Geographic destruction of bone is characteristic • Skull: a bevelled edge to the defect, indicating destruction of the two tables to a differing degree (‘hole within a hole’ sign) • Paediatric spine: thoracic > lumbar > cervical involvement • Flat or long bones: typically diaphyseal involvement with an ill-defined medullary lesion • Unusual features: epiphyseal lesions • The most common lipid storage disorder due to an autosomal recessive genetic enzyme (glucocerebrosidase) deficiency • Infantile form: hepatosplenomegaly, lymphadenopathy, neurological complications, anaemia and haemorrhage • Adult form: hepatosplenomegaly, abdominal pain, ascites, dull bone pain or acute painful crises due to bone infarction (± fever, leucocytosis and a raised ESR) • Cancer of the blood-forming cells of the bone marrow (usually affecting leucocytes)
Myeloproliferative disorders
RETICULOENDOTHELIAL DISORDERS
LANGERHANS CELL HISTIOCYTOSIS
DEFINITION
RADIOLOGICAL FEATURES
Eosinophilic granuloma
XR
 lesions of the hands and feet are rare
lesions of the hands and feet are rare
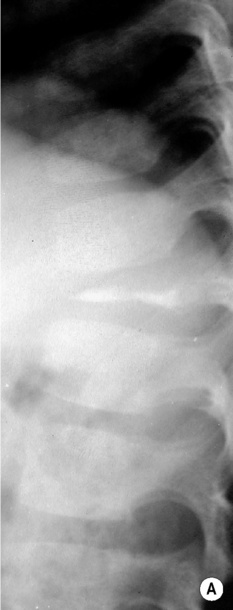
 it classically causes a vertebra plana, with the vertebral body becoming flattened and often wafer-thin
it classically causes a vertebra plana, with the vertebral body becoming flattened and often wafer-thin
 endosteal erosion and a linear periosteal reaction is common
endosteal erosion and a linear periosteal reaction is common
 transphyseal lesions
transphyseal lesions  extracranial ‘button’ sequestra
extracranial ‘button’ sequestra  posterior vertebral arch lesions
posterior vertebral arch lesions
GAUCHER’S DISEASE
DEFINITION
 this leads to accumulation of the lipid glucocerebroside within the lysosomes of monocytes and macrophages of many organs (Gaucher cells)
this leads to accumulation of the lipid glucocerebroside within the lysosomes of monocytes and macrophages of many organs (Gaucher cells)
 death usually occurs at < 2 years of age (mainly due to CNS involvement)
death usually occurs at < 2 years of age (mainly due to CNS involvement)  it mainly affects non-Jews
it mainly affects non-Jews
 many patients are Ashkenazi Jews
many patients are Ashkenazi Jews
WHITE CELL DISORDERS
LEUKAEMIA
DEFINITION
 Acute lymphocytic leukaemia (ALL): this affects adults and children although it is more common in children (65% of paediatric acute leukemias)
Acute lymphocytic leukaemia (ALL): this affects adults and children although it is more common in children (65% of paediatric acute leukemias)
 Acute myeloblastic leukaemia (AML): the most common adult acute leukemia
Acute myeloblastic leukaemia (AML): the most common adult acute leukemia
 Chronic lymphocytic leukaemia (CLL): an adult disorder (predominantly affecting the elderly)
Chronic lymphocytic leukaemia (CLL): an adult disorder (predominantly affecting the elderly)  twice as common as CML
twice as common as CML  characterized by enlargement of the spleen and lymph nodes and rarely skeletal involvement (except as a terminal event)
characterized by enlargement of the spleen and lymph nodes and rarely skeletal involvement (except as a terminal event)![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Myeloproliferative disorders

 it affects children < 2 years of age
it affects children < 2 years of age  splenomegaly, hepatomegaly and lymphadenopathy with anaemia predominate (patients usually die before any bone lesions are identified)
splenomegaly, hepatomegaly and lymphadenopathy with anaemia predominate (patients usually die before any bone lesions are identified)  patients present with fever and a failure to thrive
patients present with fever and a failure to thrive a classical triad of calvarial lesions + exophthalmos (due to bony orbit histiocytosis) + diabetes insipidus
a classical triad of calvarial lesions + exophthalmos (due to bony orbit histiocytosis) + diabetes insipidus benign and self-limiting
benign and self-limiting  80% present before 10 years of age (2M:1F)
80% present before 10 years of age (2M:1F)  multiple lesions in 10% at presentation
multiple lesions in 10% at presentation  pain and local tenderness (± a moderately elevated ESR)
pain and local tenderness (± a moderately elevated ESR)  pathological fractures are rare
pathological fractures are rare long bone metaphyseal and diaphyseal lesions are initially lytic but later heal with periosteal reaction and medullary sclerosis
long bone metaphyseal and diaphyseal lesions are initially lytic but later heal with periosteal reaction and medullary sclerosis  pelvic and vertebral body lesions are common
pelvic and vertebral body lesions are common T1WI: low SI
T1WI: low SI  T2WI/STIR: high SI
T2WI/STIR: high SI  extraosseous involvement in 30%
extraosseous involvement in 30%


 an Erlenmeyer flask deformity (due to loss of normal modelling)
an Erlenmeyer flask deformity (due to loss of normal modelling)  osteosclerosis (due to a healing bone infarct)
osteosclerosis (due to a healing bone infarct)  metaphyseal notching of the humerus (secondary to increased bone turnover) is characteristic
metaphyseal notching of the humerus (secondary to increased bone turnover) is characteristic T1WI: low SI
T1WI: low SI  T2WI: high SI
T2WI: high SI
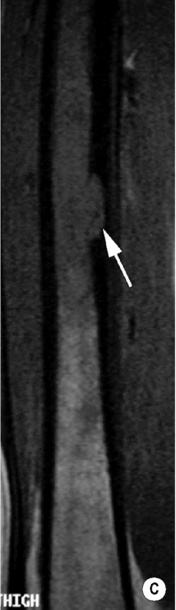
 periosteal reaction
periosteal reaction

 possible cord compression
possible cord compression it resembles Gaucher’s disease but there is deposition of sphingomyelin within foam cells
it resembles Gaucher’s disease but there is deposition of sphingomyelin within foam cells