
59. Haygood TM, Langlotz CP, Kneeland JB, et al. Categorization of acromial shape: interobserver variability with MR imaging and conventional radiography. AJR Am J Roentgenol. 1994;162:1377–1382.
60. Peh WCG, Farmer THR, Totty WG. Acromial arch shape: assessment with MR imaging. Radiology. 1995;1995:501–505.
61. Aoki M, Ishii S, Usui M. The slope of the acromion and rotator cuff impingement. Proc Am Shoulder Elbow Surg.1986.
62. Dines DM, Warren RF, Inglis AE, et al. The coracoid impingement syndrome. J Bone Joint Surg Br. 1990;72:314–316.
63. Gerber C, Terrier F, Ganz R. The role of the coracoid process in the chronic impingement syndrome. J Bone Joint Surg Br. 1985;67:703.
64. Crues JV, Fareed DO. Magnetic resonance imaging of shoulder impingement. Top Magn Reson Imaging. 1991;3: 39–49.
65. Needell SD, Zlatkin MB, Sher JS, et al. MR imaging of the rotator cuff: peritendinous and bone abnormalities in an asymptomatic population. AJR Am J Roentgenol. 1996; 166:863–867.
66. Liberson F. Os acromiale: a contested anomaly. J Bone Joint Surg. 1937;19:683–689.
67. Norris TR, Fischer J, Bigliani LU, et al. The unfused acromial epiphysis and its relationship to impingement syndrome. Orthop Trans. 1983;7:505–506.
68. Edelson JG, Zuckerman J, Hershkovitz I. Os acromiale: anatomy and surgical implications. J Bone Joint Surg Br. 1993;74:551–555.
69. Andrews JR, Byrd TJW, Kupfferman SP, et al. The profile view of the acromion. Clin Orthop Relat Res. 1991;263:1991.
70. Hutchinson MR, Veenstra MA. Arthroscopic decompression of shoulder impingement secondary to os acromiale. Arthroscopy. 1993;9:28–32.
71. Gold RH, Seeger LL, Yao L. Imaging shoulder impingement. Skeletal Radiol. 1993;22:555–561.
72. Ouellette H, Thomas BJ, Kassarjian A, et al. Re-examining the association of os acromiale with supraspinatus and infraspinatus tears. Skeletal Radiol. 2007;36:835–839.
73. Park JG, Lee JK, Phelps CT. Os acromiale associated with rotator cuff impingement: MR imaging of the shoulder. Radiology. 1994;193:255–257.
74. McClure JG, Raney RB. Anomalies of the scapula. Clin Orthop Relat Res. 1975;110:22–31.
75. Boutin RD, Spitz DJ, Newman JS, et al. Complications in Paget disease at MR imaging. Radiology. 1998;209:641–651.
76. Kjellin I, Ho CP, Cervilla V, et al. Alterations in the supraspinatus tendon at MR imaging: correlation with histopathologic findings in cadavers. Radiology. 1991;181:837–841.
77. Rafii M, Firooznia H, Sherman O. Rotator cuff lesions: signal patterns at MR imaging. Radiology. 1990;177:817–823.
78. Robertson PL, Schweitzer ME, Mitchell DG, et al. Rotator cuff disorders: interobserver and intraobserver variation in diagnosis with MR imaging. Radiology. 1995;1995:831–835.
79. Burns WC, Whipple TL. Anatomic relationships in the shoulder impingement syndrome. Clin Orthop Relat Res. 1993;294:96–102.
80. Sarkar K, Taine W, Uhthoff HK. The ultrastructure of the coracoacromial ligament in patients with chronic impingement syndrome. Clin Orthop Relat Res. 1990;254:49–54.
81. Gallino M, Battiston B, Annartone G, et al. Coracoacromial ligament: a comparative arthroscopic and anatomic study. Arthroscopy. 1995;11:564–567.
82. Morimoto K, Mori E, Nakagawa Y. Calcification of the coracoacromial ligament. A case report of the shoulder impingement syndrome. Am J Sports Med. 1988;16:80.
83. Krief OP, Huguet D. Shoulder pain and disability: comparison with MR findings. AJR Am J Roentgenol. 2006;186:1234–1239.
84. Major NM. MR imaging after therapeutic injection of the subacromial bursa. Skeletal Radiol. 1999;28:628–631.
85. Bergman AG, Fredericson M. Shoulder MRI after impingement test injection. Skeletal Radiol. 1998;27:365–368.
86. Wright RW, Fritts HM, Tierney GS, et al. MR imaging of the shoulder after an impingement test: how long to wait. AJR Am J Roentgenol. 1998;171:769–773.
87. Borick JM, Kurzweil PR. Magnetic resonance imaging appearance of the shoulder after subacromial injection with corticosteroids can mimic a rotator cuff tear. Arthroscopy. 2008;24:846–849.
88. Gumina S, Postacchini F, Orsina L, et al. The morphometry of the coracoid process—its aetiologic role in subcoracoid impingement syndrome. Int Orthop. 1999;23:198–201.
89. Paulson MM, Watnik NF, Dines DM. Coracoid impingement syndrome, rotator interval reconstruction, and biceps tenodesis in the overhead athlete. Orthop Clin North Am. 2001;32:485–493, ix.
90. Stallenberg B, Destate N, Feipel V, et al. Involvement of the anterior portion of the subacromial–subdeltoid bursa in the painful shoulder. AJR Am J Roentgenol. 2006;187:894–900.
91. Gerber C, Terrier F, Zehnder R, et al. The subcoracoid space. An anatomic study. Clin Orthop Relat Res. 1987;215:132–138.
92. Giaroli EL, Major NM, Lemley DE, et al. Coracohumeral interval imaging in subcoracoid impingement syndrome on MRI. AJR Am J Roentgenol. 2006;186:242–246.
93. MacMahon PJ, Taylor DH, Duke D, et al. Contribution of full-thickness supraspinatus tendon tears to acquired subcoracoid impingement. Clin Radiol. 2007;62:556–563.
94. Dillman CJ, Fleisig GS, Andrews JR. Biomechanics of pitching with emphasis upon shoulder kinematics. J Orthop Sports Phys Ther. 1993;18:402–408.
95. Jobe CM. Posterior superior glenoid impingement: expanded spectrum. Arthroscopy. 1995;11:530–536.
96. Warner JJP, Micheli LJ, Arsianian L, et al. Patterns of flexibility, laxity, and strength in normal shoulders and shoulders with instability and impingement. Am J Sports Med. 1990;18:366.
97. Neumann CH, Holt RG, Steinbach LS, et al. MR imaging of the shoulder: appearance of the supraspinatus tendon in asymptomatic volunteers. AJR Am J Roentgenol. 1992; 158:1281–1287.
98. Mirowitz SA. Normal rotator cuff: MR imaging with conventional and fat-suppression techniques. Radiology. 1991;180: 735–740.
99. Vahlensieck M, Pollack MPL, Grampp S, et al. Two segments of the supraspinatus muscle: cause of high signal intensity at MR imaging. Radiology. 1993;186:449–454.
100. Erickson SJ, Cox IH, Hyde JS, et al. Effect of tendon orientation on MR imaging signal intensity: a manifestation of the ‘magic angle’ phenomenon. Radiology. 1991;181:389–392.
101. Erickson SJ, Prost RW, Timins ME. The ‘magic angle’ effect: background physics and clinical relevance. Radiology. 1993;188:23–25.
102. Timins ME, Erickson SJ, Estkowski LD, et al. Increased signal in the normal supraspinatus tendon on MR imaging: diagnostic pitfall caused by the magic–angle effect. AJR Am J Roentgenol. 1995;164:109–114.
103. Davis SJ, Teresi LM, Bradley WG, et al. Effect of arm rotation on MR imaging of the rotator cuff. Radiology. 1991;181:265–268.
104. Tsai JC, Zlatkin MB. Magnetic resoance imaging of the shoulder. Radiol Clin North Am. 1990;28:279–291.
105. Zlatkin MB, Dalinka MK, Kressel HY. Magnetic resonance imaging of the shoulder. Magn Reson Q. 1989;5:3–22.
106. Sher JS, Uribe JW, Posada A, et al. Abnormal findings on magnetic resonance images of asymptomatic shoulders. J Bone Joint Surg Am. 1995;77:10–15.
107. Milgrom C, Schaffler M, Gilbert S, et al. Rotator-cuff changes in asymptomatic adults. The effect of age, hand dominance and gender. J Bone Joint Surg Br. 1995;77:296–298.
108. Miniaci A, Mascia AT, Salonen DC, et al. Magnetic resonance imaging of the shoulder in asymptomatic professional baseball pitchers. Am J Sports Med. 2002;30:66–73.
109. Yamaguchi K, Sher JS, Andersen WK, et al. Glenohumeral motion in patients with rotator cuff tears: a comparison of asymptomatic and symptomatic shoulders. J Shoulder Elbow Surg. 2000;9:6–11.
110. Ellman H. Diagnosis and treatment of incomplete rotator cuff tears. Clin Orthop Relat Res. 1990;254:64–74.
111. Tamai K, Ogawa K. Intratendinous tears of the supraspinatus tendon exhibiting winging of the scapula. Clin Orthop Relat Res. 1985;194:159.
112. Reilly P, Amis AA, Wallace AL, et al. Supraspinatus tears: propagation and strain alteration. J Shoulder Elbow Surg. 2003;12:134–138.
113. Snyder S, ed. Rotator Cuff: Introduction, Evaluation, and Imaging. Philadelphia, Pa: Lippincott Williams & Wilkins; 2003.
114. Ruotolo C, Fow JE, Nottage WM. The supraspinatus footprint: an anatomic study of the supraspinatus insertion. Arthroscopy. 2004;20:246–249.
115. Vinson EN, Helms CA, Higgins LD. Rim-rent tear of the rotator cuff: a common and easily overlooked partial tear. AJR Am J Roentgenol. 2007;189:943–946.
116. Millstein ES, Snyder SJ. Arthroscopic management of partial, full-thickness, and complex rotator cuff tears: indications, techniques, and complications. Arthroscopy. 2003;19(suppl 1):189–199.
117. Lyons TR, Savoie FH 3rd, Field LD. Arthroscopic repair of partial-thickness tears of the rotator cuff. Arthroscopy. 2001;17:219–223.
118. Waibl B, Buess E. Partial-thickness articular surface supraspinatus tears: a new transtendon suture technique. Arthroscopy. 2005;21:376–381.
119. Conway JE. Arthroscopic repair of partial-thickness rotator cuff tears and SLAP lesions in professional baseball players. Orthop Clin North Am. 2001;32:443–456.
120. Walz DM, Miller TT, Chen S, et al. MR imaging of delamination tears of the rotator cuff tendons. Skeletal Radiol. 2007;36:411–416.
121. Sonnabend DH, Yu Y, Howlett CR, et al. Laminated tears of the human rotator cuff: a histologic and immunochemical study. J Shoulder Elbow Surg. 2001;10:109–115.
122. Reinus WR, Shady KL, Mirowitz SA, et al. MR diagnosis of rotator cuff tears of the shoulder: value of using T2-weighted fat-saturated images. AJR Am J Roentgenol. 1995;164:1451–1455.
123. Hodler J, Kursunoglu-Brahme S, Snyder SJ, et al. Rotator cuff disease: assessment with MR arthrography versus standard MR imaging in 36 patients with arthroscopic confirmation. Radiology. 1992;182:431–436.
124. Flannigan B, Kursunoglu-Brahme S, Snyder S, et al. MR arthrography of the shoulder: comparison with conventional MR imaging. AJR Am J Roentgenol. 1990;155:829–832.
125. Palmer WE, Brown JH, Rosenthal DI. Rotator cuff: evaluation with fat-suppressed MR arthrography. Radiology. 1993; 1993:683–687.
126. Tirman PFJ, Bost F, Garvin GJ, et al. Posterosuperior glenoid impingement of the shoulder: findings at MR imaging and MR arthrography with arthroscopic correlation. Radiology. 1994;193:431–436.
127. Lee SY, Lee JK. Horizontal component of partial-thickness tears of rotator cuff: imaging characteristics and comparison of ABER view with oblique coronal view at MR arthrography initial results. Radiology. 2002;224:470–476.
128. Walch G, Boileau P, Noel E, et al. Impingement of the deep surface of the supraspinatus tendon on the posterosuperior glenoid rim: an arthroscopic study. Shoulder Elbow Surg. 1992;1:238–245.
129. Warner JJ, Higgins L, Parsons IM, et al. Diagnosis and treatment of anterosuperior rotator cuff tears. J Shoulder Elbow Surg. 2001;10:37–46.
130. Snyder S, ed. Arthroscopic Classification of Rotator Cuff Lesions and Surgical Decision Making. Philadelphia, Pa: Lippincott Williams & Wilkins; 2003.
131. Lo IK, Burkhart SS. Arthroscopic repair of massive, contracted, immobile rotator cuff tears using single and double interval slides: technique and preliminary results. Arthroscopy. 2004;20:22–33.
132. Burkhart SS, Danaceau SM, Pearce CE Jr. Arthroscopic rotator cuff repair: analysis of results by tear size and by repair technique—margin convergence versus direct tendon-to-bone repair. Arthroscopy. 2001;17:905–912.
133. DeOrio JK, Cofield RH. Results of a second attempt at surgical repair of a failed initial rotator–cuff repair. J Bone Joint Surg Am. 1984;66:563–567.
134. Ianotti JP, Zlatkin MB, Esterhai JL, et al. Magnetic resonance imaging of the shoulder. J Bone Joint Surg Am. 1991;73:17–29.
135. Zanetti M, Gerber C, Hodler J. Quantitative assessment of the muscles of the rotator cuff with magnetic resonance imaging. Invest Radiol. 1998;33:163–170.
136. Thomazeau H, Rolland Y, Lucas C, et al. Atrophy of the supraspinatus belly. Assessment by MRI in 55 patients with rotator cuff pathology. Acta Orthop Scand. 1996;67:264–268.
137. Maughan RJ, Watson JS, Weir J. Strength and cross-sectional area of human skeletal muscle. J Physiol. 1983;338:37–49.
138. Goutallier D, Postel JM, Bernageau J, et al. Fatty muscle degeneration in cuff ruptures. Clin Orthop Relat Res. 1994;304:78–83.
139. Goutallier D, Postel JM, Gleyze P, et al. Influence of cuff muscle fatty degeneration on anatomic and functional outcomes after simple suture of full-thickness tears. J Shoulder Elbow Surg. 2003;12:550–554.
140. Goutallier D, Postel JM, Lavau L, et al. Impact of fatty degeneration of the supraspinatus and infraspinatus muscles on the prognosis of surgical repair of the rotator cuff [in French]. Rev Chir Orthop Reparatrice Appar Mot. 1999;85:668–676.
141. Mitchell MJ, Causey G, Berthoty DP, et al. Peribursal fat plane of the shoulder: anatomic study and clinical experience. Radiology. 1988;168:699–704.
142. Ferrari JD, Ferrari DA, Coumas J, et al. Posterior ossification of the shoulder: the Bennett lesion. Am J Sports Med. 1994;22:171–176.
143. Bryan W, Wild J. Isolated infraspinatus atrophy. Am J Sports Med. 1989;17:130–133.
144. Lunn JV, Castellanos-Rosas J, Tavernier T, et al. A novel lesion of the infraspinatus characterized by musculotendinous disruption, edema, and late fatty infiltration. J Shoulder Elbow Surg. 2008;17:546–553.
145. Symeonides PP. The significance of the subscapularis muscle in the pathogenesis of recurrent anterior dislocation of the shoulder. J Bone Joint Surg Br. 1972;54:476–483.
146. Neviaser RJ, Neviaser TJ, Neviaser JS. Concurrent rupture of the rotator cuff and anterior dislocation of the shoulder in the older patient. J Bone Joint Surg Am. 1988;70:1308–1311.
147. Neviaser RJ, Neviaser TH, Neviaser JS. Anterior dislocation of the shoulder and rotator cuff rupture. Clin Orth Relat Res. 1993;291:103–106.
148. Sakurai G, Ozaki J, Tomita Y, et al. Incomplete tears of the subscapularis tendon associated with tears of the supraspinatus tendon: cadaveric and clinical studies. J Shoulder Elbow Surg. 1998;7:510–515.
149. Studler U, Pfirrmann CW, Jost B, et al. Abnormalities of the lesser tuberosity on radiography and MRI: association with subscapularis tendon lesions. AJR Am J Roentgenol. 2008; 191:100–106.
150. Bergin D, Parker L, Zoga A, et al. Abnormalities on MRI of the subscapularis tendon in the presence of a full-thickness supraspinatus tendon tear. AJR Am J Roentgenol. 2006;186:454–459.
151. Gerber C, Krushell RJ. Isolated rupture of the tendon of the subscapularis muscle. J Bone Joint Surg Br. 1991;73:389–394.
152. Chan TW, Dalinka MK, Kneeland BJ, et al. Biceps tendon dislocation: evaluation with MR imaging. Radiology. 1991;179:649–652.
153. Cervilla V, Schweitzer ME, Ho C, et al. Medial dislocation of the biceps brachii tendon: appearance at MR imaging. Radiology.1991;180:523–526.
154. Sanders TG, Tirman PF, Feller JF, et al. Association of intramuscular cysts of the rotator cuff with tears of the rotator cuff: magnetic resonance imaging findings and clinical significance. Arthroscopy. 2000;16:230–235.
155. Kassarjian A, Torriani M, Ouellette H, et al. Intramuscular rotator cuff cysts: association with tendon tears on MRI and arthroscopy. AJR Am J Roentgenol. 2005;185:160–165.
156. Craig EV. The acromioclavicular joint cyst: an unusual presentation of a rotator cuff tear. Clin Orthop Relat Res. 1986;202:189.
157. Postacchini F, Perugia D, Gumina S. Acromioclavicular joint cyst associated with rotator cuff tear. Clin Orthop Relat Res. 1993;294:111–113.
158. Tshering Vogel DW, Steinbach LS, Hertel R, et al. Acromioclavicular joint cyst: nine cases of a pseudotumor of the shoulder. Skeletal Radiol. 2005;34:260–265.
159. Groh GI, Badwey TM, Rockwood CA. Treatment of cysts of the acromioclavicular joint with shoulder hemiarthroplasty. J Bone Joint Surg Am. 1993;75:1790–1794.
160. Saupe N, Pfirrmann CW, Schmid MR, et al. Association between rotator cuff abnormalities and reduced acromiohumeral distance. AJR Am J Roentgenol. 2006;187:376–382.
161. Bianchi S, Martinoli C, Abdelwahab IF. Imaging findings of spontaneous detachment of the deltoid muscle as a complication of massive rotator cuff tear. Skeletal Radiol. 2006;35:410–415.
162. Ilaslan H, Iannotti JP, Recht MP. Deltoid muscle and tendon tears in patients with chronic rotator cuff tears. Skeletal Radiol. 2007;36:503–507.
163. Feeney MS, O’Dowd J, Kay EW, et al. Glenohumeral articular cartilage changes in rotator cuff disease. J Shoulder Elbow Surg. 2003;12:20–23.
164. Guntern DV, Pfirrmann CW, Schmid MR, et al. Articular cartilage lesions of the glenohumeral joint: diagnostic effectiveness of MR arthrography and prevalence in patients with subacromial impingement syndrome. Radiology. 2003;226:165–170.
165. Beall DP, Williamson EE, Ly JQ, et al. Association of biceps tendon tears with rotator cuff abnormalities: degree of correlation with tears of the anterior and superior portions of the rotator cuff. AJR Am J Roentgenol. 2003;180:633–639.
166. Fritz LB, Ouellette HA, O’Hanley TA, et al. Cystic changes at supraspinatus and infraspinatus tendon insertion sites: association with age and rotator cuff disorders in 238 patients. Radiology. 2007;244:239–248.
167. Zanetti M, Weishaupt D, Jost B, et al. MR imaging for traumatic tears of the rotator cuff: high prevalence of greater tuberosity fractures and subscapularis tendon tears. AJR Am J Roentgenol. 1999;172:463–467.
168. Mason BJ, Kier R, Bindleglass DF. Occult fractures of the greater tuberosity of the humerus: radiographic and MR imaging findings. AJR Am J Roentgenol. 1999;172:469–473.
169. Scheibel M, Martinek V, Imhoff AB. Arthroscopic reconstruction of an isolated avulsion fracture of the lesser tuberosity. Arthroscopy. 2005;21:487–494.
170. Zlatkin MB, Iannotti JP, Roberts MC, et al. Rotator cuff tears: diagnostic performance of MR imaging. Radiology. 1989;172:223–229.
171. Quinn SF, Sheley RC, Demlow TA, et al. Rotator cuff tendon tears: evaluation with fat-suppressed MR imaging with arthroscopic correlation in 100 patients. Radiology. 1995;195: 497–501.
172. Tuite MJ, Yandow DR, DeSmet AA, et al. Diagnosis of partial and complete rotator cuff tears using combined gradient echo and spin echo imaging. Skeletal Radiol. 1994;23:541–546.
173. Singson RD, Hoang T, Dan S, et al. MR evaluation of rotator cuff pathology using T2-weighted fast spin-echo technique with and without fat suppression. AJR Am J Roentgenol. 1996;166:1061–1065.
174. Sonin AH, Peduto AJ, Fitzgerald SW, et al. MR imaging of the rotator cuff mechanism: comparison of spin-echo and turbo spin-echo sequences. AJR Am J Roentgenol. 1996;167:333–338.
175. Toyoda H, Ito Y, Tomo H, et al. Evaluation of rotator cuff tears with magnetic resonance arthrography. Clin Orthop Relat Res. 2005;439:109–115.
176. Meister K, Thesing J, Montgomery WJ, et al. MR arthrography of partial thickness tears of the undersurface of the rotator cuff: an arthroscopic correlation. Skeletal Radiol. 2004;33:136–141.
177. Tirman PFJ, Bost FW, Steinbach LS, et al. MR arthrographic depiction of tears of the rotator cuff: benefit of abduction and external rotation of the arm. Radiology. 1994;192:851–856.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree