Infections of the central nervous system (CNS) can be severe, disabling, and potentially fatal. Infections of the central nervous system (CNS) can be severe, disabling, and potentially fatal. Appropriate recognition of symptoms facilitates expeditious evaluation, prompt diagnosis, and timely treatment. Further work-up may include cranial or spinal imaging, lumbar puncture, and invasive biopsy. Therapy involves antibiotic, antiviral, or antifungal treatment. Surgical treatment for debridement, decompression, or reconstruction may also be required. This review explores the presentation, pathogenesis, evaluation, and treatment of the most common infections of the CNS. Discussion of treatment options also includes possible neurosurgical interventions. The infections considered are cerebral abscess, subdural empyema, meningitis, encephalitis, toxoplasmosis, neurocysticercosis, diskitis, and spinal epidural abscess.
- •
Intracerebral abscesses can rapidly cause severe neurologic deficits or death and require prompt evaluation, imaging, and treatment.
- •
Subdural empyema is an uncommon but potentially life-threatening infection that typically requires prompt surgical decompression, culturing, and antibiotics.
- •
The organisms causing meningitis vary by the age of presentation and require prompt treatment with differing antibiotics.
- •
Herpes simplex encephalitis requires very rapid recognition, diagnosis, and antiviral treatment to prevent severe neurologic deficits or death.
- •
Spinal diskitis and spinal epidural abscess are uncommonly a threat to life but may cause paraplegia or quadriplegia without expeditious evaluation, imaging, and treatment.
Intracerebral abscess
Brain abscess has been one of the most feared CNS infections. This fear arose from the initial poor outcomes and from the rapid neurologic deterioration that can occur. Although rapid deterioration can still occur, the overall outcomes have improved because of improved antibiotics and imaging, which minimize the delay in diagnosis and treatment.
The brain parenchyma is not prone to parenchymal abscess formation, whereas other events and risk factors are required to set the stage for abscess formation. Inoculation can occur from direct implantation (such as a bullet entering the brain or after neurosurgery) or contiguous spread (such as from adjacent sinusitis or mastoiditis). Most commonly, however, infection elsewhere spreads hematogenously to the CNS. A classic example is bacterial endocarditis with septic emboli to the brain resulting in cerebral abscess formation. Other common primary sites include dental abscesses, cutaneous abscesses, urinary tract infection, pulmonary infection, and soft tissue infection.
Several conditions can predispose to cerebral abscess formation. Systemic immunosuppression is frequently involved. Immunosuppression can occur because of intentional immunosuppression (eg, to prevent organ transplant rejection), immune system destruction (eg, with human immunodeficiency virus [HIV] and AIDS), or other medications that affect the immune system (eg, corticosteroids and chemotherapy agents). Pulmonary arteriovenous malformations, with or without Osler-Weber-Rendu syndrome, and congenital cyanotic heart malformations are also thought to be risk factors.
Intracerebral abscesses can rapidly cause severe neurologic deficits or death and require prompt evaluation, imaging, and treatment.
Abscess development occurs in a 3-step process. The early cerebritis phase is marked by an area of poorly demarcated inflammation. The late cerebritis phase is marked by the migration of fibroblasts, which start depositing reticulin. In addition, necrosis begins to appear centrally. The early capsule (abscess) stage is marked by the migration of additional fibroblasts and generation of more reticulin in an attempt to wall off an increasing amount of central necrosis. The late capsule stage is marked by a mature collagen capsule surrounding the central necrotic zone.
The microbiology typically reflects the pathogens from the primary site that seeded the CNS. Therefore, gram-positive cocci (GPC) predominate after intravascular infection. Infections beginning from the urinary tract are more frequently gram-negative rods (GNR). Postsurgical and penetrating injuries typically result in skin-related pathogens—mostly GPC. Abscesses resulting from contiguous sinus spread often may harbor more anaerobic organisms, whereas dental abscesses give rise to polymicrobial or anaerobic cerebral abscess pathogens.
Patients present with a myriad of possible symptoms. The most common symptoms are headache, fever, nausea and vomiting, focal neurologic deficits, abnormal sensorium, and decreased level of consciousness.
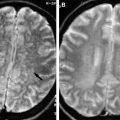
Treatment of brain abscess requires accurate microbiological diagnosis and appropriate antibiotic therapy. If a patient is not neurologically deteriorating, has no or minimal deficits; and if a microbiological diagnosis can be obtained from another location, antibiotic therapy may be prescribed without a neurosurgical procedure. This strategy does require high quality diagnostic imaging to characterize the lesions initially and during follow-up. If the lesions respond to antibiotics by decreasing in size and ultimately resolution, then no neurosurgical procedures are required. If the lesions grow, then biopsy and drainage may be required. Stereotactic biopsy and needle drainage is required when abscess is strongly suspected but no primary sites can be identified to culture and when there is a large lesion or lesions causing mass effect and significant neurologic deficits. Craniotomy for resection of abscess is another surgical alternative if needle drainage is not successful.
The prognosis is related to the initial presentation, response to antibiotic therapy, and any systemic conditions or risk factors that may hinder innate immunologic attempts to clear the infection. Recent mortality ranges from 5 to 50. Patients with no risk factors and stereotactic aspiration had 5% mortality whereas those with several risk factors had 50% mortality. Negative prognostic factors include worse functional status at presentation, immunocompromise, and older age.
Subdural empyema
Subdural empyema (SDE) is a very serious but uncommon CNS infection. An empyema is a localized purulent infection in an actual cavity or a potential space. In SDE, the empyema occurs in the subdural space. Several mechanisms explain the development of SDE. SDE can occur as a complication of meningitis, after craniotomy, and as a result of extension of paranasal sinus infections or otitis media.
Subdural empyema is an uncommon but potentially life-threatening infection that typically requires prompt surgical decompression, culturing, and antibiotics.
Patients with SDE present with headache, significant neurologic deficits, seizures, decreased level of consciousness, and fever. Empyema can compress the brain focally to cause focal deficits. SDE can cause significant inflammation in the subjacent cortex to cause seizures. If the mass effect, inflammation, and edema are significant enough, midline shift, herniation, and global decline can occur.
The range of microbiological diagnoses is different from that of intracerebral abscess and meningitis because of the direct extension from the paranasal sinuses or mastoid. Gram-negative organisms are frequently reported to predominate. In contrast, cultures from postsurgical SDE usually are dominated by gram-positive species.
Surgical treatment must address 3 issues. The first issue is accurate microbiological diagnosis. On occasion this may be obtained from a primary site such as the paranasal sinuses or mastoid. If no other active site is identified, neurosurgical intervention is required. The second issue is CNS mass effect. Mass effect, midline shift, and parenchymal displacement typically call for surgical intervention. Very significant mass effect and cerebral edema may require craniotomy or craniectomy for decompression and debridement. The third and final issue is the possibility of surgical treatment for purulent loculations that may be too large for antibiotics alone to treat. In such situations, it may be possible to culture, aspirate purulent material, and irrigate the subdural space with antibiotic solution through burr holes.
The prognosis is guarded with SDE. These patients are very ill, both systemically and neurologically. They require close multidisciplinary management among the neurosurgical, infectious disease, and critical care teams. Tsai and colleagues reported 11 of 15 patients having good outcomes (normal to moderate disability) and 4 of 15 patients having poor outcomes (severe disability to death). Hlavin and colleagues reported a mortality rate of 18.5% and an additional 18.5% survived with neurologic morbidity. They also found advanced age and more significant encephalopathy at presentation to portend a worse prognosis as well.
Subdural empyema
Subdural empyema (SDE) is a very serious but uncommon CNS infection. An empyema is a localized purulent infection in an actual cavity or a potential space. In SDE, the empyema occurs in the subdural space. Several mechanisms explain the development of SDE. SDE can occur as a complication of meningitis, after craniotomy, and as a result of extension of paranasal sinus infections or otitis media.
Subdural empyema is an uncommon but potentially life-threatening infection that typically requires prompt surgical decompression, culturing, and antibiotics.
Patients with SDE present with headache, significant neurologic deficits, seizures, decreased level of consciousness, and fever. Empyema can compress the brain focally to cause focal deficits. SDE can cause significant inflammation in the subjacent cortex to cause seizures. If the mass effect, inflammation, and edema are significant enough, midline shift, herniation, and global decline can occur.
The range of microbiological diagnoses is different from that of intracerebral abscess and meningitis because of the direct extension from the paranasal sinuses or mastoid. Gram-negative organisms are frequently reported to predominate. In contrast, cultures from postsurgical SDE usually are dominated by gram-positive species.
Surgical treatment must address 3 issues. The first issue is accurate microbiological diagnosis. On occasion this may be obtained from a primary site such as the paranasal sinuses or mastoid. If no other active site is identified, neurosurgical intervention is required. The second issue is CNS mass effect. Mass effect, midline shift, and parenchymal displacement typically call for surgical intervention. Very significant mass effect and cerebral edema may require craniotomy or craniectomy for decompression and debridement. The third and final issue is the possibility of surgical treatment for purulent loculations that may be too large for antibiotics alone to treat. In such situations, it may be possible to culture, aspirate purulent material, and irrigate the subdural space with antibiotic solution through burr holes.
The prognosis is guarded with SDE. These patients are very ill, both systemically and neurologically. They require close multidisciplinary management among the neurosurgical, infectious disease, and critical care teams. Tsai and colleagues reported 11 of 15 patients having good outcomes (normal to moderate disability) and 4 of 15 patients having poor outcomes (severe disability to death). Hlavin and colleagues reported a mortality rate of 18.5% and an additional 18.5% survived with neurologic morbidity. They also found advanced age and more significant encephalopathy at presentation to portend a worse prognosis as well.
Meningitis
Meningitis is one of the most common CNS infections, with an incidence of 3.67 to 12.5/100,000 patients. Meningitis is an infection of the cerebrospinal fluid (CSF) and the meningeal layer surrounding the brain. The infection can involve the cerebral ventricles to cause ventriculitis.
The organisms causing meningitis vary by the age of presentation and require prompt treatment with differing antibiotics.
Meningitis is most frequently treated by neurologists, pediatricians, and infectious disease specialists. However, it is crucial for all physicians to understand and recognize meningitis because meningitis is generally very treatable when promptly diagnosed and treated, whereas meningitis can be devastating if diagnosis and treatment are delayed.
Meningitis presents most commonly with headache, fever, and nuchal rigidity. Other symptoms include seizures and cranial nerve deficits. Loss of consciousness can occur from seizures, inflammation and cerebral edema, or hydrocephalus. Herniation can occur and cause coma and death.
The pathogenesis and range of responsible microbes differ with age groups. Neonatal meningitis occurs due to exposure to pathogens during delivery, particularly with vaginal delivery. Pathogens include Escherichia coli , group B streptococci, and Listeria. Children aged 3 months to 5 years are predominantly affected by Streptococcus pneumoniae and Neisseria meningitidis (meningococcus). Pneumococcus is a colonizer of the nasopharynx that is transmitted via respiratory droplets and secretions. From the nasopharynx, it can spread to cause meningitis. A 7-valent pneumococcal vaccine was licensed for use in the United States which resulted in a decrease in childhood pneumococcal meningitis incidence and mortality. Meningococci are gram-negative commensal bacteria that colonize the nasopharynx. Transmission also occurs through respiratory droplets and secretions. Once colonization has occurred, meningococci can then progress to meningitis, which has a very fulminant and rapid course. This fact makes vaccination strategies much more attractive to prevent meningococcal meningitis. A quadrivalent meningococcal vaccine was licensed for use in 2005, and monitoring is ongoing to assess the decrease in meningococcal meningitis incidence. Haemophilus influenzae type b previously was an important species in this age group; however, routine childhood immunization (Hib) begun in the early 1990’s has reduced the incidence of H influenzae meningitis nearly to 0. Patients aged 5 years–50 years continue to experience meningitis caused predominantly by S pneumoniae and meningococci. Spread is facilitated among people living in close quarters, such as dormitories. Patients older than 50 years experience S pneumoniae and meningococcal infections; however, Listeria and gram-negative enteric organisms can also be causative.
The treatment of meningitis requires prompt diagnosis and antibiotic administration. If there is any suspicion about the possible presence of meningitis, especially if a patient is experiencing significant symptoms, a first dose of broad-spectrum antibiotics should be given. The mainstay of diagnosis is the lumbar puncture (LP). Gram’s stain and cell count with differential, total protein, and glucose are recommended. Again, antibiotic administration is begun without waiting for these results if concern of meningitis is present.
Neurosurgical intervention is required if hydrocephalus is present. In the setting of meningitis, a ventriculostomy would be placed for ventricular drainage while the infection is treated. Once treated, it may be possible to wean the drainage if the normal CSF outflow can resume. If the normal CSF outflow does not re-establish itself, ventriculoperitoneal shunt placement is likely required.
Heroic measures such as craniectomies, either supratentorially or in the posterior fossa in the case of trans-foramen magnum herniation are sometimes recommended in severe cases. These procedures are more likely to be considered when the deterioration has been very abrupt, observed, brought rapidly to medical attention, and the patient is already in the hospital so that surgery can be rapidly undertaken. When rapid devastating deficits develop before the patient presents in hospital, the time involved in transport, evaluation, transport to operating room, set-up, and start, even when rapidly undertaken, rarely occurs quickly enough to reverse neurologic devastation.
Prognosis for patients with meningitis is variable. Rapid diagnosis and initiation of antibiotics is crucial to improving outcomes; Køster-Rasmussen and colleagues demonstrated a 30% increase in odds of unfavorable outcome per hour of delay before antibiotic administration. Recent mortality ranges from 13% to 18.7%. Neonates, the elderly, the immunocompromised, and those presenting with significant neurologic deficits suffer higher mortality rates. Major morbidities occurred in 12.8% of cases and minor morbidities occurred in 8.6% of cases. The most common morbidities were hearing loss (33.6%), seizures (12.6%), and motor deficits (11.6%).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree