and Sindu Sheth2
(1)
Department of Radiology, Keck School of Medicine, University of Southern California, Los Angeles, CA, USA
(2)
Keck School of Medicine, University of Southern California, Los Angeles, CA, USA
FDG Viability Scintigraphy
Introduction
Among all methodologies in the diagnosis of hibernating myocardium, 18F-FDG PET has remained a significant diagnostic tool. In combination with myocardial perfusion scintigraphy, FDG PEt allows differentiation between scar and viable myocardium and extent of disease with remarkable certainty. This leads to appropriate patient selection for invasive revascularization procedure. FDG PET has also been helpful in patients with diagnosis of cardiac sarcoidosis and evaluation of patients with cardiomyopathy for resynchronization therapy or who are being considered for revascularization or heart transplant.
Overview
Normal myocardium utilizes free fatty acids or glucose to generate energy. Under aerobic conditions, free fatty acids are the main sources of energy unless there is circulating insulin to facilitate glucose consumption. During severe ischemia (viable), myocardium switches to anaerobic metabolism, utilizing glucose as the sole source of energy. Therefore, 18F-FDG PET will detect an ischemic myocardium (hibernating).
Technique
Perhaps the most important factor in obtaining a quality image is patient preparation. The following protocol has been successfully implemented in our institution.
[18F]-FDG Cardiac Viability Imaging Protocol
Scheduling Considerations
A resting myocardial perfusion study must be obtained within the month prior to the PET scan, and there must be no change in the patient’s clinical status between the perfusion scan and the viability scan.
Patient Preparation
Obtain patient history including allergies, risk factor, diabetes, medication, known cardiovascular therapy, and prior cardiovascular tests (echocardiography, SPECT, MRI, or invasive coronary angiography).
The patient must have a resting myocardial perfusion scintigraphy (thallium, Myoview/MIBI, or rubidium) prior to viability scintigraphy.
Glucose management for diabetic cardiac patients is individually reviewed by the nuclear medicine physician, radiologist, or nurse. However, generally diabetic patients are instructed to eat a high-protein/low-carbohydrate dinner the evening before the scan. Diabetics using oral hypoglycemic agents are asked to take the normal dose of medication and no breakfast the day of the study (early morning schedule).
If the study must be scheduled for the afternoon, the patient is instructed to eat a high-protein/low-carbohydrate light breakfast, take a full dose of morning hypoglycemic agent or insulin, and abstain from eating lunch.
Tube feeding and intravenous dextrose solution must be placed on hold 3–6 h prior to study. Nicotine and caffeine consumption must be held 24 h prior to viability scintigraphy.
Radiopharmaceutical Dosage
Adult dose: 18F-FDG 10–20 mCi IV or 0.22 mCi/kg.
Pediatric dose: adjusted pediatric dose schedule = (0.14–0.21 mCi) [18F] IV not to exceed 10 mCi.
Clinical Imaging Procedure
1.
Height, weight, and blood glucose are measured. An intravenous catheter is placed and left throughout the study.
2.
Cardiac monitoring.
3.
Obtain serum fasting blood glucose (BG).
4.
Glucose is administered PO.
5.
Nondiabetic
Oral glucose loading:
(a) | If BG < or = 150 mg/dl | 50 g oral glucose + regular insulin 3 units IV |
(b) | If BG 151–300 mg/dl | regular insulin 5 units IV |
(c) | If BG 301–400 mg/dl | regular insulin 7 units IV |
(d) | If BG > 400 mg/dl | consult physician |
IV glucose loading (if unable to load PO): see below
FDG administration: After glucose load and sliding scale insulin injections, administer F-18 FDG at least 45 min after glucose loading and when BG < or = 150 mg/dl.
6.
Diabetic
Oral glucose loading:
(a) | If BG < or = 150 mg/dl | 25 g oral glucose |
(b) | If BG 151–180 mg/dl | regular insulin 5 units IV |
(c) | If BG 181–200 mg/dl | regular insulin 7 units IV |
(d) | If BG 201–300 mg/dl | regular insulin 12 units IV |
(e) | If BG > 400 mg/dl | consult physician |
IV glucose loading (if unable to load PO): see below
FDG administration: After glucose load and sliding scale insulin injections, administer F-18 FDG at least 60 min after glucose loading and when BG ≤ 150 mg/dl.
7.
15 min following administration of oral glucose load, obtain blood glucose level and repeat every 15 min and administer IV regular insulin as per above protocol.
8.
Residual activity in the syringe and tubing is assayed and used to determine the actual administered activity.
9.
Following uptake period, the patient is transferred to the imaging table.
10.
The patient is positioned with their arms up (preferred) or at their side. Scout images are acquired to determine position and whether there is adequate FDG uptake in the myocardium.
11.
Routine cardiac imaging should not begin sooner than 40 min post injection. If myocardial uptake is still negligible after 40 min, the nuclear medicine physician must be notified.
12.
The blood glucose level must be >80 mg/dl prior to discharge. The patient will be observed for signs of hypoglycemia during the entire procedure while in the PET center. If blood sugar is ever less than 80 mg/dl after insulin administration, start D5W @ 100 cm3/h IV. Recheck blood glucose in 15 min.
IV Glucose Loading Instruction
(a)
If the fasting glucose level is <150 mg/dl, 25 g dextrose-50 is given intravenously. (20–25 mg of hydrocortisone should be added to the dextrose-50 prior to injection to reduce the irritation of the veins.)
(b)
For fasting glucose levels between 150 and 200, administer 12.5 g dextrose-50 dose.
(c)
For fasting glucose levels >200, implement sliding scale insulin to lower the blood sugar using the following formula:
 Note: Up to 10 units IV per dose (i.e., no single dose greater than 10 units of regular insulin should be given).
Note: Up to 10 units IV per dose (i.e., no single dose greater than 10 units of regular insulin should be given).

(d)
After each insulin dose, blood sugar should be checked 15 min after the dose is given.
(e)
If blood sugar is ever less than 80 mg/dl after insulin administration, start D5W @ 100 cm3/h IV. Recheck blood glucose in 15 min.
(f)
If hypoglycemia occurs (patient becomes diaphoretic, tachycardic, disoriented, etc.), give dextrose-50, 1 ampule IV, and start D5W @ 100 cm3/h IV.
(g)
Insulin is administered by physician or PET nurse only.
(h)
If the blood sugar is = or < 150 mg/dl following sliding scale protocol, FDG can be injected.
(i)
If the blood sugar remains >150 mg/dl, continue sliding scale insulin formula prior to injection of the FDG.
Case 15.1
History
A 57-year-old male with known history of coronary artery disease , status post CABG, was referred for myocardial viability.
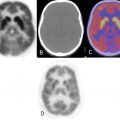
Rows 1 and 3 (short-axis images) demonstrated a large area of perfusion abnormality at rest (SPECT myocardial perfusion scintigraphy—99mTc-tetrofosmin) involving the inferior left ventricular wall (Fig. 15.1). Rows 2 and 4 18F-FDG viability scintigraphy demonstrated a nonviable myocardium.


Fig. 15.1
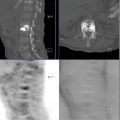
Top row (vertical axis) image resting SPECT myocardial perfusion scintigraphy (99mTc-tetrofosmin) (Fig. 15.2). Bottom row 18F-FDG viability scintigraphy demonstrated no viable myocardium in the inferior wall.


Fig. 15.2
Case 15.2
History
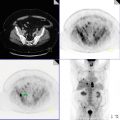
A 72-year-old male with known history of coronary artery disease, status post PTCA stent of RCA, was referred for evaluation of myocardial viability. Image 2 showed a moderate size perfusion abnormality involving inferoseptal left ventricular myocardium. This region demonstrated physiologic activity on FDG scintigraphy, indicating a viable myocardium.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree