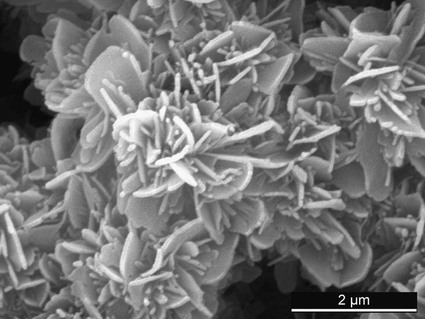
Osteoporosis has become a major health problem for most Western societies in recent decades. Strongly osteoporotic bone is so brittle, any move can result in bone fracture. In 1995, 1.5 million fractures in the United States were attributable to osteoporosis.1 In 2000, 200,000 vertebral fractures were estimated to occur every year among the female U.S. population.2 Even though these fractures are rather benign, they are associated with high morbidity and long hospital stays.3 Repairing osteoporotic fractures with traditional osteosynthesis techniques is often very difficult owing to the inherent weakness of bone. The introduction of screw-locking osteosynthesis plates has improved therapy, but not for all indications. Therefore, new techniques should be proposed, investigated, and introduced. One approach to heal or at least handle osteoporotic bone fractures is to inject a cementing bone substitute into bone. This technique, called bone augmentation, is particularly useful for vertebral fractures (the procedure is often called vertebroplasty [see Chapter 159]).4 Unfortunately, dramatic negative outcomes of spine augmentation procedures have been reported in recent years.5,6 Even though the cause of these negative results is in most cases associated with poor clinical practice, inadequate cement properties are also mentioned.6 Therefore, the cement properties required by the given application should be well understood to design more adequate cements. The goal of this chapter is to review the present knowledge on cements designed for bone augmentation. Exclusively bone cements developed for bone augmentation procedures should be used in vertebroplasty/kyphoplasty. Modifications of commercial cements that are often mentioned in leading publications7,8 are prohibited, and hence the use of modified cements should be carefully weighed and discussed with the patient.9 The first cement that was used for a bone augmentation procedure was a PMMA cement.4 This cement consists of several ingredients that all have their importance10: • A monomer called methyl methacrylate (MMA; transparent liquid; Mw = 100 g/mole) that will eventually react to form PMMA. The heat released by the latter reaction is very large (i.e., close to 57 kJ/mole), whereas the specific heat of PMMA is relatively low (i.e., close to 0.146 kJ/[mole·K]).11 As a result, the heat released during the reaction is large enough to potentially heat up the cement by several hundred degrees during setting. • A PMMA powder (or copolymers) used as a filler material, hence decreasing the total heat released per cement volume, as well as reducing shrinkage during setting (21% for pure MMA) • A radiopacifier to ensure the cement can be seen radiographically (radiopacifier included in or added to PMMA powder). Typical powders are BaSO4 and ZrO2. • Additives to initiate the polymerization reaction, commonly dibenzoyl peroxide (generally included in or added to PMMA powder) and N,N-dimethyl-p-toluidine (generally included in the liquid phase) • Other additives such as stabilizers, inhibitors, radical catchers, coloring agents, antibiotics In commercial formulations, the ratio between powder and liquid component is typically close to 2 : 3. Additionally, the radiopacifier content can easily reach 30%. For example, the powder component of Osteopal V (Heraeus Kulzer [see Table 160-1]) contains 14.16 g PMMA (40.0 w% of the total cement weight), 11.70 g ZrO2 (33.1 w%), 0.14 g benzoyl peroxide (0.4 w%), and chlorophyll (coloring agent), and the liquid component contains 9.2 g MMA (26 w%), 0.19 g N,N-dimethyl-p-toluidine (0.5%), and chlorophyll. Since the MMA content is relatively small, shrinkage and volume heat release of commercial cement formulations are much lower than those of pure MMA cement. TABLE 160-1 List of PMMA Cements with 510(k) FDA Clearance for Vertebroplasty FDA, U.S. Food and Drug Administration; PMMA, polymethyl methacrylate. *Device listed under the category “Polymethyl methacrylate (PMMA) bone cement” that does not appear to refer to a cement. (From Bohner M: Uebersicht über einspritzbare Zemente für die Vertebroplastie und die Kyphoplastie. IN Becker S, Ogon M (eds): Ballonkyphoplastie. Springer-Verlag: Wien, 2006. Used with kind permission from Springer Science+Business Media.) In the early days of vertebroplasty, PMMA cements were modified to better fulfill the requirements of the application. In particular, the powder-to-liquid ratio was reduced to prolong the injection period, and more radiopacifier was added to increase radiologic contrast.7,8 These changes considerably modified cement properties such as viscosity, setting time, monomer release, and mechanical properties. There was no cement accepted for vertebral bone augmentation procedures, so these changes were required, but at the clinician’s and patient’s risk. Nowadays there are cements designed specifically for the application (Table 160-1), and their use is recommended. CPCs were discovered in the early 1980s by LeGeros12 and Brown and Chow.13 Since then, CPCs have proved to be attractive bone-substitute materials.14 The first in vitro attempt to use CPC for the augmentation of osteoporotic bone was performed in 1991.15 A few years later, the first in vitro use for intravertebral reconstruction was proposed.16 To our knowledge, there is presently no CPC cleared by the U.S. Food and Drug Administration (FDA) for vertebroplasty applications, despite the fact that their clinical use has been described in the literature.17–20 CPCs generally consist of an aqueous solution and a powder that typically contains several calcium phosphate compounds. Upon mixing, the powder dissolves in the aqueous solution, and new crystals form (precipitate). The reaction proceeds until all reactive calcium phosphate compounds have reacted. Cement hardening occurs with the entanglement of calcium phosphate crystals (Fig. 160-1), leading to a highly porous structure. The final product has a porosity close to 40% to 60%, with pores ranging typically from 0.1 to 10 µm. It is worth noting that CPCs are mechanically much stronger in compression than in tension or shear because the entangled crystals are not well bonded. Compressive strength is typically 5 to 10 times greater than tensile strength. The two principal CPC types are apatite (e.g., hydroxyapatite, Ca5[PO4]3[OH]) and brushite (also called dicalcium phosphate dihydrate, CaHPO4·2H2O), depending on the end product of the setting reaction.21,22 Most commercially available CPCs belong to the first category (e.g., α-BSM, Biopex, BoneSource, Calcibon, Cementek, Embarc, Kyphos, Mimix, Norian, Rebone (see list in Bohner23). In the past years, a few brushite CPCs have been used clinically: chronOS Inject, JectOS, Eurobone, and VitalOS.23 The main difference between apatite and brushite CPCs lies in their solubility and hence resorption rate: brushite is much more soluble than apatite, so brushite CPC is in principle more rapidly resorbable than apatite CPC. Because CPCs are the main candidates to replace PMMA in vertebroplasty, it is of interest to describe the primary differences between the two cements. Some very important differences are noteworthy (Table 160-2), and four of these will be described. First, PMMA cements are hydrophobic, whereas CPCs are hydrophilic, so the setting reaction of PMMA is barely affected by body fluids. This is in contrast to CPCs, where cement disintegration might occur, leading to the release of very large numbers of micro- and nanoparticles in the close environment of the cement and into blood. Second, the setting reaction occurs much faster in PMMA cements than in CPCs. As a result, reaction heat is released much faster from PMMA cements than from CPCs, leading to a much larger temperature increase in the former. So, even though CPCs are sometimes as exothermic as PMMA, they can be considered to set isothermally. Third, CPCs are very fragile materials. In particular, their shear and tensile properties are much lower than those of PMMA cements. As a result, clinicians are advised to use CPCs in simple/stable spinal fractures17,24 or not to use them at all.18 Fourth, CPCs are resorbable, contrary to PMMA cements, and should be replaced by bone and not simply resorbed. Presently, it is not clear how fast CPCs resorb and how much bone forms after CPC resorption in osteoporotic patients.
New Directions in Bone Materials
Clinical Relevance
Indications
Polymethyl Methacrylate Cements
Device Name
Applicant
BonOs Inject
AAP Biomaterials GmbH
Symphony VR Radiopaque Bone Cement
Advanced Biomaterial Systems
Parallax Acrylic Resin with TRACERS
NeuroTherm
Parallax Acrylic Resin with TRACERS-Ta
NeuroTherm
Parallax Acrylic Resin cartridge with TRACERS
NeuroTherm
Parallax Acrylic Resin cartridge with TRACERS-Ta
NeuroTherm
Parallax contour vertebral augmentation device*
NeuroTherm
ArthroCare Parallax contour vertebral augmentation device*
NeuroTherm
Radiopaque Bone Cement
Cardinal Health
AVAflex vertebral augmentation needle*
Cardinal Health
Inflatable bone tamp*
Cardinal Health
AVAmax vertebral balloon model*
CareFusion
AVAmax vertebral balloon*
CareFusion
Vertefix Vertebroplasty Procedure Set
Cook Medical
Modification to Vertebroplastic Radiopaque Bone Cement
DePuy Spine
Vertebroplastic Radiopaque Bone Cement
DePuy Spine
Space CPSXL Bone Cement
DFine Inc.
Space 360 delivery system*
DFine Inc.
Modification to Space CPSXL Bone Cement
DFine Inc.
Stabili ERX Bone Cement
DFine Inc.
Confidence High Viscosity Bone Cement
DePuy Spine
Confidence Ex High Viscosity Bone Cement
DePuy Spine
Confidence Fenestrated Introducer Needle*
DePuy Spine
Mesh Fenestrated Introducer Needle*
DePuy Spine
EBI Vertebroplasty Systems
EBI L.P.
KyphX HV-R
Kyphon
KyphX HV-R Bone Cement
Kyphon
Kyphon XPEDE Bone Cement
Medtronic
KyphX HV-R Bone Cement
Medtronic
Arcuate Vertebral Augmentation System
Medtronic Sofamor Danek
Cortoss Bone Augmentation Material
Orthovita Inc.
Skeltex ISV
Skeltex Technologies Inc.
StaXx FX System
Spine Wave
Stryker VertaPlex Radiopaque Bone Cement
Stryker Corp.
VertaPlex HV
Stryker Corp.
IVAS 2-10 mm (10 gauge) Balloon Catheter*
Stryker Corp.
Mendec Spine
Tecres Medical
Kit Mendec Spine and Delivery System*
Tecres Medical
VSPSPN
Tecres Medical
Spine-Fix Biomimetic Bone Cement
Teknimed
Opacity + Bone Cement
Teknimed
Vertecem
Teknimed
F20
Teknimed
Cohesion Bone Cement
Teknimed
Calcium Phosphate Cements
Difference Between PMMA and CPC