FIGURE 3.8 Total active forward elevation is measured as maximal elevation performed with the humerus in the scapular plane located between the sagittal and coronal planes.
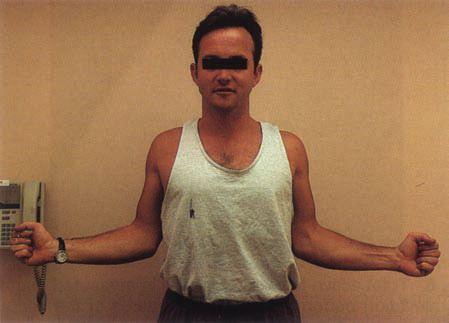
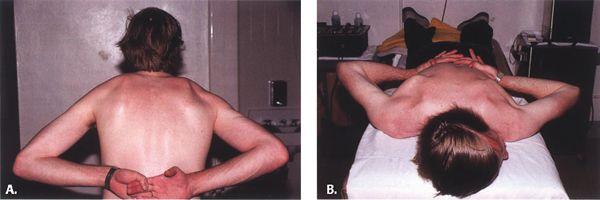
Forward elevation is an examination of the patient’s ability to raise his or her arm maximally in the plane of scapular motion, located between the sagittal and coronal planes (Fig. 3.8). Because two thirds of the overall shoulder range of motion occurs at the glenohumeral articulation and one third occurs at the scapulothoracic articulation (20), this examination evaluates the patient’s true functional range of motion in overhead reaching ability. Limitations in glenohumeral range of motion can be determined by careful examination of the scapulothoracic rhythm and range. If limitations or an abnormal motion exists, the patient should be observed both anteriorly and posteriorly to determine which articulation is abnormal. A common finding in patients with a weak or painful shoulder is “hiking,” which is a pathologic shoulder rhythm in which elevation or rotation of the scapula precedes glenohumeral abduction in an effort to maximize total elevation of the extremity (Fig. 3.9).
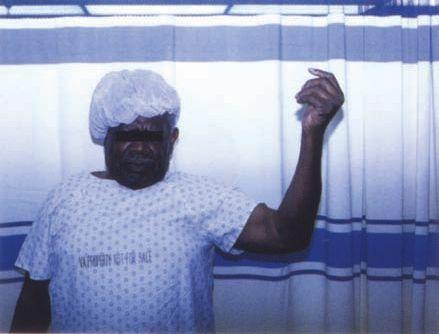
FIGURE 3.9 This patient demonstrates the classic “hiking” of the shoulder seen in patients with massive rotator cuff tears. In an effort to increase total shoulder elevation, the patient elevates the scapula using the periscapular muscles.
FIGURE 3.10 Active external rotation with the elbow flexed 90 degrees and the patient standing.
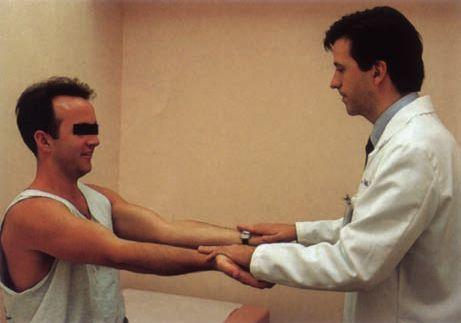
External rotation is performed with the patient’s elbow flexed at 90 degrees and the elbow located at the patient’s side. The patient then rotates his or her forearm externally while maintaining a vertical humerus and a flexed elbow (Fig. 3.10). Neutral rotation is defined when the forearm is directly anterior, that is, in the sagittal plane, and 90 degrees external rotation is noted when the forearm is rotated directly laterally in the coronal plane.
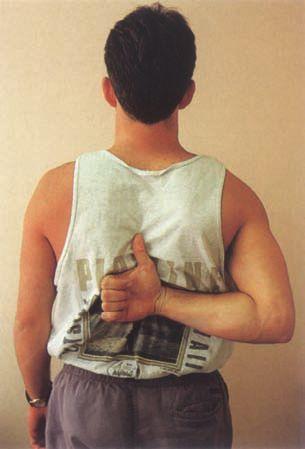
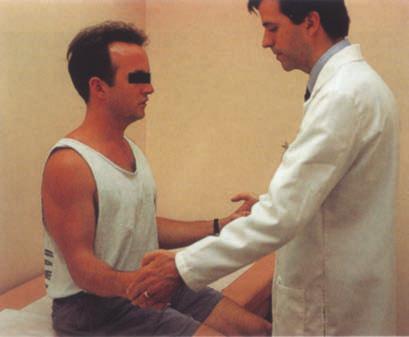
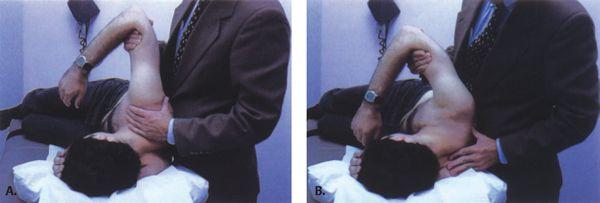
Internal rotation is evaluated by instructing patients to place their hand behind their back and reach their thumb as high as possible. This examination is not performed simultaneously but rather sequentially to minimize interference between the two extremities. The maximum height that the patient is able to reach the thumb is documented by the anatomic level, for instance, the iliac crest, lumbar spine, or thoracolumbar junction (Fig. 3.11).
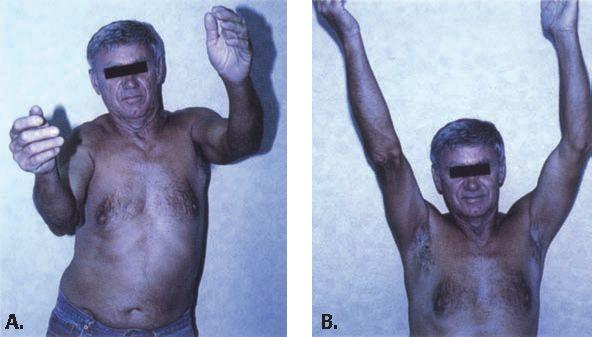
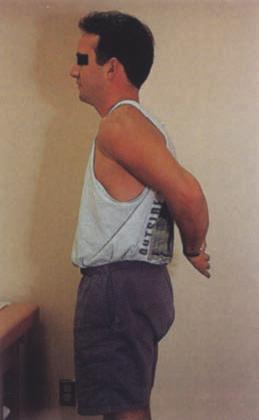
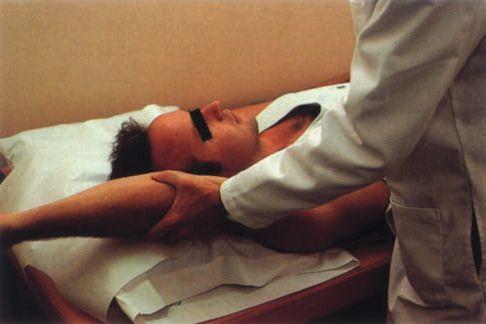
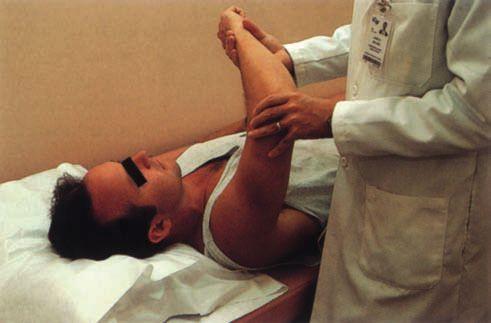
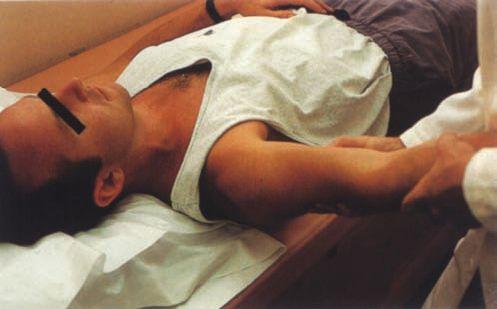
Measurements of passive range of motion are performed when limitations in active motion are noted. An increase seen in passive range of motion over that noted in active range of motion suggests a functional cause for motion loss. The most common diagnosis resulting in this discrepancy is large and massive rotator cuff tears, although neurologic causes may result in a similar clinical picture (Fig. 3.12). Passive range of motion may be performed with the patient supine to increase patient comfort.
FIGURE 3.11 Internal rotation is documented as the maximum cephalad position the patient can reach with the extended thumb.
FIGURE 3.12 Passive motion in all planes is measured in patients who do not have full active range of motion. A: In this patient, active forward elevation is limited. B: The examiner is able to passively position the arm in full forward elevation. Also note that the patient is able to maintain the arm in the position that it was placed.
Determination of the subtle loss in range of motion is essential in the throwing athlete because contractures frequently limit internal rotation and horizontal adduction in this patient population. These alterations in the normal mechanics of the shoulder, if not addressed, may result in increased stresses on the anterior capsule and secondarily on the elbow. Subtle restrictions of passive motion again can be detected by measuring internal and external rotation of the shoulder with the humerus abducted 90 degrees and the scapula stabilized by the examiner’s hand (Fig. 3.13). Alternatively, internal rotation loss can be quickly detected (but not quantitatively measured) by observing scapular winging on standing or prone patients with their hands clasped behind their back (Fig. 3.14). An external rotation contracture (limited internal rotation) is frequently noted (Fig. 3.15).
Strength Testing
Strength testing is an integral part of the shoulder examination. It exposes weakness that may be primarily related to mechanical damage to the soft tissues, to neurologic causes, or secondarily to pain inhibition. It is thus imperative that the strength examination evaluate all of the major structures of the shoulder to delineate the structures that are injured or dysfunctional. The supraspinatus strength is tested by resisted forward elevation with the arm maximally internally rotated and shoulder abducted 60 degrees (Fig. 3.16). Resisted external rotation in neutral abduction tests the infraspinatus–teres minor complex (Fig. 3.17). Strength of the subscapularis is tested with resisted internal rotation and the lift-off test (Fig. 3.18), which is described subsequently.
Neurologic and Vascular Examination
In patients with subtle shoulder pain or weakness, a thorough neurologic examination must be performed. This includes an examination of sensory, motor, and reflex functions of the upper extremity because cervical spine conditions may mimic shoulder conditions. Careful attention should be paid to the evaluation of the external rotators of the shoulder because suprascapular nerve entrapment at the level of the suprascapular notch or the spinoglenoid notch may lead to paralysis of the supraspinatus and infraspinatus or the infraspinatus alone, respectively (21). This denervation results in shoulder pain as well as weakness in shoulder elevation and external rotation. Frequently, these patients have clinical findings that are consistent with rotator cuff disease.
FIGURE 3.13 Passive external rotation with the shoulder abducted 90 degrees is a sensitive means of determining motion abnormalities. A: The unaffected shoulder in a patient with adhesive capsulitis reveals normal external rotation. B: The affected shoulder reveals significant limitation in external rotation.
FIGURE 3.14 Passive internal rotation with the shoulder abducted 90 degrees and the scapula stabilized reveals loss of motion. This professional baseball player exhibits a classic external rotation contracture.
Finally, in patients with shoulder pain of unclear origin, a vascular examination should be performed to evaluate the patient for thoracic outlet syndrome (TOS) or axillary venous occlusion. The Adson’s test, which is used to determine TOS, is performed by palpating the patient’s radial pulse. The patient’s arm is then placed in abduction and external rotation while the pulse is maintained. Patients are then instructed to rotate their head to the involved shoulder. A diminished pulse confirms TOS. In overhead athletes, axillary venous occlusion can occur through repetitive impingement with abduction and is manifested by pain and venous engorgement of the upper extremity.
Specific Examinations
There are many afflictions of the shoulder that may be adequately evaluated using a thorough general examination complemented by an appropriate radiographic examination. These afflictions include most fractures and acute dislocations, glenohumeral and acromioclavicular arthritis, and calcific tendinitis. The clinical evaluation of soft tissue injuries of the shoulder, which are some of the more common causes of a symptomatic shoulder, may be much more elusive. These injuries include impingement syndrome and rotator cuff disease, glenohumeral instability, and superior labral lesions. In the evaluation of these entities, many special signs and tests have been described to aid in the evaluation of these processes. MRI is also an important adjunct because of its ability to accurately evaluate soft tissue structures of the shoulder. The following is a discussion of the evaluation of those entities in which MRI is most effectively used to improve diagnostic accuracy.
Examination for Impingement, Rotator Cuff Disease, and Biceps Tendinitis
A thorough history and physical examination of the shoulder by an experienced examiner results in an examination with 84% to 90% sensitivity and 75% to 95% specificity when evaluating for rotator cuff tears (22, 23). The history generally reveals chronic symptoms of pain, which may be aggravated with overhead activity of the shoulder. An acute incident such as a fall may worsen an already painful shoulder and may result in greater weakness. This may represent an acute additional tear in an already torn rotator cuff and can greatly influence the goals and success of surgical intervention. The location of pain is nonspecific but generally is located over the lateral aspect of the deltoid. Classically, patients report night pain that awakens them from sleep.
Physical Examination
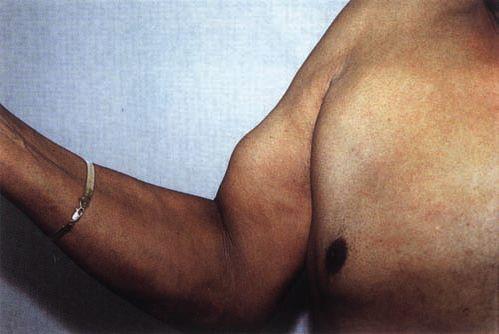
The visual examination of the shoulder with rotator cuff disease may reveal previous incisions or other conditions related to previous surgery (Fig. 3.19). Supraspinatus or infraspinatus fossa atrophy suggests disuse of the rotator cuff resulting from longstanding pain with or without tearing of cuff tissue. Inspection of the distal arm may reveal a distally migrated bulk of the biceps muscle caused by rupture of the long head of the biceps tendon (Fig. 3.20).
FIGURE 3.15 External rotation contracture may be demonstrated by two methods. A: Abduction rotation testing. B: Scapular winging in the prone patient with the hands placed on the lumbar spine.
FIGURE 3.16 Supraspinatus strength is tested with the patient’s arm in a position of 60 degrees of forward elevation with the shoulder internally rotated and the elbow extended. A downward force applied by the examiner is resisted by the patient.
Palpation of the rotator cuff may reveal tenderness of the cuff in various positions, suggesting an impingement process. The palpation examination is facilitated by extending the shoulder. With subsequent external rotation, the anterior portion of the supraspinatus is palpated. With progressive internal rotation, the more posterior aspect of the rotator cuff is exposed. Crepitus is common in patients with rotator cuff disease. It is tested by bringing the arm into approximately 60 degrees of forward elevation and then rotating the arm internally and externally. The roughened cuff and bursa rotating under the acromion and coracoacromial ligament create the crepitus, which is palpated by the examiner’s fingertips.
Range of motion of the shoulder with rotator cuff deficiency is frequently not affected. A small percentage of patients with massive rotator cuff tears may be able to fully elevate the arm. These patients may have proximal migration of the humeral head such that it contacts the undersurface of the acromion. This contact point functions as a fulcrum, allowing for near normal elevation of the shoulder with deltoid contraction despite the absence of the rotator cuff. For this reason, examination of the rhythm of shoulder motion is essential in the diagnosis of rotator cuff disease. An often subtle finding on range-of-motion examination in patients with rotator cuff disease is the characteristic hiking of the shoulder or elevation of the scapula with the trapezius muscle. An even more subtle observation, which is best appreciated when viewed posteriorly, is the abnormal rhythm accompanying excessive scapular rotation in abduction or flexion.
FIGURE 3.17 External rotation is tested with the patient’s arm at the side and the elbow flexed 90 degrees. The patient resists a medially directed force applied by the examiner to the dorsum of the patient’s hand.
FIGURE 3.18 The lift-off test is performed to evaluate subscapularis strength. The patient is asked to actively lift the hand off of the lumbar region.
FIGURE 3.19 Previous incisions may indicate prior related surgical procedures.
FIGURE 3.20 Ruptured long head of the biceps tendon. Because of the tendon rupture, the muscle belly has retracted distally, resulting in the characteristic “Popeye” appearance.
In patients who do exhibit limits in range of motion, an examination of passive motion is carried out. This important aspect of the examination helps distinguish impingement syndrome and rotator cuff disease from other conditions, most notably adhesive capsulitis. Whereas in adhesive capsulitis, there are similar limits in both active and passive range of motion, rotator cuff disease generally does not limit passive range of motion unless secondary adhesive capsulitis has developed. Additionally, those patients with massive tears who are unable to actively elevate the arm above 90 degrees may be able to actively maintain the arm in full abduction when placed in this position by the examiner.
While testing range of motion, the examiner should look for a painful arc of motion. The painful arc is a non-specific examination, but it is suggestive of rotator cuff disease (24). The painful arc usually occurs when the patient actively elevates the arm between approximately 60 and 100 degrees (Fig. 3.21). This motion arc is painful because of the passing of the greater tuberosity under the anterolateral edge of the acromion, causing increased discomfort in an irritated rotator cuff or biceps tendon. A similar painful arc may also be seen when performing the passive supine abduction rotation test. Patients may experience painful symptoms when the arm is taken from neutral to 60 degrees of external rotation and from neutral rotation into approximately 45 degrees of internal rotation, which causes abrasion of the inflamed rotator cuff or biceps tendon against the undersurface of the acromion or coracoacromial ligament.
After range of motion has been assessed, strength testing of the supraspinatus, external (infraspinatus/teres minor), and internal (subscapularis) rotators is performed to further highlight suspected weakness. Supraspinatus function is evaluated by testing the patient’s ability to resist a downward force applied to the humerus with the elbow extended and the arm in a position of internal rotation and 45 degrees of forward flexion. Pain, weakness, or both symptoms may result in the patient’s inability to resist.
If the patient is sufficiently weak or painful, he or she may exhibit a drop-arm test (25). The drop-arm test is positive when the patient is unable to slowly lower the maximally elevated arm to the side because of pain or weakness. Instead, the patient drops the affected extremity to his or her side.
Strength of the infraspinatus and teres minor is evaluated by assessing the patient’s ability to resist inwardly applied force to the forearm with the shoulder in a position of neutral abduction with the elbow flexed 90 degrees. Weakness in external rotation suggests a large or massive cuff tear, although it may also represent palsy of the infraspinatus branch of the suprascapular nerve (Fig. 3.22). A confirmatory indicator of a large or massive rotator cuff tear is the dropping test (24). In this test, the examiner holds the patient’s involved extremity in external rotation. The patient is asked to maintain the arm in the externally rotated position. Because the infraspinatus and teres minor are the primary external rotators of the shoulder, a patient’s inability to maintain external rotation suggests a massive tear involving the infraspinatus and often the teres minor.
FIGURE 3.21 The painful arc is noted when the patient elevates the shoulder through an arc between 60 and 100 degrees. This patient had impingement without a rotator cuff tear and improved with subacromial decompression.
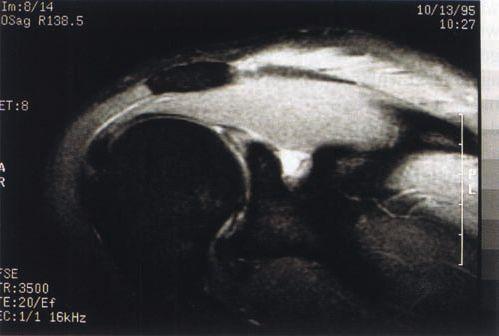
FIGURE 3.22 An example of a ganglion cyst in the spinoglenoid notch impinging on the infraspinatus branch of the suprascapular nerve with electromyographically documented neuropraxia of the infraspinatus.
FIGURE 3.23 Speed’s test assessing tendonitis of the long head of the bicepsis demonstrated.
FIGURE 3.24 Primary or impingement I (Neer’s sign) is noted as pain with maximal passive elevation of the shoulder.
The internal rotation strength of the shoulder is evaluated by the lift-off test (26). Because internal rotation of the shoulder in neutral rotation is performed by not only the subscapularis, but also the pectoralis major, teres major, and latissimus dorsi, it is necessary to isolate the subscapularis by placing these other external rotators at a mechanical disadvantage. This is achieved by internally rotating the shoulder and positioning the forearm behind the patient’s back. The patient is then asked to lift his or her hand off of the lumbar region of the spine, an action that requires further active internal rotation of the shoulder. Alternatively, the physician may hold the hand away from the patient’s lumbar spine and then ask the patient to maintain the position when the hand is released. An inability to do so suggests dysfunction of the subscapularis.
Pathology of the long head of the biceps tendon often accompanies rotator cuff conditions and occasionally can be seen in isolation (8). Because of this, it is imperative that the biceps tendon be examined in isolation. Speed’s test is the most useful of the many tests that evaluate the biceps tendon (19). In Speed’s test, the patient resists a downward force applied to the arm in 90 degrees of forward flexion with the palms facing up and the elbows straight (Fig. 3.23). Pain at the shoulder suggests biceps pathology at its origin, at the superior labrum, or within the bicipital groove; however, this test may elicit similar symptoms in patients with supraspinatus conditions. A confirmatory test is the Yergason’s sign in which the patient simultaneously resists a pronation force applied to the forearm and an external rotation force applied to the shoulder by the examiner (27).
The impingement signs are provocative maneuvers that are helpful in clarifying the diagnosis of rotator cuff disease or biceps tendinitis. Two signs of impingement are routinely examined and may be performed with the patient in the upright or supine positions. The first sign, described by Neer (8), is pain elicited with maximal passive glenohumeral forward flexion with the shoulder in neutral rotation, which impinges the inflamed supraspinatus and biceps tendons and the subacromial bursa under the anterolateral edge of the acromion (Fig. 3.24). The second sign, described by Hawkins and Bokor (19), Neer (24), and Hawkins and Hobeika (28), is pain elicited with glenohumeral forward flexion to 90 degrees, slight horizontal adduction, and internal rotation, which compresses the inflamed supraspinatus insertion at the greater tuberosity and subacromial bursa under the coracoacromial ligament (Fig. 3.25).
Once the entire physical examination is completed, a diagnostic subacromial impingement test may be performed to confirm the diagnosis of rotator cuff disease (8). In this test, 5 to 10 mL of 1% lidocaine is injected into the subacromial bursa to temporarily eliminate the patient’s symptoms of pain. Cortisone may also be included in the injection as a therapeutic treatment (Fig. 3.26). Patients with true impingement or rotator cuff disease should receive greater than 50% relief of pain when the impingement signs are repeated. In addition to pain relief, the cause of weakness elicited on examination is clarified. Weakness may be secondary to pain inhibition, muscular atrophy, or tendon rupture. If weakness persists despite the relief of pain after the injection, the rotator cuff is usually torn. Persistent pain should lead the physician to suspect other sources of shoulder pain.
Frequently, acromioclavicular arthritis accompanies rotator cuff disease in the elderly patient. Symptoms referable to the AC joint are clarified by the “cross-body” or horizontal adduction test. In this test, the arm is brought into 90 degrees of forward flexion. The arm is then adducted maximally, creating compression of the AC joint. Pain suggests pathology of this articulation. Subsequent injection of 2 mL of 1% lidocaine into the AC joint assists in determining the contribution of an AC condition to the patient’s symptoms.
FIGURE 3.25 Secondary or impingement II (Hawkins sign) is noted as pain with passive internal rotation of the shoulder in a position of 90 degrees of forward flexion.
FIGURE 3.26 The impingement test. The eradication of pain after the injection of lidocaine confirms rotator cuff disease.
Examination for Instability
Instability of the shoulder remains one of the more complex and interesting aspects of shoulder pathology. In recent years, a more thorough understanding of the variations in normal glenohumeral translation has evolved. Additionally, there continues to be advancements in the understanding of the true spectrum of the pathology associated with glenohumeral instability, including its relationship to rotator cuff disease. These changing concepts of the causes of shoulder symptoms as they relate to shoulder instability is evident in the overhead-throwing athlete in whom secondary impingement of the articular rotator cuff has been identified as a cause of shoulder pain related to instability (29).
The most common mechanism of shoulder instability is trauma, which may be acute or recurrent. The initial episode of instability usually is the result of a major force and frequently requires manipulation by a health-care worker to achieve a reduction. Subsequent dislocations may occur with less force. Patients who present with traumatic instability have been classified by the acronym TUBS (traumatic, unidirectional, Bankart, surgical, which is most appropriately treated by surgery) (15).
Atraumatic instability of the shoulder, which represents the more complex patient profile to evaluate and treat, has gained more attention recently. Some of these patients have an underlying collagen disorder, which results in laxity of all joints. Because of the global laxity of all structures of the shoulder, these patients present with multidirectional instability, which occurs as a result of minor trauma. The minor trauma may lead to disuse of the shoulder, which allows for weakening of the rotator cuff and further symptomatic instability of the shoulder. These patients have been classified by the acronym AMBRI (atraumatic, multidirectional, bilateral, recurrent, instability, which is most appropriately treated by rehabilitation aimed at strengthening the rotator cuff, and when indicated, surgery consists of an inferior capsular shift) (15).
A third group of patients are those in whom symptoms of unidirectional or multidirectional instability develop after repetitive microtrauma. This group includes the athletic population, especially throwers and other athletes who use overhead motion, in whom secondary impingement related to either underlying traumatic instability or congenital ligamentous laxity develops (29, 30). These patients may have symptoms of pain consistent with rotator cuff tendinitis instead of symptoms of instability.
History
Determining the origin of shoulder instability is essential in properly diagnosing and treating the unstable shoulder. The initial history addresses whether the patient’s instability is traumatic or atraumatic. The patient with traumatic instability should be asked about the position of the shoulder when the dislocation occurred and the magnitude and direction of the force that led to the dislocation. Additionally, patients should be asked about the frequency and the magnitude of the forces required to create recurrence of instability.
The more common anterior dislocation (31) occurs when a force is applied to the abducted and externally rotated upper extremity and frequently occurs in sporting activities such as basketball, football, volleyball, and waterpolo. Posterior shoulder dislocation is a much less common injury than anterior dislocations and for this reason, these patients are frequently misdiagnosed. Traumatic posterior instability classically occurs during a seizure or from electric shock (19), but it may also be caused by a posteriorly directed force applied to the extremity when the arm is forward flexed to 90 degrees, for example, in a motor vehicle accident when the patient’s hand is on the steering wheel or when a football player’s arms are in a blocking position.
Patients with multidirectional instability may be anterior-dominant or posterior-dominant depending on the direction of greatest laxity. Their history is much less well described. Patients may report either pain or instability, or they may not realize that their shoulder is unstable at all but they are unable to perform certain activities. Patients with multidirectional instability often do not recognize episodes of instability because the shoulder rarely stays subluxated or dislocated. The onset of their symptoms is usually insidious. An additional crucial component of the history is whether the instability is voluntary or involuntary; patients with voluntary instability are poor surgical candidates (32).
Throwers and other athletes who use overhand motion and who have shoulder pain should always be suspected of having instability as a cause for their symptoms. The description of a dead arm sensation may indicate a momentary instability episode during a violent overhand throw (7). Such persons may report night pain and other symptoms of rotator cuff disease as previously discussed (29).
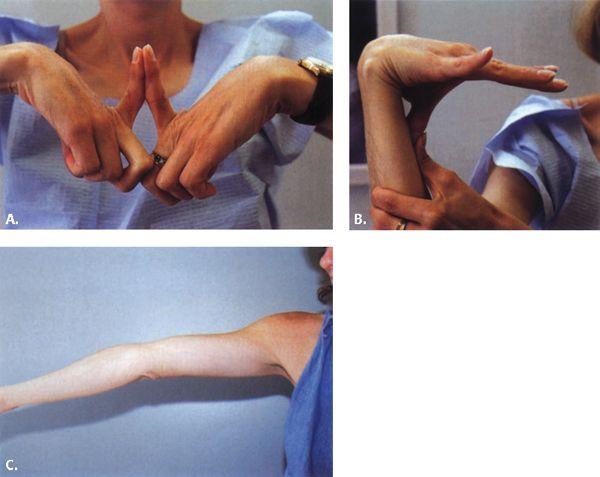
FIGURE 3.27 The sulcus sign. A: In the resting position, the patient’s shoulder has a relatively normal appearance. B: The examiner applies axial traction on the extremity, resulting in the sulcus being inferior to the lateral edge of the acromion.
Physical Examination
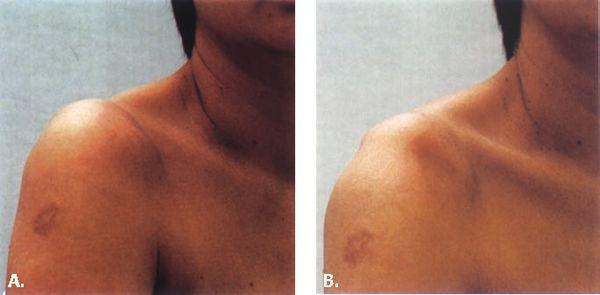
Inspection. The physical examination of a reduced glenohumeral joint in a patient with symptomatic instability may be unremarkable. Simple inspection of the shoulder at rest infrequently reveals findings of significance in the unstable shoulder, which, at the time of examination, is reduced. The examiner should inspect the patient’s shoulder girdle for evidence of a sulcus sign, which suggests inferior translation of the glenohumeral joint (Fig. 3.27). The examiner should evaluate the patient for findings of systemic laxity, which may contribute to multidirectional instability. These findings include the ability to hyperextend the elbows, hyperextend the metacarpophalangeal joint of the index finger, abduct the thumb so that it reaches the volar surface of the forearm, and hyperextend the elbows (Fig. 3.28). If the examiner suspects an underlying collagen disorder such as Marfan disease, a brief ocular inspection and cardiac examination should be performed.
FIGURE 3.28 In patients with suspected multidirectional instability, findings of joint laxity in other joints should be noted. A: Hyperflexibility of the index metacarpophalyngeal joint. B: The ability to touch the thumb to the volar surface of the forearm. C: The ability to hyperextend the elbow.
FIGURE 3.29 Apprehension/apprehension suppression test. A: The patient’s shoulder is positioned in 90 degrees of abduction and then maximally externally rotated. In patients with symptomatic anterior instability, the patient will experience apprehension that the shoulder will dislocate. B: A gentle posterior force is then applied to the anterior humerus, reducing the humeral head into the glenoid and suppressing the patient’s apprehension.
The acutely dislocated shoulder has the exaggerated sulcus noted below the acromion caused by the medial shift of the proximal humerus. In posterior dislocation, the arm is only comfortable to the patient in internal rotation, whereas the appearance of the shoulder is near normal. These subtle findings may easily be missed by even the experienced examiner. The most helpful inspection aid is the examination from above and behind the seated patient. From this vantage point, the examiner can appreciate differences in the anterior and posterior shoulder contours, which may be the most notable physical finding.
Palpation. Palpation of the unstable shoulder may, on occasion, reveal an inferior sulcus sign. This may be bilateral in patients with multidirectional instability. If the examiner palpates the shoulder while moving the shoulder, crepitus may be evident. This is rare but may be present in patients with numerous dislocations or subluxations in whom traumatic degenerative changes, Hill-Sachs lesions, or labral lesions are beginning to develop.
Range of Motion. Active and passive range of motion are rarely limited in patients with instability of the shoulder. However, patients who have recently experienced dislocations may experience apprehension or pain when the shoulder is put in a position of risk, for instance, abduction and external rotation in a patient who has recently experienced an anteroinferior dislocation.
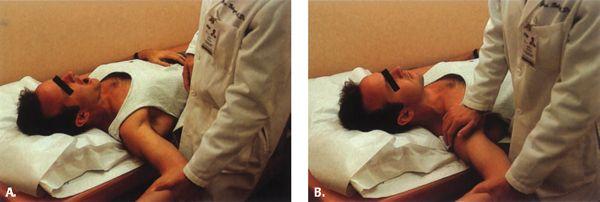
Provocative Maneuvers. After the passive range of motion portion of the physical examination, the apprehension test can be performed. The apprehension test is a provocative maneuver to evaluate the shoulder for anterior instability (Fig. 3.29A). This test is best performed with the patient supine. In this position, the patient is comfortable, thus eliminating extraneous symptoms and allowing focused examination on anterior capsulolabral stressing. The examiner brings the arm into 90 degrees of abduction. Slowly the arm is brought into increased external rotation. As the shoulder reaches approximately 90 degrees of external rotation, the humeral head may begin to subluxate anteriorly in a patient with anterior instability, making the patient apprehensive that dislocation is imminent (25). If the patient reports only pain with the apprehension testing, this may be a symptom related to impingement syndrome, rotator cuff disease, biceps tendinitis, or labral lesions. To confirm that symptoms are originating from the anterior subluxation of the humeral head, the examiner performs the Jobe relocation test. In this test, the examiner attempts to reduce the anterior subluxation of the glenohumeral joint by applying a gentle posteriorly directed pressure on the anterior aspect of the proximal humerus while the shoulder is maintained in the position of apprehension (Fig. 3.29B). If the patient’s symptoms are related to anterior instability, this maneuver will relieve the patient’s symptoms.
Posterior instability is tested by the posterior stress test. This test is performed on the seated or side-lying patient with the humerus forward flexed 90 degrees, adducted, and internally rotated and with the examiner applying a posteriorly directed force on the elbow, forcing the humeral head over the posterior rim of the glenoid. Because posterior instability is more frequently a subluxation than a true dislocation, patients do not react as strongly to this maneuver, but rather confirm that this position recreates their shoulder symptoms.
Stability Testing. Stability testing, although often difficult to perform effectively because of patient guarding, represents the mainstay of the assessment of the unstable shoulder. The purpose of this portion of the examination is to determine the direction and magnitude of instability. Many stability tests have been described, including the sulcus test, the drawer test, the shift and load test, and testing of anterior and posterior translation with the patient supine or lateral.
The sulcus test assesses inferior translation of the glenohumeral joint and determines the inferior component of multidirectional instability.
FIGURE 3.30 The load and shift test. Axial compression is placed on the abducted extremity, centering the humeral head in the glenoid. Anterior or posterior shift is then performed by the examiner to assess the level of instability.
In the drawer test, the patient is seated with the patient’s arm dangling comfortably at the side to prevent muscular guarding. The examiner stands behind the patient and grasps the humeral head with one hand while the other hand stabilizes the scapula. The examiner then applies an axial load to the humerus, compressing the glenohumeral articulation and centering the humeral head in the glenoid fossa. The examiner then applies an anteriorly directed force to the posterior aspect of the humeral head. In normal patients, a firm end point should be reached without evidence of the humeral head translating over the anterior lip of the glenoid. A posteriorly directed force is then applied to the anterior humerus and the posterior translation is determined. Posterior translation of up to half of the humeral head diameter is considered normal.
The limitation of the drawer test is that it is an evaluation of the shoulder stability in a position in which instability is rarely problematic. For example, patients with traumatic anteroinferior instability of the shoulder sustain an injury to the anteroinferior glenohumeral ligament–labral complex (1, 12, 13, 33). This ligament has been shown to provide stability to the glenohumeral articulation when the shoulder is abducted and externally rotated (34, 35). Thus, evaluation of shoulder stability with the arm in neutral abduction is of relatively little use in evaluating patients with this type of instability because the injured anteroinferior glenohumeral ligament is not stressed in neutral abduction. An evaluation that is performed with the arm in 90 degrees of abduction with rotation applied to discriminate between normal ligamentous laxity and pathologic instability represents a more effective examination technique.
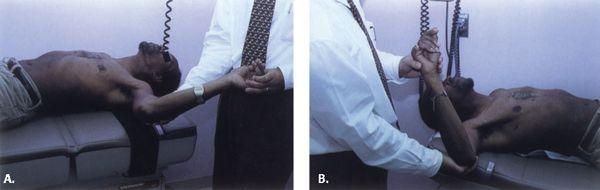
Shoulder stability testing with the arm in abduction with applied rotation can be performed with the patient in either a supine (Fig. 3.30) or lateral position. For testing patients in the lateral position, the patients are asked to lie comfortably on their side with their back toward the examiner at the edge of the examination table. The examiner grasps the patient’s extremity at the level of the elbow with one hand and abducts the patients arm to 90 degrees. The other hand grasps the humeral head between the thumb and index finger while stabilizing the scapula between the heel of the hand and the remaining three fingers. With varying degrees of external rotation applied by the examiner to the patient’s humerus, an anteriorly directed force is applied to the posterior humeral head. A clunk or dislocation may be felt. Subsequently, with varying degrees of internal rotation, a posteriorly directed force is applied to the anterior humeral head (Fig. 3.31).
Alternatively, rather than grasping the humeral head and scapula, the examiner may position the more proximal hand on the shaft of the humerus and apply an axial load to center the humeral head in the glenoid. An anterior or posterior force is then applied by the more proximal hand while varying the rotation with the other hand. This method of examination is easier to perform, but has the disadvantage of losing the stabilizing effect of the examiner’s proximal hand on the scapula. Additionally, more subtle translation may not be appreciated without the examiner’s fingers located near the joint line. In either case, both shoulders should be examined to determine side-to-side discrepancy.
FIGURE 3.31 Testing in the lateral position. A: The patient’s glenohumeral articulation is reduced by allowing the weight of the arm to center the humeral head in the glenoid. B: Posterior force applied to the humerus results in posterior dislocation of the glenohumeral joint in this patient with symptomatic traumatic posterior instability.
The examination may be performed in a similar fashion with the patient in the supine position. The primary advantage of supine testing is the ability to compare the afflicted shoulder with the contralateral side without having to reposition the patient. This is important when the examination is performed in the operating room under anesthesia (36, 37). Examination under anesthesia of instability may be necessary in clarifying shoulder instability because stability testing of the shoulder in the office setting may cause patient discomfort, resulting in guarding and a less sensitive examination.
Instability is graded by the amount of translation of the humeral head on the glenoid (37). Grade 1 is no translation, grade 2 is translation that is not sufficient for the humeral head to rise up on the rim of the glenoid, grade 3 is translation of the humeral head to but not over the rim of the glenoid, and grade 4 is dislocation of the glenohumeral articulation.
Examination of Superior Labrum–Anterior to Posterior Lesions
With the advent of arthroscopy of the shoulder, orthopaedists have gained a more thorough understanding of the shoulder joint and pathologic anatomy that may result in painful symptoms. Lesions of the superior labrum–biceps tendon complex, otherwise known as superior labrum–anterior to posterior, or SLAP, lesions, have been identified and classified arthroscopically and have been implicated as a previously overlooked source of shoulder symptoms (21, 38–42). Although this lesion has been observed in 6% to 12% of patients undergoing arthroscopy for shoulder symptoms, a classic history or reproducible physical finding to identify these lesions more effectively preoperatively has not been distinguished (40, 41).
Three mechanisms that lead to SLAP lesions have been proposed. In Snyder et al.’s (40, 41) series, the most common mechanism of injury was a fall onto the outstretched arm (31%). However, traction injuries (14%) such as those that result from lifting a heavy weight from a dead lift or overhead racquet sports and glenohumeral dislocations (16%) have also been documented as mechanisms leading to the development of SLAP lesions. The primary consistent symptom in all patients in Snyder et al.’s series was pain. An additional component of mechanical symptoms was noted in half of the patients in the study group.
On physical examination, no finding or specific test has been reported to reproducibly indicate underlying anterior labral conditions. Snyder et al. (40, 41) reported that only 34% of patients had symptoms referable to the long head of the biceps evaluated by biceps tension testing (Speed’s test). Crepitus suggestive of labral conditions was noted in 22% of patients. Most patients had findings relative to their associated findings. These signs were indicative of underlying impingement, rotator cuff tears, AC joint arthritis, and glenohumeral instability. Recently, a study reviewing numerous clinical assessments for SLAP lesions demonstrated significant variablity in all tests. These tests included the anterior slide test, the crank test, the active compression test, biceps load test I and II, pain provocation test, resisted supination external rotation test, rotation–compression test, and forced abduction test. Although the initial published reports describing these many tests demonstrated good sensitivity and specificity, the results were not validated by subsequent studies (43).
Examination for Acromioclavicular Joint Pathology
Acromioclavicular joint pain is often overlooked in shoulder pathology. The presentation may be misinterpreted as rotator cuff pathology or superior labral lesions. Thus, it is essential to thoroughly examine the AC joint in conjunction with a complete shoulder examination.
The two predominant pathologies of the AC joint are trauma and degenerative processes. Trauma to the shoulder may lead AC separations, which are graded I to VI (44–46). Grade II to VI injuries are usually diagnosed based on history and visual inspection alone. A deformity of the AC joint with a cephalad presentation of the distal clavicle relative to the acromion is noted when compared with the contralateral limb. Grade I injuries may or may not present with a notable deformity. Instead, the patient presents primarily with pain at the AC joint. This presentation is similar in the patient with degenerative processes.
Degenerative processes of the shoulder may be diagnosed by direct palpation of the AC joint to elicit pain. Additionally, three provocative tests will increase the sensitivity and specificity of the examination. These include the cross-body adduction stress test, the acromioclavicular resisted extension test, and the cross-arm adduction stress test (47).
Examination for Adhesive Capsulitis (Frozen Shoulder)
Adhesive capsulitis (frozen shoulder) is a pathologic process that is unique to the shoulder. It is often mis-diagnosed as impingement or rotator cuff disease, and therefore careful attention to the physical findings associated with this disease process is necessary to direct treatment. The patient generally reports the idiopathic onset of shoulder pain followed by weakness or stiffness. In most cases, the patient can recall a minor injury that may or may not be related to the onset of the process.
The most dramatic physical finding in adhesive capsulitis is the loss of normal shoulder range of motion. This finding is often attributed by the examining physician to pain in the shoulder as a result of rotator cuff impingement or tendinopathy. This diagnosis may lead to worsening of the limited range of motion because patients are frequently instructed to rest the shoulder for several weeks resulting in further capsular contracture and joint stiffness.
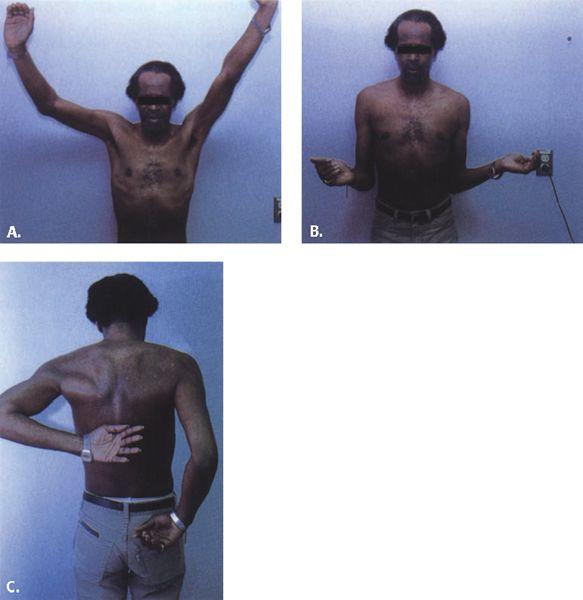
The most common restriction of motion is in external rotation tested in both 0 and 90 degrees of abduction, although all planes of motion are usually involved to some degree. Controversy exists over the exact diagnostic criteria for adhesive capsulitis. In general, a loss of approximately 50% of external rotation with limitation of combined forward elevation of 135 degrees or combined abduction of 90 degrees have all been considered criteria for the diagnosis of adhesive capsulitis (10), although patients with motion slightly better than that noted previously are likely to be experiencing the same pathologic process (Fig. 3.32).
FIGURE 3.32 Physical findings in patients with adhesive capsulitis include limitations in (A) forward elevation, (B) external rotation, and (C) internal rotation.
Examination for Specific Shoulder Disorders/Extrinsic
Extrinsic sources of shoulder pain include cervical radiculopathy, brachial plexopathy, postural pain, and neoplasm. These should be considered in all patients with shoulder disorders. This is especially true in patients in whom symptoms are not consistent with primary shoulder conditions or in patients with a history of cervical spine disease (18).
References
1. Rowe CR, Patel D, Southmayd WW. The Bankart procedure. A long-term end-result study. J Bone Joint Surg Am. 1978;60:1–16.
2. Altchek DW, Warren RF, Wickiewicz TL, et al. Arthroscopic acromioplasty. Technique and results. J Bone Joint Surg Am. 1990;72:1198–1207.
3. Ellman H. Diagnosis and treatment of incomplete rotator cuff tears. Clin Orthop Relat Res. 1990;254:64.
4. Constant CR, Murley AHG. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987; 214:160.
5. Richards RR, An K-N, Bigliani LU, et al. A standardized method for the assessment of shoulder function. J Shoulder Elbow Surg. 1994;3:347–352.
6. Hawkins RJ, Chris T, Bokor D, et al. Failed anterior acromioplasty. A review of 51 cases. Clin Orthop Relat Res. 1989;243: 106–111.
7. Rowe CR. Recurrent anterior transient subluxation of the shoulder. The ‘dead arm’ syndrome. Orthop Clin North Am. 1988;19:767–772.
8. Neer CS II. Impingement lesions. Clin Orthop Relat Res. 1983; 173:70.
9. Nevaiser JS. Adhesive capsulitis and the stiff and painful shoulder. Orthop Clin North Am. 1980;11:327.
10. Murnaghan JP. Frozen shoulder. In: Rockwood CA Jr, Matsen FA III, eds. The Shoulder. Philadelphia, Pa: WB Saunders; 1990:837–862.
11. Nevaiser RJ. Painful conditions affecting the shoulder. Clin Orthop Relat Res. 1983;173:63.
12. Bankart ASB. Recurrent or habitual dislocation of the shoulder joint. BMJ. 1923;2:1132.
13. Bankart ASB. The pathology and treatment of recurrent dislocation of the shoulder joint. BMJ. 1938;26:23.
14. Fronek J, Warren RF, Bowen M. Posterior subluxation of the glenohumeral joint. J Bone Joint Surg Am. 1989;71:205.
15. Matsen FA III, Thomas SC, Rockwood CA Jr. Glenohumeral instability. In: Rockwood CA Jr, Matsen FA III, eds. The Shoulder. Philadelphia, Pa: WB Saunders; 1990:526–622.
16. Pollock RG, Bigliani LU. Recurrent posterior shoulder instability: diagnosis and treatment. Clin Orthop Relat Res. 1993; 291:85–96.
17. Glockner SM. Shoulder pain: a diagnostic dilemma. Am Fam Phys. 1995;51:1677.
18. Zuckerman JD, Mirabello SC, Newman D, et al. The painful shoulder: Part I. Extrinsic disorders. Am Fam Phys. 1991;43:119–128.
19. Hawkins RJ, Bokor DJ. Clinical evaluation of shoulder problems. In: Rockwood CA Jr, Matsen FA III, eds. The Shoulder. Philadelphia, Pa: WB Saunders; 1990:149–177.
20. Inman VT, Saunders JB, Abbott LC. Observation of the function of the shoulder joint. J Bone Joint Surg Am. 1944;26: 1–30.
21. Schulte KR, Warner JJP. Uncommon causes of shoulder pain in the athlete. Orthop Clin North Am. 1995;26:505–528.
22. Lyons AR, Tomlinson JE. Clinical diagnosis of tears of the rotator cuff. J Bone Joint Surg Br. 1992;74:414–415.
23. Wiener BD, Rossario EJ, Feldman AJ. A comparison between physical examination and MRI in the detection of rotator cuff tears confirmed with arthroscopy. In: American Shoulder and Elbow Surgeons. Thirteenth Open Meeting at the American Academy of Orthopaedic Surgeons Annual Meeting; San Francisco, CA; 1997.
24. Neer CS II. Shoulder Reconstruction. Philadelphia, Pa: WB Saunders, 1990.
25. Hoppenfeld S. Physical Examination of the Spine and Extremities. East Norwalk, Conn: Appleton-Century-Crofts; 1976.
26. Gerber C, Krushell RJ. Isolated rupture of the tendon of the subscapularis muscle. J Bone Joint Surg Br. 1991;73:389–394.
27. Yergason RM. Supination sign. J Bone Joint Surg. 1931;13:160.
28. Hawkins RJ, Hobeika P. Physical examination of the shoulder. Orthopedics. 1983;6:1270–1278.
29. Jobe FW, Kvitne RS. Shoulder pain in the overhand throwing athlete: the relationship of anterior instability and rotator cuff impingement. Orthop Rev. 1989;18:963.
30. Kvitne RS, Jobe FW. The diagnosis and treatment of anterior instability in the throwing athlete. Clin Orthop Relat Res. 1993;291:107–123.
31. Rowe CR. Prognosis in dislocations of the shoulder. J Bone Joint Surg Am. 1956;38:957–977.
32. Rowe CR, Pierce DS, Clark JG. Voluntary dislocation of the shoulder. A preliminary report on a clinical, electromyographic, and psychiatric study of 26 patients. J Bone Joint Surg Am. 1973;55:445.
33. Reeves B. Experiments on the tensile strength of the anterior capsular structures of the shoulder in man. J Bone Joint Surg Br. 1968;50: 858–865.
34. O’Connell PW, Nuber GW, Mileski RA, et al. The contribution of the glenohumeral ligaments to anterior stability of the shoulder joint. Am J Sports Med. 1990;18:579–584.
35. Turkel SJ, Panio MW, Marshall JL, et al. Stabilizing mechanisms preventing anterior dislocation of the glenohumeral joint. J Bone Joint Surg Am. 1981;63:1208–1217.
36. Cofield RH, Irving JF. Evaluation and classification of shoulder instability—with special reference to examination under anesthesia. Clin Orthop Relat Res. 1987;223:32.
37. Cofield RH, Nessler JP, Weinstabl R. Diagnosis of shoulder instability by examination under anesthesia. Clin Orthop Relat Res. 1993;291:45–53.
38. Andrews JR, Carson WG, McLeod WD. Glenoid labrum tears related to the long head of the biceps. Am J Sports Med. 1985;13:337.
39. Snyder SJ, Karzel RP, Del Pizzo W, et al. SLAP lesions of the shoulder. Arthroscopy. 1990;6:274–279.
40. Snyder SJ, Banas MP, Karzel RP. An analysis of 140 injuries to the superior glenoid labrum. J Shoulder Elbow Surg. 1995;4: 243–248.
41. Snyder SJ, Banas MP, Belzer JP. Arthroscopic evaluation and treatment of injuries to the superior glenoid labrum. In: Pritchard DJ, ed. Instructional Course Lectures. Rosemont, IL: American Academy of Orthopaedic Surgeons; 1996:65–70.
42. Maffet MW, Gartsman GM, Moseley B. Superior labrum-biceps tendon complex lesions of the shoulder. Am J Sports Med. 1995;23 93–98.
43. Jones GL, Galluch DB. Clincal assessment of superior glenoid labral lesions. Clin Orthop Relat Res. 2007;455:45–51.
44. Allman FL Jr. Fractures and ligamentous injuries of the clavicle and its articulation. J Bone Joint Surg Am. 1967;49:774–784.
45. McPhee IB. Inferior dislocation of the outer end of the clavicle. J Trauma. 1980;20:709–710.
46. Rockwood CA Jr, Young DC. Disorders of the acromioclavicular joint. In: The Shoulder. Philadelphia, Pa: WB Saunders; 1990.
47. Chronopoulos E, Kim TK, Park HB, et al. Diagnostic value of clinical tests for isolated chronic acromiclavicular lesions. Am J Sports Med. 2004;32:655–661.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree