▪ Normal Variants and Common Benign Entities
Probably more than in any other organ system, the normal imaging appearance of the skeletal system is strikingly different in children from its appearance in adults ( Fig. 7-1 ). This is related to the changing appearance of growing and maturing bone. The most striking changes occur near the physes and apophyses. Many of the more common mistakes made in pediatric skeletal radiology are related to the misinterpretation of normal structures as being abnormal. Textbooks such as Keats’s Atlas of Normal Roentgen Variants That May Simulate Disease are dedicated to the normal radiographic appearances and variations of bones in children. The details of all of the normal changes in the radiographic appearance throughout the maturing skeleton cannot be covered here. The following section describes several commonly misinterpreted normal variants and benign entities.
Apophyseal and Epiphyseal Irregularity
The terms apophysis and epiphysis sound similar and have similar meanings. Their differences can be confusing. The term epiphysis refers to the part of bone that articulate with the adjacent bone. The primary growth plate, or physis, of the epiphysis is typically perpendicular to the longitudinal axis of the bone. Apophyses do not have an articular surface. The physis of an apophysis often courses parallel to the long axis of the bone. Apophyses act as a site of attachment for tendons.
In the growing child, apophyses and epiphyses in various parts of the body can have variable and often somewhat irregular appearances. Separate ossicles of an apophysis can mimic fragments, irregularity can mimic periosteal reaction, and mixed sclerosis and lucency can be confused with findings of an inflammatory or neoplastic process. Common apophyses that may have this appearance include tibial tuberosity, ischeal tuberosity, ischeal pubic synchondrosis, posterior calcaneal apophysis ( Fig. 7-2 ), and medial malleolus of the ankle ( Fig. 7-3 ). Irregularity and fragmentation are commonly seen in the normal tibial tuberosity. The calcaneal apophysis can often demonstrate a strikingly sclerotic appearance (see Fig. 7-2, C ). The ischeal pubic synchondrosis can appear very prominent (see Fig. 7-1, D ) and asymmetric.


Epiphyses can also appear irregular and even fragmented. The most common epiphyses with this irregular appearance are the distal femoral epiphysis ( Fig. 7-4 ) and the capitellum ( Fig. 7-5 ). It is important to recognize these irregularities as a normal stage of development and not confuse them with osteochondral lesions (in the distal femoral epiphysis or the capitellum) or with fracture (medial malleolus).
Distal Femoral Metaphyseal Irregularity
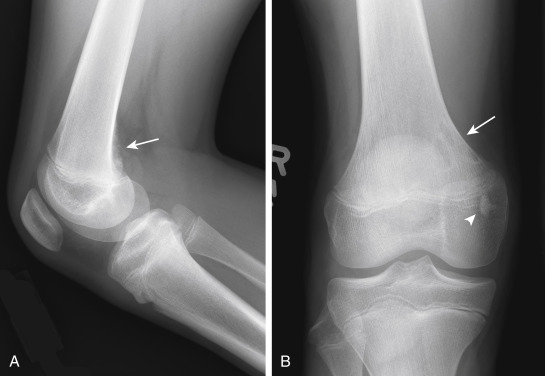
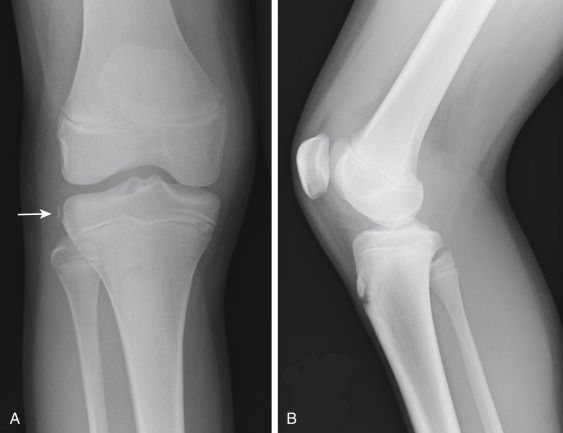
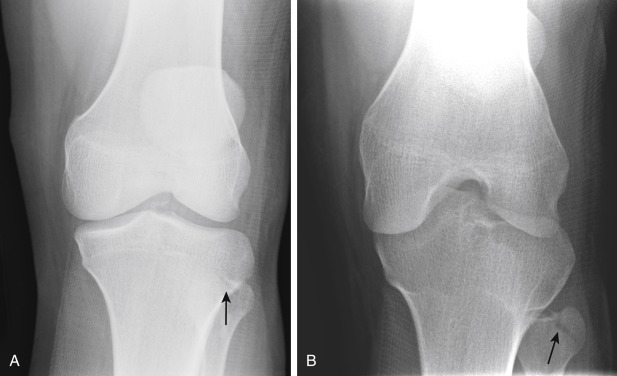
Distal femoral metaphyseal irregularity, also referred to as cortical desmoid or cortical irregularity syndrome, refers to the presence of irregular cortical margination and associated lucency involving the posteromedial aspect of the distal femoral metaphysis. It occurs in as many as 11% of boys aged 10 to 15 years. Although debated, its presence is thought to be related to chronic avulsion at the insertion of the adductor magnus muscle. Although this lesion can be associated with pain, it is often discovered incidentally, and its significance lies in its alarming radiographic appearance. On radiography there is cortical irregularity present along the posteromedial cortex of the distal femoral metaphysis, best seen on the lateral view ( Fig. 7-6 ). On frontal radiographs there may be an associated lucency (see Fig. 7-6, B ). Familiarity with the typical location, appearance, and patient age is important so that these lesions are not confused with aggressive malignancies. Because the lesions are often bilateral, confirmation of their benign nature can be made by demonstrating a similar lesion on radiographs of the opposite knee. In problematic cases, computed tomography (CT) or magnetic resonance imaging (MRI) can be used to demonstrate the characteristic findings: a characteristic scooplike defect with an irregular but intact cortex; no associated soft tissue mass; and a subtle contralateral lesion.
Benign Fibrous Cortical Defects
Benign fibrous cortical defects, or nonossifying fibromas, are commonly encountered lesions of no clinical significance. They are seen in as many as 40% of children at some time during development and are most common between 5 and 6 years of age. The term nonossifying fibroma is typically reserved for lesions larger than 3 cm. They occur most commonly within the bones around the knee and in the distal tibia. They appear as eccentrically based, well-defined, bubbly, lucent lesions. These benign tumors have a narrow zone of transition with thin cortical rims ( Figs. 7-7 through 7-9 ) and are typically round or oval in shape. When the characteristic pattern is identified, no further imaging or follow-up is necessary. Occasionally a pathologic fracture can occur through the lesion (see Fig. 7-9 ). Over time, benign fibrous cortical defects become more sclerotic and eventually resolve (see Fig. 7-7 ). When imaged during this healing process, they are sometimes referred to as ossifying nonossifying fibromas.


▪ Trauma
Fractures in children differ from those in adults for multiple reasons. Children’s bones have higher water content and are thus more pliable with a greater propensity to deform before breaking. This is akin to a new branch on a tree. Green sticks, with their higher water content, bend and deform before breaking.
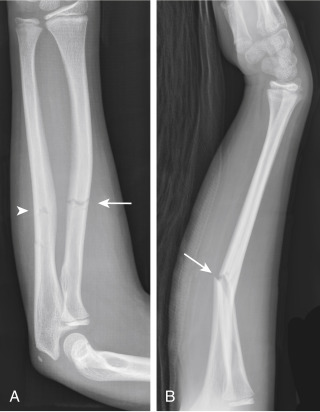
The term incomplete fracture refers to a fracture that does not extend through the entire diameter of the cortex. Because children’s bones are more elastic, incomplete fractures occur more commonly in children than adults. There are a number of types of incomplete fractures. Plastic bowing deformity ( Figs. 7-10 and 7-11 ) is diagnosed when there is a greater than expected curvature of the bone after trauma without a discrete fracture line. This type of fracture occurs almost exclusively in the radius, ulna, or fibula. At times this injury can be difficult to diagnose, and it is not until the follow-up image, when periosteal new bone is present, that the fracture can confidently be diagnosed. A buckle fracture is a concave buckling of the cortical surface of a long bone. Buckle fractures may be subtle and may appear only as an increase in acute angulation of a normally gentler curve ( Figs. 7-12 and 7-13 ). Buckle fractures are most common in the distal radius and ulna, the metacarpals and metatarsals, the phalanges, and the tibia. Finally, a greenstick fracture is an incomplete fracture along the cortex of the convex margin of the bowing ( Figs. 7-11 and 7-14 ). Greenstick fractures are most common in the forearm. Which name you give an incomplete fracture is not important. What is important is recognizing that a fracture is present when it has one of these incomplete appearances.



The potential for healing and the healing rate of fractures also differ in children and adults. Younger children heal very quickly. Periosteal reaction can be expected to be radiographically present 10 to 14 days after injuries in children. Children also tend to heal completely. Nonunited fractures are very uncommon in children. Fracture remodeling is also rapid and impressively complete in fractures of pediatric long bones. Normal alignment is typically restored.
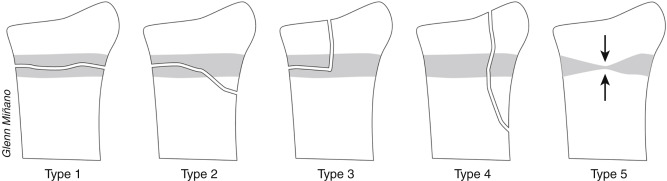
Involvement of the Physis
One of the potential problematic issues with fractures in children is involvement of the physis. The physis is involved in as many as 18% of pediatric long bone fractures. Physeal involvement may result in growth arrest of that limb and in a higher rate of necessary internal fixation. The standard classification for physeal fractures is that by Salter and Harris. It divides fractures into five types according to whether there is involvement of the physis, epiphysis, or metaphysis, as determined by radiography ( Fig. 7-15 ). Fractures with higher numbers by the Salter-Harris classification system have a greater incidence of complications. Type 1 fractures involve only the physis ( Fig. 7-16 ). They tend to occur in children younger than 5 years of age. On radiography the epiphysis may appear to be displaced in comparison with the metaphysis. However, type 1 fractures often reduce before the radiographs being obtained, making diagnosis extremely difficult. The potential findings of a type 1 fracture include soft tissue swelling adjacent to the physis, asymmetric widening of the physis, and/or displacement of the epiphysis. Salter-Harris type 1 injuries are uncommon and may only occur at the distal fibula and the proximal femur (as in a slipped capital femoral epiphysis [SCFE]). Type 2 fractures involve the metaphysis and physis but do not involve the epiphysis ( Figs. 7-9 and 7-17 ). They are the most common type of physeal injury, accounting for up to 75% of Salter-Harris fractures. On radiography there is typically a triangular fragment of the metaphysis attached to the physis and epiphysis. Type 3 fractures involve the physis and epiphysis but not the metaphysis( Figs. 7-18 and 7-19 ). Type 3 injuries have a greater predisposition for growth arrest. Type 4 injuries involve the epiphysis, physis, and metaphysis and, like type 3 injuries, are associated with a high rate of growth arrest ( Figs. 7-20 and 7-21 ). Type 5 fractures consist of a crush injury to part of or all of the physis. Like type 1 injuries, type 5 injuries are extremely difficult to diagnose. Often a diagnosis can be made only with a suspicious clinical history and comparison to the contralateral physis. With all Salter-Harris type fractures, it is important to assess the physis on follow-up images. Posttraumatic growth arrest is detected radiographically by demonstration of a bony bridge across the physis ( Fig. 7-22 ).







Commonly Encountered Fractures by Anatomic Location
Pediatric fractures have unique features in almost all locations. The following material reviews several of the more commonly encountered areas.
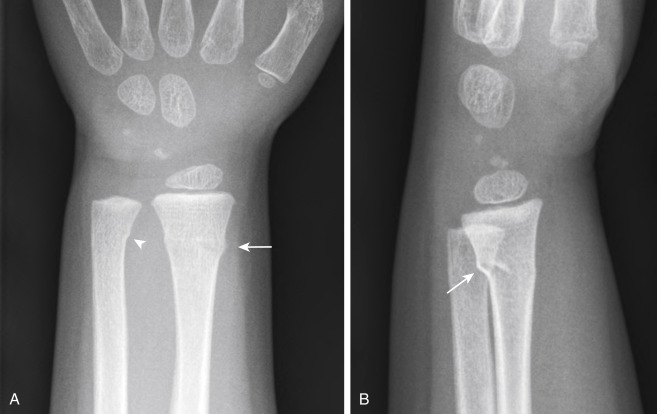
Wrist
The wrist is the most common fracture site in children. Most fractures of the distal forearm are buckle or transverse fractures of the distal metaphysis of the radius, with or without fracture of the distal ulnar metaphysis or styloid ( Figs. 7-13 and 7-23 ). It is important to assess all fractures of the distal radius for extension of the fracture line to the physis because the distal radius is also the most common area of physeal fracture (28% of physeal injuries occur in the distal radius). Displacement or obliteration of the pronator fat pad indicates a fracture or deep soft tissue injury. The normal pronator fat pad is visualized on a lateral view of the forearm as a thin line of fat with a mildly convex border. In most distal forearm fractures the convexity of the pronator fat pad is increased or the fat pad becomes obliterated by soft tissue attenuation.

Elbow
There are several unusual features that make elbow injuries in children different from those in adults. In contrast to adults, in whom fracture of the radial head is the most common injury, children most commonly experience supracondylar fractures ( Figs. 7-24 and 7-25 ). They occur secondary to hyperextension that occurs when falling on an outstretched arm. As many as 25% of such fractures are incomplete and may be subtle on radiography. On radiographs there can be posterior displacement of the distal fragment such that a line drawn down the anterior cortex of the humerus (anterior humeral line) no longer bisects the middle third of the capitellum (see Fig. 7-24 ). The fracture line is usually best seen through the anterior cortex of the distal humerus on the lateral view. A joint effusion is typically evident. Elbow effusions are identified when there is displacement of the posterior fat pad, resulting in its visualization on a lateral view ( Figs. 7-24 through 7-26 ). Normally the posterior fat pad rests within the olecranon fossa and is not visible on a true lateral view of the elbow. The anterior fat pad, which is often visible normally, may become prominent and have a prominent apex anterior convexity.
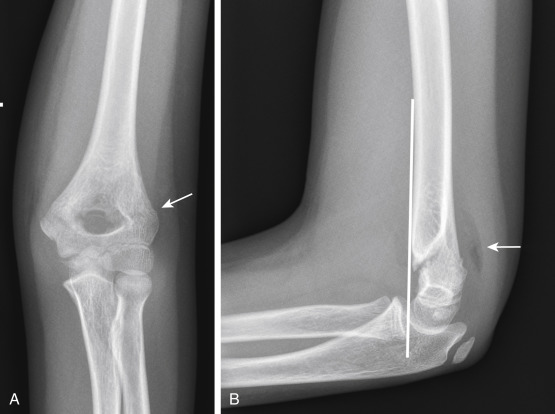


There is much debate about the significance of a traumatic elbow effusion in the absence of a visualized fracture (see Fig. 7-26 ). It is often taught that such a joint effusion is synonymous with an occult fracture. However, studies have shown that fractures are probably present in 50% or fewer cases. The point is moot because traumatic injury to the elbow is treated by splinting, whether a subtle fracture is identified or not. If pain persists, a repeat radiograph if often obtained at the follow-up orthopedic appointment and can be used to assess for signs of healing.
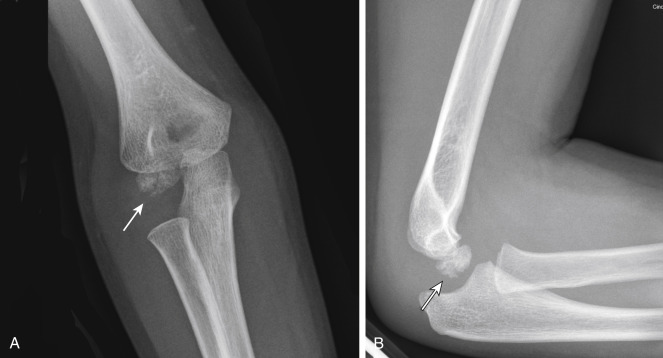
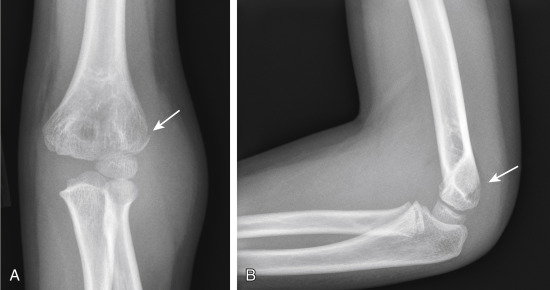
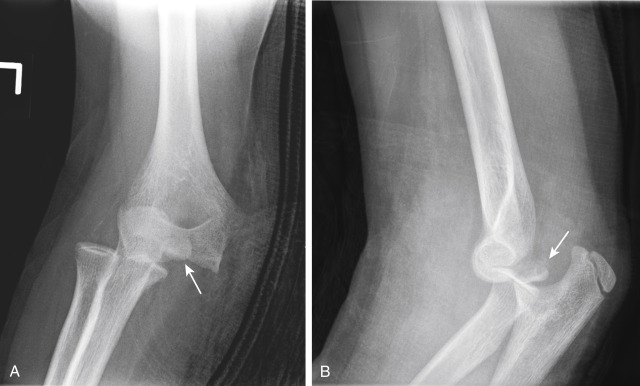
Other elbow injuries include fractures of the radial neck and lateral condyle ( Fig. 7-27 ) and avulsion of the medial epicondyle (Little League elbow; Figs. 7-28 and 7-29 ). With avulsion of the medial epicondyle (10% of elbow injuries), the medial epicondyle may become displaced and even entrapped within the elbow joint (see Fig. 7-29 ). It is important to know the predictable order of maturity of the elbow ossification centers so that a displaced medial epicondyle is not missed. The order can be remembered by the mnemonic CRITOE (capitellum, radial head, internal [medial] epicondyle, trochlea, olecranon, external [lateral] epicondyle).

Whenever there is a fracture of the forearm, it is important to evaluate the radial-capitellar joint for potential dislocation of the radial head. The radial head should align with the capitellum on both the anteroposterior (AP) and lateral views. If it does not, radial head dislocation should be suspected ( Fig. 7-30 ). When a radiocapitellar dislocation is present, it is important to image the entire forearm to look for a fracture-dislocation injury. A Monteggia fracture is a dislocation of the head of the radius with an associated fracture of the ulnar diaphysis (see Fig. 7-30 ).

Ankle
The ankle in a commonly injured joint due to combination of inversion and eversion injuries with weight bearing. There are two common fractures that are unique in adolescents, triplane fractures and juvenile Tillaux fractures. Like the name implies, a triplane fracture is a fracture in three planes: the coronal plane through the tibial metaphysis, transverse plane through the physis, and sagittal plane through the epiphysis ( Fig. 7-31 ). Because the fracture extends through the metaphysis and epiphysis, this is a Salter-Harris type IV fracture. Triplane fractures occur in adolescents in whom the growth plate is beginning to close. It is important to evaluate the fracture carefully because internal fixation is performed if there is more than 2-mm displacement of the fracture fragment. Often a CT is performed to evaluate the fracture and the degree of displacement more accurately. Fibular fractures are present approximately half of the time.

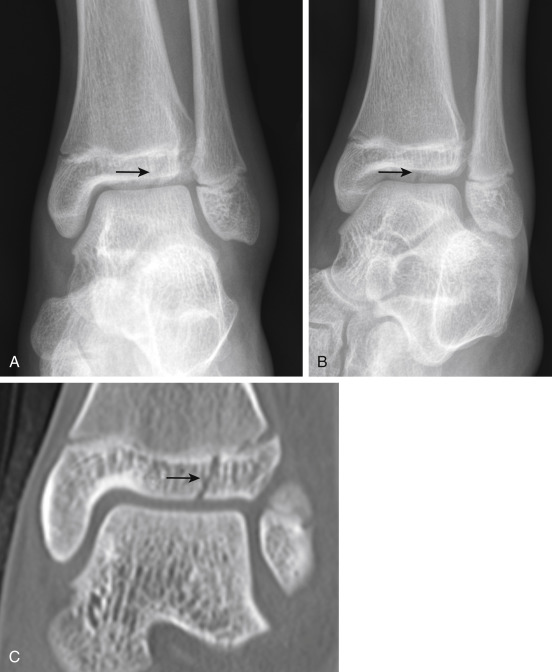
Juvenile Tillaux fractures are Salter-Harris type III fractures of the distal tibia. Like triplane fractures, they occur in adolescents in whom the growth plate is beginning to close. The fracture occurs because the medial tibial physis closes before the lateral physis. The differences in structural stability lead to this fracture pattern when there is abduction and external rotation of the ankle. On x-ray there is a fracture line through the distal tibial epiphysis and widening of the medial aspect of the ankle mortise ( Fig. 7-32 ). CT is performed to evaluate the amount of fracture displacement. Orthopedic surgeons will perform internal fixation if the fracture is displaced by more than 2 mm.
Toddler Fracture
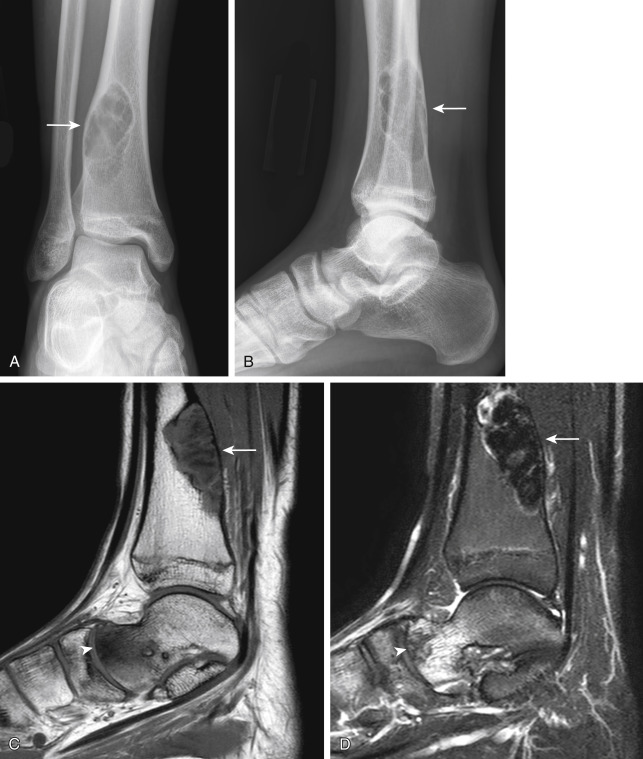
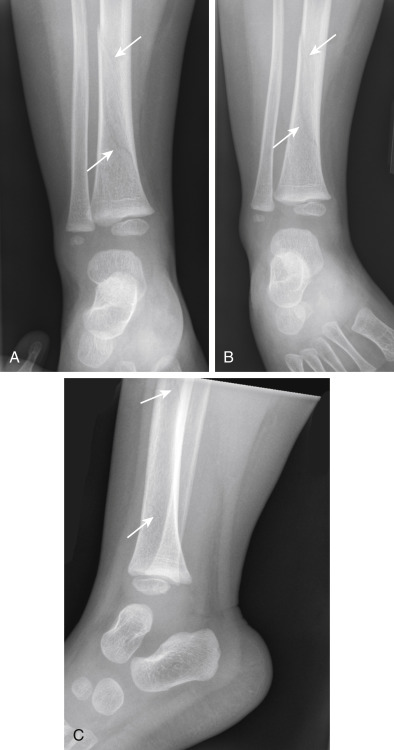
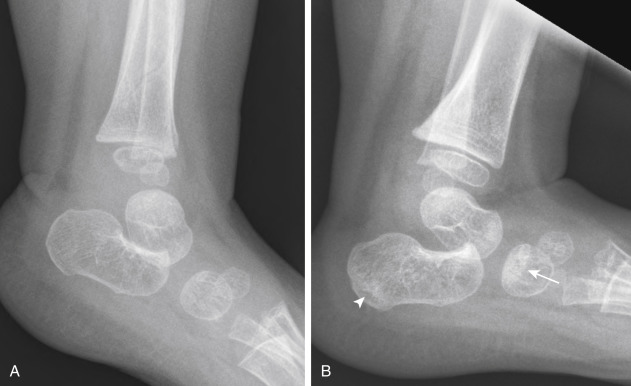
There are a number of fractures referred to as toddler fractures. The most common of these is a nondisplaced oblique or spiral fracture of the midshaft of the tibia ( Fig. 7-33 ). Such an injury is relatively common and occurs when a child first begins to walk. Most children present with failure to continue to walk or refusal to bear weight on that extremity. Oblique views often demonstrate the fracture better than do frontal or lateral views. When diagnosing this fracture, it is important to look at the patient’s age because a spiral fracture in a child who is not yet walking can be a fracture of abuse. Other types of toddler fractures include stress-type fractures involving the calcaneus or cuboid ( Figs. 7-34 and 7-35 ).

Avulsion Fractures in Adolescents
An avulsion injury is a structural failure of bone at a tendon or aponeurotic insertion and is related to a tensile force being applied by a musculoskeletal unit. Adolescents are prone to avulsive injuries because of a combination of their propensity to have great strength, their ability to sustain extreme levels of activity, and their immature, growing apophyses. The growing apophysis is often more prone to injury than the adjacent tendons. The sites of insertion of muscles capable of generating great forces are most predisposed to avulsion injuries.
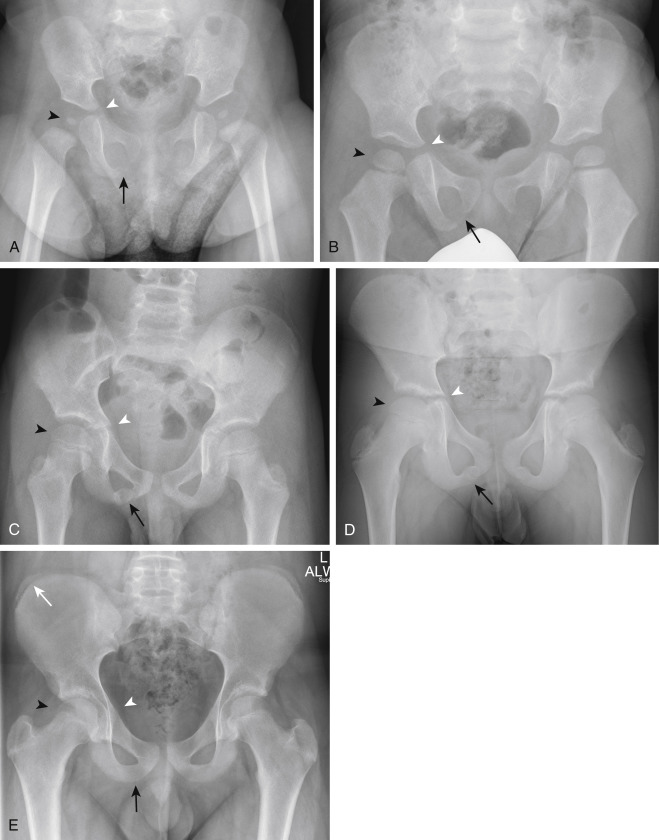
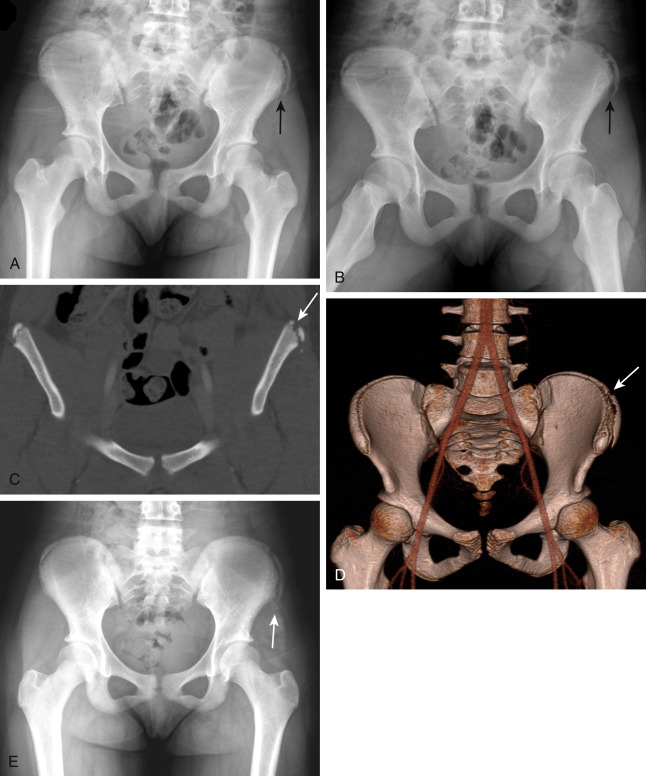
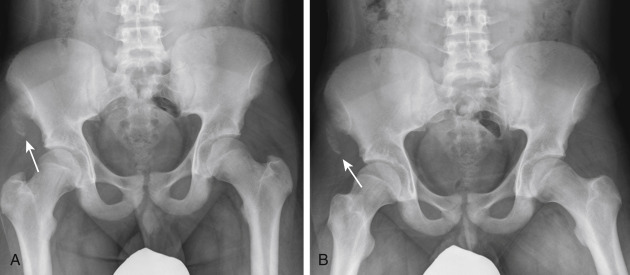
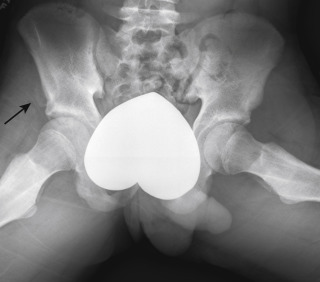
Radiologists may encounter findings of chronic avulsion when patients are imaged for pain or incidentally when imaging is performed for other reasons. The irregularity and periostitis that can be associated with chronic avulsions should not be misinterpreted as suspicious for malignancy. In addition, if unwarranted biopsies of these areas are performed, the histologic changes associated with the healing callus of the avulsion injury may be misinterpreted as malignancy. The most common sites of avulsion occur within the pelvis, where muscles capable of great force attach. Common sites of pelvic apophyseal avulsions and their associated muscular attachments include the iliac crest (transversalis, internal oblique abdominalis, external oblique abdominalis; Fig. 7-36 ); anterior superior iliac spine (Sartorius; Fig. 7-37 ); anterior inferior iliac spine (rectus femoris; Fig. 7-38 ); ischial apophysis (hamstring muscles: biceps femoris, gracilis, semimembranosus, semitendinosus; Fig. 7-39 ); and lesser trochanter (iliopsoas). The radiographic findings of avulsion injuries include displacement of the ossified apophysis from normal position and variable, often exuberant amounts of associated periosteal new bone formation.

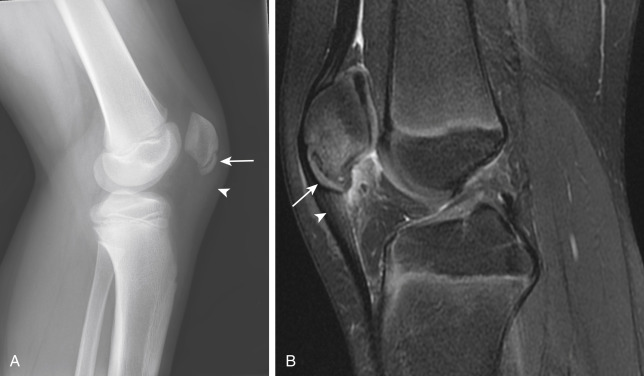
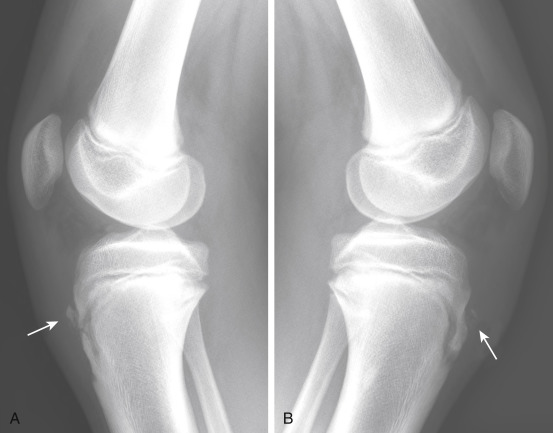
When involving a joint, avulsive injuries can occur at the cortical insertion site of a ligament or tendon. The knee is the joint most commonly associated with avulsive injuries. Many of these injuries occur exclusively in children and adolescents. Common sites of knee avulsion fractures and their associated tendinous or ligamentous attachments include the anterior medial tibial spine (anterior cruciate ligament; Fig. 7-40 ); lateral tibial rim, also known as a Segond fracture (lateral collateral ligament; Fig. 7-41 ); fibular head (conjoined tendon with biceps femoris; Fig. 7-42 ); tip of the fibular head (arcuate ligament); inferior pole of the patella, also known as the patellar sleeve (proximal patellar tendon; Figs. 7-43 and 7-44 ); and tibial tubercle (distal patellar tendon Fig. 7-45 ). Many of these injuries present with sudden pain and a joint effusion. MRI is often indicated because these injuries are associated with other internal derangement.

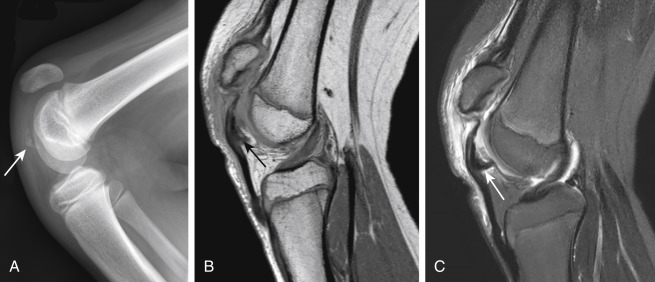


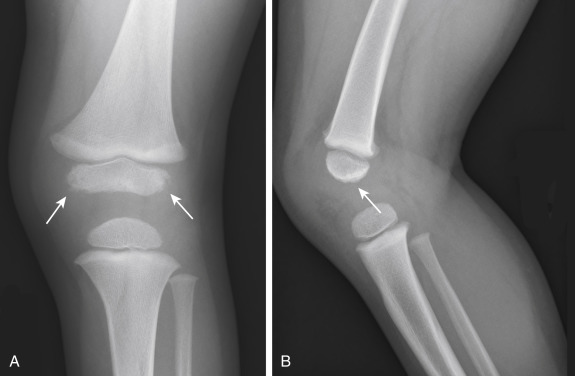
Chronic avulsion injuries are also common in the adolescent knee. Avulsion of the patellar tendon at its attachment to the patella is called Sinding-Larsen-Johansson syndrome. It occurs most commonly in children between the ages of 10 and 14 years. Symptoms include localized pain and swelling over the inferior aspect of the patella associated with restricted knee motion. Radiography demonstrates irregular bony fragments at the inferior margin of the patella, associated with adjacent soft tissue swelling and thickening and indistinctness of the patellar tendon ( Fig. 7-46 ). Chronic avulsive injury of the patellar tendon at its inferior attachment is referred to as Osgood-Schlatter disease (tibial tuberosity avulsion). It is a common disorder that most often affects active adolescent boys. Symptoms include pain and swelling over the tibial tuberosity. Radiography demonstrates bony fragmentation of the tibial tuberosity, associated adjacent soft tissue swelling, and thickening and indistinctness of the patellar tendon ( Fig. 7-47 ).
Child Abuse
Child abuse, also referred to as the more politically correct and less graphic nonaccidental trauma , is unfortunately common. According to data from the U.S. Department of Health and Human Services, it is estimated that approximately 750,000 children are abused and 1600 killed each year in the United States ( http://www.acf.hhs.gov/programs/cb/resource/cwo-08-11 ). Most abused children are less than 1 year of age and almost all are less than 6 years of age. When clinical or imaging findings are suspicious for potential abuse, a radiographic skeletal survey is typically obtained. The purpose of the skeletal survey is to document the presence of findings of abuse. In young children a head CT is often performed to identify intracranial signs of abuse. Other tests sometimes used include a repeat skeletal survey after approximately 2 weeks to look for healing injuries not seen on the initial skeletal survey, skeletal scintigraphy, abdominal CT, and MRI of the brain. The identification and reporting of findings of child abuse by the radiologist is an important task. False-positive cases can cause a nonabused child to be removed from his or her family, whereas false-negative cases can result in a child’s returning to a potentially life-threatening environment.
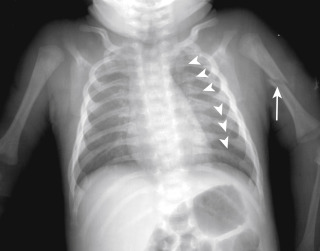
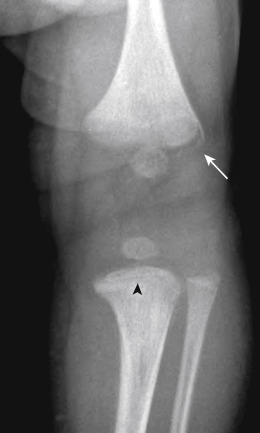
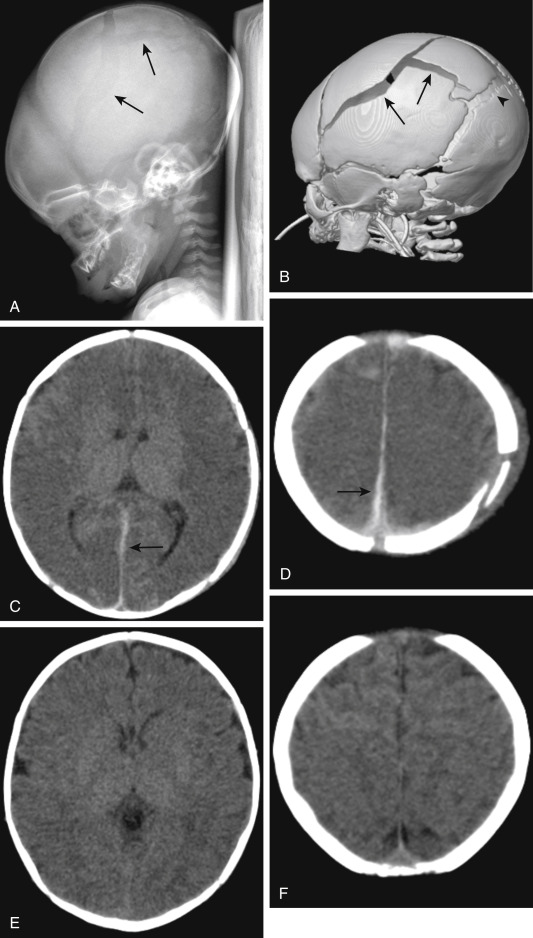
The radiographic findings of abuse vary in their specificity. One of the highly specific findings is the presence of posterior rib fractures occurring near the costovertebral joints ( Fig. 7-48 ). These are thought to occur when an adult squeezes an infant’s thorax. Such rib fractures may be subtle before development of callus formation. The evaluation for rib fractures should be a routine part of the evaluation of the chest radiograph of any infant. Another finding that is highly specific for abuse is the metaphyseal corner fracture ( Fig. 7-49 ). This fracture extends through the primary spongiosa of the metaphysis, the weakest portion, and usually occurs secondary to forceful pulling of an extremity. The broken metaphyseal rim appears as a corner fracture (a triangular piece of bone) when seen tangentially or as a crescentic rim of bone (referred to as a bucket-handle fracture) when seen obliquely. Other fractures associated with abuse include those of the scapula, spinous process, and sternum. Spiral long bone fractures in nonambulatory children are also highly suspicious. Multiple fractures in children of various ages (some with callus and some acute), as well as multiple fractures of various body parts, are highly suspicious for abuse (see Fig. 7-48 ). In fact, any fracture in an infant should be viewed with suspicion because as many as 30% of fractures in infants are secondary to abuse. Extraskeletal findings seen in abuse include acute or chronic subdural hematoma, cerebral edema (asphyxia), intraparenchymal brain hematoma ( Fig. 7-50 ), lung contusion, duodenal hematoma, solid abdominal organ laceration, and pancreatitis.
The clinical and imaging findings of abuse do not usually require differential diagnosis. However, other entities that may cause multiple fractures or that may cause radiographic findings that could be confused with injury, such as periosteal reaction, should always be considered. The other disorders that may present with multiple fractures in an infant are osteogenesis imperfecta (OI) and Menkes syndrome. Both of these entities are also associated with excessive wormian bones and osteopenia. There has been some debate about whether some patients diagnosed with child abuse do not suffer from vitamin D deficiency. Rickets, caused by vitamin D deficiency, is not a cause of the fractures specific for abuse, and most pediatric radiologists believe that the imaging appearance of child abuse and that of rickets do not overlap.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree