1. Most patients are scheduled for this procedure. If there are any emergencies, discuss the case with the neuroradiology attending staff before sending for the patient.
2. Include the following possible risks and complications on the consent form and have the patient acknowledge appropriate areas: headache; bleeding; infection; seizures; nausea; vomiting; damage to nerves; paralysis; bowel, bladder, and muscle dysfunction; allergic reaction to contrast; and death. If the patient has a clotting disorder or low platelets (platelets need to be at least 50,000 to perform a lumbar puncture), be especially careful. Myelography on anticoagulated patients is usually avoided, if possible.
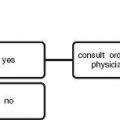
3. Check the patient’s chart for allergies, as well as whether the patient is taking any of the medications that may either lower the seizure threshold (although not an absolute contraindication since the introduction of nonionic hypo-osmolar contrast media). Some physicians will stop these medications before myelography (the risk of seizures is <1%), while some may perform the study without discontinuing such medications. The inserts for iohexol and iopamidol approach this issue in such a way that the decision is left to the physician. We currently do not discontinue these medications prior to myelography. Patients taking platelet inhibitors are at risk for epidural hematoma and subarachnoid hemorrhage from a lumbar or a cervical puncture. Aspirin and Plavix should be discontinued at least 5 days before myelography. (Please note that some aspirin is relative contraindication and always represents a risk vs. benefit situation. For example, if a patient is on aspirin for stroke it is best to continue while it is best not to if aspirin is being taken for a condition such as minor aches). Antiinflammatory drugs with mild platelet inhibition such as ibuprofen are not a contraindication to lumbar puncture. If there is no opportunity to discontinue an antiplatelet medication before myelography, then the user of small-bore needle (22-gauge) is advised.
4. One of the most common problems during a myelogram is a vasovagal reaction, that is, the patient has nausea, sweating, cold clammy appearance, hypotension, and bradycardia. Be prepared to treat it with IV fluids and atropine. In some instances (particularly with young males who seem to have more vasovagal reactions), it is advisable to place an IV line before the myelogram.
5. Usually inject at L2-L3. Remember that the majority of pathology is at L4-L5 or L5-S1 levels. Stay away from higher levels because that is where the conus is located (i.e., T12-L1 or L1-L2). When injecting, use the “puffmethod” and look for the contrast to flow downward with the table angled slightly caudally If there is a question about the injection being sub dural, leave the needle in, do not inject any more media, and call attending staff . A lateral cross-table radiograph will clearly show the position of the needle and of the injected contrast. We always begin with a 22-gauge spinal needle. We use a standard bevel-tip needle, but a blunt-tip needle may also be used.
6. For pediatric patients, talk with attending staff first because general anesthesia is usually used. Find out if the patient has had an MR imaging study first (usually the MR should be done before the myelogram as it almost always answers the majority of questions).
7. All patients have a CT study after the myelogram. Inform the CT technologist what levels need to be scanned based on the findings of the conventional myelogram.
8. Ask women about the possibility of pregnancy. If unsure, get a urine pregnancy test stat.
9. When doing a cervical myelogram from the lumbar route, if you see contrast outlining the basilar artery along the clivus or if the patient complains of headache, tilt the patient back down because contrast media is going up into the head and may induce seizures.
10. Suggested usage of contrast media myelography in adults is shown in the following table.
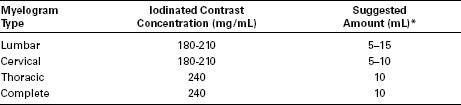
*Total dose of contrast should not exceed 3.0 gm of iodine. For cervical myelograms from a lumbar approach use 10 mL of 300 mg/mL.
11. If a complete myelogram is requested, do the thoracic area last (unless worried about a block, which usually occurs in the upper thoracic area and is encountered when running contrast media up to the cervical area). In cases of suspected spinal cord compression, inject contrast, to rule out cord compression, before removing any CSF. In the presence of a compressive lesion, removal of CSF may worsen the symptoms. However, contrast mixed with CSF does not hinder cytology of this fluid.
12. C1-C2 punctures may be done to outline the superior aspect in a region of cord compression or when lumbar access is not available (e.g., in patients with severe spondylosis). With the patient in a prone position and using cross-table fluoroscopy, a 22-gauge spinal needle is introduced into the posterior third of the spinal canal at the C1-C2 interspace. If the needle is in the subarachnoid space, there is always CSF return. Contrast is injected in order to fill completely the cervical canal. The amount of contrast needed is variable, but it is safe to stop injecting it when it reaches the inferior tip of the clivus.
LUMBAR MYELOGRAMS
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree