History and Clinical Findings
A 31-year-old man had fallen 4 weeks earlier during a soccer match. He had attempted to break his fall with his hands. Afterward he complained of pain on the radial side of his right wrist and painful limitation of motion, especially on extension. He reported that his hand had been swollen for several days after the fall. Radiographs of the right wrist were interpreted as normal (Fig. 6.1).
Fig. 6.1a, b Radiographic examination of the right wrist after trauma. The radiographs were interpreted as normal.
Further Case Summary
The attending trauma surgeon was sure that the patient had sustained a scaphoid fracture due to the typical clinical findings (tenderness over the snuffbox, pain on axial compression of the thumb). This prompted him to request spot radiographs of the scaphoid in two different oblique projections. The spot films revealed a Herbert type B2 scaphoid fracture (unstable, nondisplaced fracture through the middle third of the scaphoid, Figs. 6.2, 6.3).
Error Analysis and Strategy for Error Prevention
As in the present case, up to 70% of scaphoid fractures are missed on standard radiographic projections in two planes because the capsule and ligaments tend to reduce the fragments to an anatomical position. When clinical findings are suspicious for a scaphoid fracture, the wrist should first be radiographed in two planes to provide an overview of the radius, ulna, and carpal bones. With the hand in a neutral position, these survey views may not demonstrate the fine line of a fresh, nondisplaced fracture due to the minimal absorption differences and superimposed shadows, even when the injury is known (Fig. 6.1). Given the doubly oblique orientation of the scaphoid bone, spot views in pronation and supination are often better for positioning the scaphoid parallel to the imaging plane. The purpose of these oblique projections is to correct for the palmar angulation of the scaphoid and image the bone perpendicular to its long axis (the four views in Fig. 6.1 and Fig. 6.2 are called the “scaphoid quartet”). If the survey and spot films do not reveal a scaphoid fracture in clinically suspicious cases, the prognostic and therapeutic implications of this injury warrant investigation by CT or MRI to prevent the fracture from going on to necrosis or nonunion.
Fig. 6.2a, b Spot radiographs of the scaphoid bone in the dorsovolar projection demonstrate a nondisplaced, horizontal fracture through the middle third of the scaphoid (Herbert type B2).
a View with the wrist pronated approximately 15°.
b View with the wrist supinated approximately 15°.
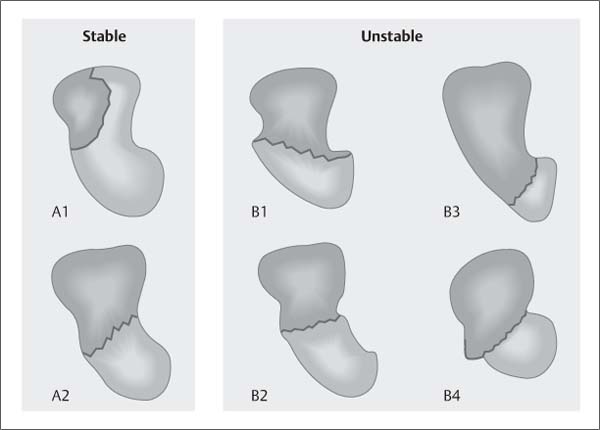
Fig. 6.3 Herbert classification of acute and subacute scaphoid fractures (after Treitl et al. 2002). A1 = fracture of the scaphoid tubercle, A2 = incomplete fracture of the middle third, B1 = distal oblique fracture, B2 = complete fracture of the middle third, B3 = fracture of the proximal pole, B4 = transscaphoid perilunar fracture with carpal dislocation.
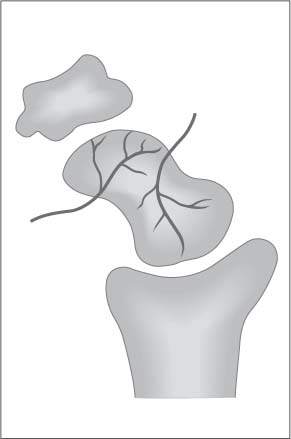
Fig. 6.4 Arterial blood supply of the scaphoid in the lateral view (after Treitl et al. 2002).
Scaphoid Fractures
Approximately 60% of wrist fractures involve the scaphoid bone. The ratio of scaphoid to radial fractures is approximately 1:10. Males between 15 and 40 years of age are predominantly affected. Most scaphoid fractures are caused by a fall onto the hyperextended hand. This mechanism drives the scaphoid bone up against the posterior margin of the radius, which acts as a fulcrum. While the proximal scaphoid is fixed to the radius by the radioscaphocapitate ligament, the force vector acts directly on the distal pole of the scaphoid. Even with a complete scaphoid fracture, the fragments are often undisplaced because the extrinsic capsule and ligaments hold them in an approximately normal position. The middle third of the scaphoid is most commonly affected. Scaphoid fractures are often associated with other fractures and tendon/ligament injuries. The exact location of the fracture has prognostic importance because the distal and middle portions of the scaphoid have a better blood supply than the proximal pole (Fig. 6.4). As a result, proximal scaphoid fractures are more likely to go on to nonunion than fractures at other sites.
Stability and treatment. The imaging goal in patients with an acute (< 2 weeks post injury) or subacute scaphoid fracture (2–6 weeks post injury) is to distinguish a stable fracture, which can be managed conservatively, from an unstable fracture, which requires surgical treatment.
Stable: Fractures of the scaphoid tubercle, incomplete fractures, and nondisplaced transverse fractures of the middle third. Unstable: Distal oblique fractures, displaced transverse fractures of the middle third, all proximal third fractures, and transscaphoid perilunar fracture-dislocations.
References and Further Reading
Greenspan A. Orthopedic Imaging: A Practical Approach. 4th ed. Philadelphia: Lippincott Williams & Wilkins; 2005
Treitl M, Stäbler A, Reiser M. Bildgebende Diagnostik der Hand-wurzel. Radiologie up2date 2002; 1: 93–120
History and Clinical Findings
A 92-year-old woman suffering from osteoporosis was taken to the emergency room with a fracture of the distal left femur. Initial radiographs showed an extra-articular fracture of the distal femoral diaphysis (Fig. 6.5). A pre-operative lateral view was omitted because of the poor clinical condition of the patient. At operation, the fracture was stabilized with an intramedullary nail under image intensifier control. Postoperative radiographs of the left femur taken in the ICU not only showed the surgically stabilized distal femoral fracture (Fig. 6.6c, d) but also revealed a new, posteriorly displaced fracture of the proximal femur, which was visible in the lateral projection in the second round of radiographs (Fig. 6.6b).
Fig. 6.5a, b Preoperative radiographs showed an extra-articular fracture of the distal left femur with shortening, lateral displacement, and rotational displacement of the distal femur.
Fig. 6.6a–d Postoperative radiographs taken in the ICU. The radiographs are presented in chronological order.
Further Case Summary
The image intensifier used at operation confirmed that the original fracture was confined to the distal femoral diaphysis. The postoperative lateral radiograph revealed a new fracture of the proximal femur (Fig. 6.6b).
This fracture, then, occurred while the patient was being positioned for the second round of radiographs. Afterward the patient confirmed that she had felt a sudden pain during the examination. Positioning was difficult due to patient immobility. The intramedullary nail had acted as a lever and pressed sharply against the posterior femoral cortex, which had already been weakened due to osteoporosis. The second fracture was successfully treated by internal fixation on the following day (Fig. 6.7).
Fig. 6.7a, b Radiographic examination of the left femur after removal of the first intramedullary nail and the insertion of a longer intramedullary nail with cross screws. The new nail extends the full length of the femoral diaphysis.
Error Analysis and Strategy for Error Prevention
The following errors were made during the postoperative radiographic examination (Fig. 6.6):
 Both technologists who performed the radiographic examination on the bed-confined 92-year-old patient had underestimated the fragility of the osteoporotic bone. During positioning of the cassette, the distal femur had been elevated from a relatively fixed position of the hip. During this maneuver the intramedullary nail pressed hard against the posterior femoral cortex, causing the proximal blowout fracture that was visible on postoperative films. This type of error could easily provide grounds for subsequent litigation.
Both technologists who performed the radiographic examination on the bed-confined 92-year-old patient had underestimated the fragility of the osteoporotic bone. During positioning of the cassette, the distal femur had been elevated from a relatively fixed position of the hip. During this maneuver the intramedullary nail pressed hard against the posterior femoral cortex, causing the proximal blowout fracture that was visible on postoperative films. This type of error could easily provide grounds for subsequent litigation.
 The mA·s product was set too high for the proximal femoral radiographs (Fig. 6.6a, b). Because of this, the proximal thigh was imaged in the “shoulder” part of the gradation curve rather than its linear portion, and regional differences in the radiation dose delivered to the film were not converted into gray-scale differences in a linear fashion. This resulted in a dark, low-contrast appearance of the fracture zone.
The mA·s product was set too high for the proximal femoral radiographs (Fig. 6.6a, b). Because of this, the proximal thigh was imaged in the “shoulder” part of the gradation curve rather than its linear portion, and regional differences in the radiation dose delivered to the film were not converted into gray-scale differences in a linear fashion. This resulted in a dark, low-contrast appearance of the fracture zone.
In a different patient 89 years of age, postoperative radio-graphs were taken to assess the fixation of a left femoral neck fracture with a dynamic hip screw. Initial radio-graphs of the right hip showed no abnormalities (Fig. 6.8a, b). When the technologist was questioned, it was learned that she had x-rayed the right hip instead of the left hip, where the surgery had actually been performed. Subsequent radiographs of the left hip showed an unstable femoral neck fracture that had been stabilized with a dynamic hip screw. The films showed impaction, shortening, axial rotation, and medial angulation of the femoral diaphysis (Fig. 6.8c, d). As a result of these findings, the femoral head and neck were resected and a total hip replacement was performed. A detailed review of the case showed that the radiology technician had not asked the patient which side required imaging and had failed to note the absence of a surgical scar. There was no valid indication for imaging the right hip, and this type of error would furnish definite grounds for a malpractice claim.
Fig. 6.8a–d Radiographs in an 89-year-old woman referred for evaluation of a femoral neck fracture stabilized with a dynamic hip screw.
a, b Initial radiographic examination of the right hip. A side marker was not placed in b.
c, d Second radiographic examination.
References and Further Reading
American College of Radiology (ACR). ACR Practice Guideline for Diagnostic Reference Levels in Medical X-ray Imaging. http://www.acr.org/SecondaryMainMenuCategories/quality_safety/RadSafety/RadiationSafety/guideline-diagnostic-reference.aspx (accessed November 10, 2010)
Amis ES, Butler PF, Applegate KE, et al. American College of Radiology White Paper on Radiation Dose in Medicine. J Am Coll Radiol 2007; 4: 272–284. http://www.acr.org/Secondary-MainMenuCategories/quality_safety/white_paper_dose.aspx (accessed November 10, 2010)
Council Directive 96/29/EURATOM of 13 May 1996 laying down basic safety standards for the protection of the health of workers and the general public against the danger arising from ionizing radiation. http://ec.europa.eu/energy/nuclear/radioprotection/doc/legislation/9629_en.pdf (accessed January 10, 2011)
Council Directive 97/43/EURATOM of 30 June 1997 on health protection in individuals against the dangers of ionizing radiation in relation to medical exposure, and repealing Directive 84/466/Euratom. http://ec.europa.eu/energy/nuclear/radioprotection/doc/legislation/9743_en.pdf (accessed January 10, 2011)
Sonnek C, Bauer B. Die neue Röntgenverordnung. Verordnung über den Schutz vor Schäden durch Röntgenstrahlen (Röntgenverordnung RöV) vom 8. Januar 1987 (BGBl. I S 114), zuletzt geändert durch Verordnung vom 18. Juni 2002 (BGBl. I S 1869). Berlin: H. Hoffmann; 2002
History and Clinical Findings
A 67-year-old man was referred from radiotherapy for pelvic radiographs because of pain in the right hip (Fig. 6.9). He had a history of metastatic adenocarcinoma from an unknown primary tumor (CUP) with lesions in the liver, lungs, mediastinal lymph nodes, and ribs. The radiology report described degenerative changes in the lower lumbar spine. Osteolytic and osteoplastic changes were excluded, although the lower portion of the sacrum could not be evaluated due to superimposed iodinated contrast medium in the bladder following a previous examination with IV contrast administration.
Fig. 6.9 Radiographic examination of the pelvis, interpreted as normal.
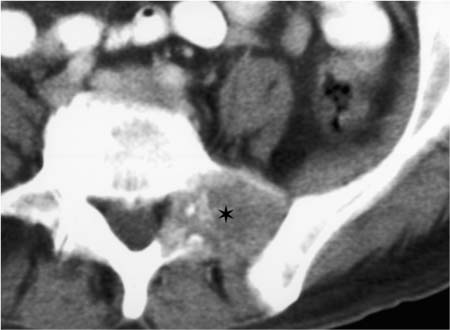
Fig. 6.10 Abdominal CT shows destruction of the left pedicle and left transverse process of L5 with an extraosseous soft-tissue component (asterisk).
Fig. 6.11 Pelvic radiograph. Magnified view of the osteolytic area (circled).
Further Case Summary
An abdominal CT examination performed earlier in the day showed an osteolytic metastasis in the left pedicle and left transverse process of the L5 vertebra (Fig. 6.10). In retrospect, this finding was also visible on the pelvic radio-graph (Fig. 6.11). A lumbosacral transitional vertebra with degenerative changes was noted on the left side as an incidental finding. Chemoradiation was prescribed for the disseminated metastases. A small-cell lung cancer was later identified histologically as the primary tumor.
Error Analysis and Strategy for Error Prevention
Radiographic examination of the pelvis was not indicated in this patient because the pelvic skeleton had already been evaluated earlier that day by CT, which is superior to plain films. The clinical request for pelvic radiographs contained no information on the CT examination, although scrutiny of the patient’s chart and questioning of the patient would have drawn attention to the duplicated examination. When the radiographs were interpreted, the opacified bladder urine should have indicated the previous CT examination and called the radiographic findings into question.
Destruction of the left pedicle and left transverse process of L5 was presumably missed because the original clinical problem was right hip pain.
References and Further Reading
American College of Radiology (ACR). ACR Practice Guideline for Diagnostic Reference Levels in Medical X-ray Imaging. http://www.acr.org/SecondaryMainMenuCategories/quality_safety/RadSafety/RadiationSafety/guideline-diagnostic-reference.aspx (accessed November 10, 2010)
Amis ES, Butler PF, Applegate KE, et al. American College of Radiology White Paper on Radiation Dose in Medicine. J Am Coll Radiol 2007; 4: 272–284. http://www.acr.org/Secondary-MainMenuCategories/quality_safety/white_paper_dose.aspx (accessed November 10, 2010)
Council Directive 97/43/EURATOM of 30 June 1997 on health protection in individuals against the dangers of ionizing radiation in relation to medical exposure, and repealing Directive 84/466/Euratom. http://ec.europa.eu/energy/nuclear/radioprotection/doc/legislation/9743_en.pdf (accessed January 10, 2011)
Sonnek C, Bauer B. Die neue Röntgenverordnung. Verordnung über den Schutz vor Schäden durch Röntgenstrahlen (Röntgenverordnung RöV) vom 8. Januar 1987 (BGBl. I S 114), zuletzt geändert durch Verordnung vom 18. Juni 2002 (BGBl. I S 1869). Berlin: H. Hoffmann; 2002
History and Clinical Findings
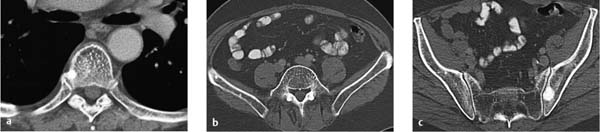
A 63-year-old man had undergone a radical prostatectomy for prostate cancer 10 years earlier. At follow-up he was found to have a serum PSA > 10 μg/mL, which continued to rise in subsequent follow-ups. CT showed multiple sclerotic lesions in the axial skeleton as evidence of osteo-plastic bone metastases (Fig. 6.12). Six days later the patient was referred by urology for radiographic evaluation of the axial skeleton to verify the CT findings (Fig. 6.13).
Fig. 6.12a–c CT. The report described multiple osteoplastic masses consistent with metastases.
Fig. 6.13a–c Representative selection of radiographs. Diagnosis: osteosclerotic metastasis in the left ilium and surgical clips in the lesser pelvis following a prostatectomy.
Further Case Summary
The osteoplastic metastasis in the left ilium close to the sacroiliac joint was visible on the pelvic radiograph (Fig. 6.13). Osteoporosis and spondylosis deformans were noted in the mid and lower lumbar spine as incidental findings.
Error Analysis and Strategy for Error Prevention
The radiographic examinations were not indicated for the following reasons:
 The diagnosis of skeletal metastasis was established by the serum PSA level and abnormal CT findings. Any measurable PSA concentration following a radical pros-tatectomy indicates the continued presence of neo-plastic prostatic tissue, which may signify a local recurrence or lymphogenous or skeletal metastasis. A syn-optic review of the CT, clinical, and laboratory findings should have identified the rounded sclerotic lesions in the cancellous and cortical bone as skeletal metastases (Table 6.1).
The diagnosis of skeletal metastasis was established by the serum PSA level and abnormal CT findings. Any measurable PSA concentration following a radical pros-tatectomy indicates the continued presence of neo-plastic prostatic tissue, which may signify a local recurrence or lymphogenous or skeletal metastasis. A syn-optic review of the CT, clinical, and laboratory findings should have identified the rounded sclerotic lesions in the cancellous and cortical bone as skeletal metastases (Table 6.1).
 All questions relevant to further management (number and volume of the metastases) were answered by the CT examination. Osteoplastic metastases do not jeopardize the stability of the bones.
All questions relevant to further management (number and volume of the metastases) were answered by the CT examination. Osteoplastic metastases do not jeopardize the stability of the bones.
 The spatial and contrast resolution of radiographs is inherently inferior to the spatial and contrast resolution of CT slices due to the projection nature of x-ray films. This explains why the smaller metastases detected by CT (Fig. 6.12) were not visible on the radiographs (Fig. 6.13).
The spatial and contrast resolution of radiographs is inherently inferior to the spatial and contrast resolution of CT slices due to the projection nature of x-ray films. This explains why the smaller metastases detected by CT (Fig. 6.12) were not visible on the radiographs (Fig. 6.13).
The radiographs could have been avoided by applying careful selection criteria in urology and radiology. Any unnecessary imaging leads to needless costs and may provide legal grounds for bodily injury claims. The incidence of unnecessary radiographs varies greatly from one facility to the next and is in the range of 10–40% (see p. 217).
Prostate Cancer
Prostate-Specific Antigen (PSA)
The most important serum marker for prostate cancer is PSA, a glycoprotein produced in the glandular epithelial cells of the prostate. The normal serum level of PSA is less than 4.0 μg/mL. The level may be slightly elevated in benign prostatic hyper-plasia and acute prostatitis. The serum concentration of PSA correlates closely with the mass of PSA-expressing cells. When the levels exceed 10 μg/mL, it should be assumed that prostate cancer is present until proven otherwise. The progression of serum PSA values is just as important as the absolute PSA level. Up to 15% of all prostate cancers do not express PSA. Any measurable PSA concentration after a radical prostatectomy is abnormal and suggests a local tumor recurrence or metastasis.
Serum PSA
 Low: 0–2.5 μg/mL
Low: 0–2.5 μg/mL
 Mildly elevated: 2.6–10.0 μg/mL
Mildly elevated: 2.6–10.0 μg/mL
 Moderately elevated: 10.1–19.9 μg/mL
Moderately elevated: 10.1–19.9 μg/mL
 Markedly elevated: ≥ 20 μg/mL
Markedly elevated: ≥ 20 μg/mL
Skeletal Metastasis of Prostate Cancer
Metastases from prostate cancer affect the bone in approximately 90% of cases. Approximately 80% of these metastases are osteoplastic, 4% are osteolytic, and 16% are mixed. Metastases involve the obturator and pelvic lymph nodes in 60% of cases, the lung in 40%, and the liver in 25%.
References and Further Reading
American College of Radiology (ACR). ACR Appropriateness CriteriaTM. Metastatic bone disease. http://www.acr.org/SecondaryMainMenuCategories/quality_safety/app_criteria/pdf/ExpertPanelonMusculoskeletalImaging/MetastaticBoneDiseaseDoc14.aspx (accessed January 13, 2011)
Greenspan A. Orthopedic Imaging: A Practical Approach. 4th ed. Philadelphia: Lippincott Williams & Wilkins; 2005
Krug B, Wolters U, Stützer H, Lackner K. Inadequacies of repeated radiological examinations in a university hospital. Acta Radiol 2001; 42: 612–61
Krug B, Boettge M, Coburger S, et al. Qualitätskontrolle der ambulanten bildgebenden Diagnostik in Nordrhein-Westfalen, Teil I. RöFo 2003a; 175: 46–57
Krug B, Boettge M, Reineke T, et al. Qualitätskontrolle der ambulanten bildgebenden Diagnostik in Nordrhein-Westfalen, Teil II. RöFo 2003b; 175: 346–360
Walsh PC, Retik AB, Vaughan ED, Wein AJ, eds. Campell’s Urology. Philadelphia: WB Saunders; 2002
Wein JA, Kavoussi LR, Novick AC, Partin AW, Peters CA, eds. Campell-Walsh Urology. 9th ed. New York: Elsevier; 2007
History and Clinical Findings
A 69-year-old man with a hemangioendothelial sarcoma in the left pelvis complained of increasing pain in the left hip region. He was referred for pelvic radiography to evaluate bone stability (Fig. 6.14). The radiographic report described a pathologic fracture of the left acetabulum associated with osteolytic and osteoplastic bone changes.
Fig. 6.14 Pelvic radiograph shows a pathologic fracture of the left acetabulum and mixed osteolytic–osteoplastic changes in the left iliac wing in a patient with a known hemangioendothelial sarcoma.
Further Case Summary
Another pelvic radiograph was taken 4 weeks later for re-staging prior to chemotherapy (Fig. 6.15). When the two images were compared, it was noticed that the “L ap” marker had been placed on the wrong side of the previous radiograph.
Error Analysis and Strategy for Error Prevention
The RT and attending radiologist had failed to notice the misplaced side marker on the initial pelvic radiograph. The examination had been performed with a digital flat-panel detector system in which side labeling is done automatically when the imaging program is selected. The RT remembered that she had turned the patient 180° due to spatial constraints, positioning the patient’s head at the foot of the digital Bucky table. Afterward the image was electronically flipped on the longitudinal body axis, causing the side label to be misplaced. This error went unnoticed until the subsequent restaging radiograph was read.
For accuracy of interpretation and to avoid medicolegal consequences, it is essential that the x-ray film or digital image data set have anatomically correct side labeling.
Fig. 6.15 Pelvic radiograph 4 weeks later. The pathologic fracture of the left acetabulum shows increasing marginal sclerosis. New osteolytic lesions in the right ischium and intertrochanteric zone of the left femur were interpreted as hematogenous metastases.
References and Further Reading
American College of Radiology (ACR). ACR Practice Guideline for Communication of Diagnostic Imaging Findings. http://www.acr.org/SecondaryMainMenuCategories/quality_safety/guidelines/dx/comm_diag_rad.aspx (accessed November 10, 2010)
American College of Radiology (ACR). ACR Practice Guideline for Diagnostic Reference Levels in Medical X-ray Imaging. http://www.acr.org/SecondaryMainMenuCategories/quality_safety/RadSafety/RadiationSafety/guideline-diagnostic-reference.aspx (accessed November 10, 2010)
Amis ES, Butler PF, Applegate KE, et al. American College of Radiology White Paper on Radiation Dose in Medicine. J Am Coll Radiol 2007; 4: 272–284. http://www.acr.org/Secondary-MainMenuCategories/quality_safety/white_paper_dose.aspx (accessed November 10, 2010)
History and Clinical Findings
A 67-year-old woman complained of new pain in the right inguinal region during exertion. Her body weight was 94 kg. She had a history of chronic back pain relating to degenerative spinal changes. She had undergone previous breast-conserving surgery for a ductal carcinoma in situ (DCIS) of the left breast (tumor diameter 0.8 cm).
She had undergone a number of imaging studies at various institutions to investigate her complaints, including radiographs of the lumbar spine, pelvis and right hip (Fig. 6.16
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree