This article discusses anatomic relationships, anatomic variants, and MRI protocols that pertain to the foot and ankle. MR images with detailed anatomic description form the cornerstone of this article. The superb image quality will facilitate learning normal imaging anatomy, as well as conceptualizing spatial relationships of anatomic structures.
Radiologic evaluation of the foot and ankle is often a complex task given the relatively small size of structures, detailed intricacy of anatomy, multifaceted relationships and mechanism of the anatomic structures, and wide range of pathologic entities. In addition to a proper clinical examination, imaging is routinely used for a complete evaluation of the foot and ankle. In fact, a multimodality approach is often necessary for complete radiologic assessment. Radiography, sonography, and computed tomography all play important roles in the radiologic assessment of the foot and ankle. However, magnetic resonance imaging (MRI) is often the imaging modality of choice attributable to the superior soft tissue contrast resolution, multiplanar capability, lack of ionizing radiation, and ability to do postcontrast imaging.
The keys to optimizing MRI evaluation of the foot and ankle include: obtaining good MR images in ideal imaging planes, understanding the anatomy and relationship of the anatomic structures, and learning the more and less common pathologic entities that may affect this region. Careful attention should also be given to avoid misinterpretation or diagnostic pitfalls by understanding the appearance and significance of anatomic variants.
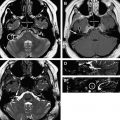
This article discusses anatomic relationships, anatomic variants, and MRI protocols that pertain to the foot and ankle. MR images with detailed anatomic description form the cornerstone of this article. The superb image quality will facilitate learning normal imaging anatomy, as well as conceptualizing spatial relationships of anatomic structures. MRI of a healthy volunteer was performed on a 3 Tesla magnet (Siemens Medical, Erlangen, Germany). Representative images of normal anatomy are depicted primarily using a T1 weighted sequence in the axial (short axis) plane for the ankle and the coronal (short axis) plane for the foot.
Protocol
Obtaining MR images in ideal planes using specific sequences is crucial for the evaluation of anatomy and assessment of pathology. Obtaining MR images in ideal planes using specific sequences is crucial for the evaluation of anatomy and assessment of pathology. In the foot and ankle particularly, musculoskeletal MRI technique is as important as understanding the complex anatomy. The wide range of possible pathologies that can affect this region necessitates the availability and understanding of various imaging protocols.
Several factors may contribute to the selection and customization of the appropriate MRI protocol. Of all the possible factors, the indication for the examination is the most critical. Communication with the ordering physician, the MRI technologist, and the patient is important for designing an appropriate MRI protocol. Additionally, reviewing prior imaging and medical records can often be instrumental. Other factors that should be considered include the patient’s clinical status, ability to cooperate with the MRI examination, availability of specific MRI coils, and availability of higher field strength magnets.
Due to the complex anatomy and wide range of possible pathology, MRI of the foot and ankle can be performed and customized with various imaging planes using a variety of imaging sequences. The authors protocol cases of the foot and ankle based primarily on the clinical indication. Typically, 1 of 3 anatomic regions of interest is selected: ankle/hindfoot, hindfoot/midfoot, or midfoot/forefoot. Six standard imaging planes and sequences are used regardless of the indication for nonarthrogram examinations including T1 nonfat-suppressed in axial, sagittal, and coronal planes, T2 fat-suppressed short axis, short tau inversion recovery (STIR) sagittal, and intermediate proton density long axis. The terms short axis and long axis are routinely used at the authors’ institution to avoid any discrepancy, which can occur with the terms coronal and axial when discussing the foot and ankle. Standard field of view (FOV) of 14 cm or smaller is routinely used for the ankle. Standard FOV of 12 cm or smaller is routinely used for the foot. Smaller fields of view are often used to improve spatial resolution and anatomic detail, while remaining large enough to also allow for an adjacent control structure or anatomic reference point. Indications for a routine ankle protocol include, but are not limited to, ligament injury, tendon pathology, impingement, plantar fasciitis, os trigonum or sinus tarsi syndrome, occult fracture, osteochondral defect, or osteonecrosis. Indications for routine foot protocols (with attention to either the forefoot or hindfoot and including the midfoot) include ligament injury, tendon pathology, plantar fasciitis, plantar plate injury, occult fracture, degenerative disease, osteonecrosis, or Lisfranc joint or ligament instability.
In addition to demonstrating exquisite anatomic detail, the T1 non-fat-saturation (NFS) sequences are useful for the evaluation of a radiographically occult fracture, or for focal or regional bone marrow signal abnormality that may relate to edema or possibly a marrow replacing process. Abnormalities detected on the T1 NFS sequences can then be compared with the T2 FS sequence to assess for fat-containing lesions such as an intraosseous lipoma, bone marrow edema, or replacement of normal fat signal within the sinus tarsi. T2 FS sequence in the axial plane also demonstrates excellent anatomic detail, while suppressing fat signal and accentuating fluid and bone marrow edema. Although time-consuming, STIR provides the most uniform fat suppression and is not subject to the heterogeneous effect observed on T2 FS sequences. In addition, the STIR sequence is useful in limiting susceptibility artifact related to adjacent metallic hardware.
Intravenous gadolinium contrast is typically used for cases involving mass or infection. Specific etiologies more commonly encountered in the foot and ankle requiring contrast-enhanced sequences include cellulitis, abscess, osteomyelitis, plantar fibroma, Morton neuroma, differentiating a solid from a cystic mass, or a synovial inflammatory processes (ie, rheumatoid or reactive arthritis). Gadolinium highlights the soft tissue changes seen in cellulitis as well as the bone marrow changes seen in osteomyelitis. However, contrast is not essential for the diagnosis of either. Enhancement of a Morton neuroma may help to distinguish it from intermetatarsal bursitis or a ganglion cyst; however, anatomic location is a more reliable characteristic. Contrast enhancement patterns help to differentiate a solid from a cystic mass. Lastly, gadolinium will accentuate thickened and inflamed synovial tissue. If contrast is indicated, T1 FS short-axis precontrast and 3 planes of T1 FS postcontrast imaging are added to the routine sequences.
Direct (intra-articular) MRI arthrogram studies are infrequently ordered by referring clinicians, but may be considered in specific clinical settings. Typical indications include assessment of intra-articular bodies, articular cartilage injuries, osteochondral defects, and postoperative cases in the setting of microfracture surgery or osteochondral implantation. Evaluation of the foot and ankle with direct MR arthrography primarily uses T1 FS imaging sequences secondary to the T1 shortening characteristics of gadolinium.
Sample protocols are presented ( Tables 1 and 2 ) from the authors’ institution using a 3 Tesla Siemens MRI machine (Erlangen, Germany). The parameters shown are used as a basic guideline, but are routinely optimized for patient specific factors such as area of interest, patient size, and time restrictions. These parameters will also vary widely with magnetic field strength (ie, 3T vs 1.5 T), as well as the specific make of the MRI machine.
| Sequence# | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| Sequence | T1NFS | T2 FS | STIR | Int PDFS | T1NFS | T1NFS | T1FS Pre | T1FS Post |
| Plane | Axial | Axial | Sagittal | Coronal | Sagittal | Coronal | axial | 3 planes |
| TR/TI (mc) | 780 | 7000 | 7380/ 130 | 3500 | 860 | 700 | 650 | 450–650 |
| TE (mc) | 10 | 70 | 35 | 55 | 10 | 10 | 10 | 10 |
| Slice thickness (mm)/gap | 3/30 | 3/30 | 3/30 | 3/30 | 3/30 | 3/30 | 3/20 | 3/20 |
| FOV (cm) | 14 × 9 | 14 × 9 | 17 × 10 | 19 × 8 | 17 × 10 | 19 × 8 | 14 × 9 | 14 × 9 |
| Matrix | 232 × 256 | 232 × 256 | 232 × 256 | 204 × 256 | 256 × 256 | 204 × 256 | 259 × 320 | 259 × 320 |
| Contrast | No | No | No | No | No | No | No | Yes |
| Sequence# | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| Sequence | T1NFS | T2FS | STIR | Int PDFS | T1NFS | T1NFS | T1FS Pre | T1FS Post |
| Plane | Short axis (cor) | Short axis (cor) | sagittal | Long axis (axial) | Long axis (axial) | sagittal | short axis (cor) | 3 planes |
| TR/TI (mc) | 750 | 5000 | 7300/ 130 | 3500 | 750 | 750 | 650 | 450–650 |
| TE (mc) | 10 | 80 | 30 | 55 | 10 | 10 | 10 | 10 |
| Slice thickness (mm) | 3/30 | 3/30 | 3/30 | 3/30 | 3/30 | 3/30 | 3/20 | 3/20 |
| FOV (cm) | Smallest possible (<12) | Smallest possible (<12) | Smallest possible (<12) | Smallest possible (<12) | Smallest possible (<12) | Smallest possible (<12) | Smallest possible (<12) | Smallest possible (<12) |
| Matrix | 256 × 256 | 180 × 256 | 230 × 384 | 152 × 256 | 256 × 256 | 180 × 256 | 259 × 320 | 259 × 320 |
| Contrast | No | No | No | No | No | No | No | Yes |
Performing the examination
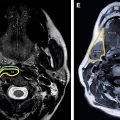
At the authors’ institution, MRI arthrograms and the majority of the conventional MRI examinations are performed on a 3 Tesla MRI magnet. MRI of the foot and ankle is performed with the patient in a supine position, feet first, with the foot 90° to the lower leg. A standard smokestack foot and ankle coil ( Fig. 1 ) is used, and the foot and ankle of interest are centered within the bore. Additional support is placed around the toes for immobilization purposes if necessary. Vitamin E markers may be placed outlining the region of interest as directed by the referring physician or patient. An initial localizer sequence is performed. MRI planes are then selected from the localizer images to identify 3 conventional anatomic planes including short axis, long axis, and sagittal (see Fig. 1 ), allowing the anatomy to be most easily be understood and consistently reproduced.

Performing the examination
At the authors’ institution, MRI arthrograms and the majority of the conventional MRI examinations are performed on a 3 Tesla MRI magnet. MRI of the foot and ankle is performed with the patient in a supine position, feet first, with the foot 90° to the lower leg. A standard smokestack foot and ankle coil ( Fig. 1 ) is used, and the foot and ankle of interest are centered within the bore. Additional support is placed around the toes for immobilization purposes if necessary. Vitamin E markers may be placed outlining the region of interest as directed by the referring physician or patient. An initial localizer sequence is performed. MRI planes are then selected from the localizer images to identify 3 conventional anatomic planes including short axis, long axis, and sagittal (see Fig. 1 ), allowing the anatomy to be most easily be understood and consistently reproduced.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree