Magnetic resonance (MR) imaging is the preferred imaging modality for evaluating internal derangement of the knee, due to its superior soft tissue contrast resolution, multiplanar imaging capability, and lack of ionizing radiation. The superb image quality facilitates learning of normal imaging anatomy and conceptualizing spatial relationships of anatomic structures, leading to improved understanding of pathologic processes, mechanisms of injury, and injury patterns, and ultimately increased diagnostic accuracy. This article depicts normal MR imaging anatomy and commonly encountered anatomic variants using representative MR images of the knee, and describes and explains the rationale of routine knee MR imaging protocol.
There are several keys to successfully interpreting MR imaging examinations. Initially, constructing a solid foundation consisting of a good understanding of basic MR imaging principles and imaging protocols as well as the appearance of normal imaging anatomy is crucial. This knowledge can be then applied to one’s understanding of pathology commonly encountered in the area of interest. Careful attention should be focused on awareness of commonly encountered normal variants and diagnostic pitfalls to improve accuracy and avoid misinterpretation. In this article, MR imaging of a healthy volunteer was performed on a 3-T MR imaging unit (Siemens, Munich, Germany). Normal anatomy is depicted at representative levels throughout the knee, and descriptions of frequently encountered anatomic variants are provided.
Protocols
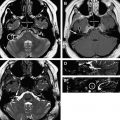
At the authors’ institution, a combination of intermediate-weighted proton density (PD) and T2-weighted fast spin echo sequences with and without fat suppression are used to provide excellent anatomic detail and localize pathology. Fat suppression accentuates bone marrow and soft tissue edema on fluid-sensitive sequences, and non–fat-suppressed images increase conspicuity of bone marrow abnormalities on short echo time (TE) sequences. Furthermore, fast spin echo PD sequences employing fat saturation are accurate and sensitive for evaluation of meniscal tears and articular cartilage disruption.
In general, optimal evaluation is achieved when the imaging planes are oriented perpendicular to and parallel to the long axis of the structure in question. The multiplanar capability of MR imaging allows for oblique sagittal image acquisition oriented parallel to the lateral femoral condyle, which optimizes evaluation of the anterior cruciate ligament (ACL), horns of the menisci, femorotibial joint and femoral trochlear articular cartilage, cruciate ligaments, and extensor mechanism. The coronal plane of imaging is preferred for evaluation of the body of the menisci, and medial and lateral stabilizing structures. The axial plane is used to evaluate the patellar articular cartilage, quadriceps tendon, and medial and lateral stabilizing structures.
The routine knee MR imaging protocol at the authors’ institution ( Table 1 ) consists of axial intermediate PD with fat saturation, PD sagittal oblique without fat saturation, PD coronal without fat saturation, intermediate T2 coronal with fat saturation, and intermediate T2 sagittal oblique with fat saturation sequences. When indicated, intravenous gadolinium contrast may help to further characterize neoplastic, infectious, and inflammatory processes. Prior to gadolinium contrast administration, an axial T1-weighted sequence with fat suppression is obtained as a control sequence. Following intravenous gadolinium contrast administration, T1-weighted fat-suppressed sequences are obtained in the axial plane, and at least one additional orthogonal plane. Indications for intra-articular dilute gadolinium contrast administration include suspected meniscal retear after meniscectomy, and evaluation for instability of an osteochondral lesion.
| Sequence | Fat Saturation | FOV (cm) | Matrix | TR (ms) | TE (ms) | Slice Thickness/Gap (mm) |
|---|---|---|---|---|---|---|
| Intermediate PD axial | Y | 14 | 313 × 384 | 4430 | 11 | 3/0.6 |
| Intermediate T2 sagittal oblique | Y | 14 | 200 × 256 | 2920 | 56 | 3/0.6 |
| Intermediate T2 coronal | Y | 14 | 200 × 256 | 4050 | 56 | 3/0.6 |
| PD coronal | N | 14 | 314 × 448 | 1200 | 15 | 3/0.6 |
| PD sagittal oblique | N | 14 | 314 × 448 | 1200 | 15 | 3/0.6 |
The field strength, coil (volume surface phased array), slice thickness, field of view, matrix size, and other select imaging parameters are optimized with the goal of increasing the signal to noise ratio and decreasing scan time, thereby decreasing motion artifact. Metal artifact reduction can be achieved by orienting the long axis of metallic prosthesis parallel to both magnetic field and frequency encoding axis, employing fast spin echo techniques with increased echo train length, increasing receiver band width, decreasing field of view, and increasing the matrix size in the direction of the frequency encoding gradient.
Imaging anatomy
The knee, a hinge-type joint, is primarily composed of 3 articulating compartments: patellofemoral, medial femorotibial, and lateral femorotibial. A combination of muscles, tendons, ligaments, and extensions of the joint capsule collectively help to offer multidirectional stability to the knee, while allowing for necessary mobility. Numerous bursae about the knee allow for ease of motion of the stabilizing structures in relation to one another.
The medial femorotibial compartment is formed by the medial femoral condyle and medial tibial plateau articulation, and houses the medial meniscus and articular cartilage. Major medial stabilizers include the deep (coronary ligaments) and superficial portions of the medial collateral ligament (MCL), medial tendons (sartorius, gracilis, semitendinosus, and semimembranosus), and deep crural fascia of vastus medialis, which helps to form the medial patellar retinaculum anteriorly. Posteriorly, the deep portion of the MCL, with contributing fibers from the semimembranosus tendon and synovial sheath, form the posterior oblique ligament, a major stabilizer of the posteromedial knee. The MCL bursa is located along the middle third of the medial knee joint between the superficial and deep components of the MCL.
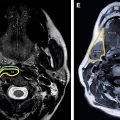
The lateral femorotibial compartment is formed by the lateral femoral condyle and lateral tibial plateau articulation, and houses the lateral meniscus and articular cartilage. It can communicate with the proximal tibiofibular joint in a minority of individuals. Lateral joint stabilizers are composed of muscles, tendons, and ligaments. The anterolateral joint is stabilized by the joint capsule and the iliotibial tract, which inserts on Gerdy’s tubercle along the anterolateral tibia, and is a fascial extension of the tensor fascia lata. The posterolateral corner is a complex anatomic area providing stabilization, achieved by several structures including the fibular (lateral) collateral ligament (FCL), biceps femoris tendon, popliteus muscle and tendon, popliteal fibular and popliteal meniscal ligaments, oblique popliteal, arcuate, and fabellofibular ligaments, and lateral gastrocnemius muscle. These structures are collectively referred to as the arcuate ligament complex. The major stabilizers of the posterolateral corner are adequately visualized on routine knee MR imaging examinations. The FCL has an oblique course from the lateral femoral condyle, immediately anterior to the origin of the lateral head of the gastrocnemius muscle, to the fibular head. The biceps femoris common tendon, directly posterior to the iliotibial tract at the level of the femoral condyles, joins the FCL to form the conjoint tendon before inserting upon the fibular head. The intra-articular segment of the popliteus tendon originates just below and passes beneath the FCL (through the popliteus hiatus), and then the arcuate ligament. The extra-articular segment of the tendon quickly joins its muscle belly, which in turn attaches to the posteromedial proximal tibial surface.
The menisci are C-shaped structures composed of relatively small anterior and larger posterior horns and a central body. The menisci are divided into an inner avascular or white-white zone (>5 mm from the capsule), middle hypovascular or red-white zone (3–5 mm from the capsule), and outer vascular or red-red zone (<3 mm from the capsule).
Several potential diagnostic pitfalls exist involving the menisci, and awareness of anatomic variants related to these structures is essential to avoid misinterpretation. The most common meniscomeniscal ligament is the anterior transverse meniscal ligament, which can be a potential diagnostic pitfall because the junction of the ligament and meniscus can mimic a tear if not properly followed through its entirety. The meniscofemoral ligaments of Humphrey and Wrisberg, located anterior and posterior to the posterior cruciate ligament (PCL), respectively, can similarly be mistaken for pseudotears or meniscal fragments of the posterior horn of the lateral meniscus at their meniscal attachment. A rare variant, the oblique meniscomeniscal ligament, courses obliquely from the posterior horn of either meniscus through the intercondylar notch between the cruciate ligaments to the anterior horn of the opposite meniscus, and can be mistaken for a flipped meniscal fragment. Physiologic small fluid within the popliteus tendon sheath can simulate a lateral meniscal tear at the body-posterior horn junction. Meniscal flounce is an unusual normal variant characterized by a single fold along the inner margin of the meniscus. It more commonly involves the medial meniscus and can be mistaken for a tear, especially on coronal images.
Imaging artifacts generated by patient motion, magic angle, arterial pulsation, susceptibility artifact/field inhomogeneity (eg, chondrocalcinosis), and the concave morphology of the menisci (edge artifact) all can create a diagnostic dilemma, and this can be avoided with improved understanding of MR imaging physics and by paying special attention to imaging technique. Hemosiderin-vacuum phenomenon from fracture or osteoarthrosis can mimic a meniscal fragment, and will be more conspicuous on gradient echo sequences.
The cruciate ligaments are situated in the intercondylar notch between the medial and lateral compartments. The ACL courses from the posteromedial aspect of the lateral femoral condyle to insert anterolateral to the anterior tibial spine. The normal ACL has a fan-shaped striated appearance on both T1-weighted and T2-weighted sequences whereas, in contrast, the PCL appears homogeneously hypointense on all sequences. The PCL has a broad origin along the mid aspect of the medial femoral condyle and tapers as it inserts along the posterior mid tibia approximately 1 cm below the joint line. Both cruciate ligaments have two distinct components, an anterolateral and posteromedial bundle. A normal recess, which can accumulate fluid, is located posterior to the PCL.
The extensor mechanism of the knee is composed of the quadriceps tendon, prepatellar quadriceps continuation, and patellar tendon. The quadriceps tendon is striated in appearance, due to interspersed fat between 4 contributing muscles: vastus lateralis, vastus intermedius (deep), rectus femoris (superficial), and vastus medialis. The patellar tendon is a hypointense band arising from the inferior pole of the patella and attaching to the tibial tuberosity. The prepatellar quadriceps continuation is a thin sliver of hypointense signal comprising superficial fibers from the rectus femoris tendon.
Numerous bursae are present around the knee joint, and allow for smooth motion of various stabilizing structures in relation to one another. Visualization of these potential spaces is commonly due to pathologic fluid accumulation (bursitis). The semimembranosus-gastrocnemius bursa, located within the posteromedial aspect of the knee, communicates with the knee joint in a majority of individuals, and is referred to as a popliteal (Baker’s) cyst. The neck of the cyst is formed by the tendon of the medial head of the gastrocnemius muscle laterally and semimembranosus tendon medially. Anteriorly, 4 bursae are commonly visualized and include the suprapatellar, prepatellar, and superficial and deep infrapatellar bursae. The anterior and posterior bursae are best seen on axial or sagittal sequences.
Medially, the pes anserine, tibial collateral ligament, and semimembranosus-tibial collateral ligament bursae are seen. The pes anserine bursa is located between the distal tibial collateral ligament and the pesanserinus, which is composed of the sartorius, gracilis, and semitendinosus tendons at their tibial insertion. The tibial collateral ligament (MCL) bursa is located at the level of the knee joint line between the superficial and deep components of the MCL, and is elongated in a vertical fashion. The semimembranosus-tibial collateral ligament bursa, an inverted U-shaped structure, does not communicate with the joint, and is positioned between the semimembranosus tendon and tibial collateral ligament at the level of the medial tibial plateau. Laterally, the iliotibial band and fibular collateral ligament (FCL)-biceps femoris bursae are found. The iliotibial band bursa is situated between the tibia and distal iliotibial band immediately proximal to its insertion on Gerdy’s tubercle. The FCL-biceps femoris bursa is found lateral to the distal FCL, and insinuates anterior and anteromedial in relation to this ligament. Superiorly, it extends to the level of the crossing of the biceps femoris tendon, and remains superficial to FCL in this location.
Knowledge of normal locations of bursae is important in order to distinguish these from pathologic processes. One example exists within the soft tissues deep to the distal iliotibial tract at the level of the lateral femoral condyle. As a normal bursa does not exist in this location, fluid accumulation is likely pathologic and related to iliotibial band friction syndrome; however, it must be differentiated from joint fluid within the lateral parapatellar recess.
The popliteal fossa is located posterior to the knee and contains several neurovascular structures that course between the thigh and leg. The popliteal artery most commonly bifurcates at the caudal aspect of the popliteus muscle into the posterior and anterior tibial arteries. A rare but important variant branching pattern, termed the aberrant anterior tibial artery, occurs when there is high (early) division of the popliteal artery, and the anterior tibial artery courses inferiorly along the anterior surface of the popliteal muscle. This vessel is at high risk of injury during orthopedic operations involving posterior knee soft tissue manipulation, drilling through the posterior tibial cortex, and proximal tibial osteomoties.
Imaging anatomy
The knee, a hinge-type joint, is primarily composed of 3 articulating compartments: patellofemoral, medial femorotibial, and lateral femorotibial. A combination of muscles, tendons, ligaments, and extensions of the joint capsule collectively help to offer multidirectional stability to the knee, while allowing for necessary mobility. Numerous bursae about the knee allow for ease of motion of the stabilizing structures in relation to one another.
The medial femorotibial compartment is formed by the medial femoral condyle and medial tibial plateau articulation, and houses the medial meniscus and articular cartilage. Major medial stabilizers include the deep (coronary ligaments) and superficial portions of the medial collateral ligament (MCL), medial tendons (sartorius, gracilis, semitendinosus, and semimembranosus), and deep crural fascia of vastus medialis, which helps to form the medial patellar retinaculum anteriorly. Posteriorly, the deep portion of the MCL, with contributing fibers from the semimembranosus tendon and synovial sheath, form the posterior oblique ligament, a major stabilizer of the posteromedial knee. The MCL bursa is located along the middle third of the medial knee joint between the superficial and deep components of the MCL.
The lateral femorotibial compartment is formed by the lateral femoral condyle and lateral tibial plateau articulation, and houses the lateral meniscus and articular cartilage. It can communicate with the proximal tibiofibular joint in a minority of individuals. Lateral joint stabilizers are composed of muscles, tendons, and ligaments. The anterolateral joint is stabilized by the joint capsule and the iliotibial tract, which inserts on Gerdy’s tubercle along the anterolateral tibia, and is a fascial extension of the tensor fascia lata. The posterolateral corner is a complex anatomic area providing stabilization, achieved by several structures including the fibular (lateral) collateral ligament (FCL), biceps femoris tendon, popliteus muscle and tendon, popliteal fibular and popliteal meniscal ligaments, oblique popliteal, arcuate, and fabellofibular ligaments, and lateral gastrocnemius muscle. These structures are collectively referred to as the arcuate ligament complex. The major stabilizers of the posterolateral corner are adequately visualized on routine knee MR imaging examinations. The FCL has an oblique course from the lateral femoral condyle, immediately anterior to the origin of the lateral head of the gastrocnemius muscle, to the fibular head. The biceps femoris common tendon, directly posterior to the iliotibial tract at the level of the femoral condyles, joins the FCL to form the conjoint tendon before inserting upon the fibular head. The intra-articular segment of the popliteus tendon originates just below and passes beneath the FCL (through the popliteus hiatus), and then the arcuate ligament. The extra-articular segment of the tendon quickly joins its muscle belly, which in turn attaches to the posteromedial proximal tibial surface.
The menisci are C-shaped structures composed of relatively small anterior and larger posterior horns and a central body. The menisci are divided into an inner avascular or white-white zone (>5 mm from the capsule), middle hypovascular or red-white zone (3–5 mm from the capsule), and outer vascular or red-red zone (<3 mm from the capsule).
Several potential diagnostic pitfalls exist involving the menisci, and awareness of anatomic variants related to these structures is essential to avoid misinterpretation. The most common meniscomeniscal ligament is the anterior transverse meniscal ligament, which can be a potential diagnostic pitfall because the junction of the ligament and meniscus can mimic a tear if not properly followed through its entirety. The meniscofemoral ligaments of Humphrey and Wrisberg, located anterior and posterior to the posterior cruciate ligament (PCL), respectively, can similarly be mistaken for pseudotears or meniscal fragments of the posterior horn of the lateral meniscus at their meniscal attachment. A rare variant, the oblique meniscomeniscal ligament, courses obliquely from the posterior horn of either meniscus through the intercondylar notch between the cruciate ligaments to the anterior horn of the opposite meniscus, and can be mistaken for a flipped meniscal fragment. Physiologic small fluid within the popliteus tendon sheath can simulate a lateral meniscal tear at the body-posterior horn junction. Meniscal flounce is an unusual normal variant characterized by a single fold along the inner margin of the meniscus. It more commonly involves the medial meniscus and can be mistaken for a tear, especially on coronal images.
Imaging artifacts generated by patient motion, magic angle, arterial pulsation, susceptibility artifact/field inhomogeneity (eg, chondrocalcinosis), and the concave morphology of the menisci (edge artifact) all can create a diagnostic dilemma, and this can be avoided with improved understanding of MR imaging physics and by paying special attention to imaging technique. Hemosiderin-vacuum phenomenon from fracture or osteoarthrosis can mimic a meniscal fragment, and will be more conspicuous on gradient echo sequences.
The cruciate ligaments are situated in the intercondylar notch between the medial and lateral compartments. The ACL courses from the posteromedial aspect of the lateral femoral condyle to insert anterolateral to the anterior tibial spine. The normal ACL has a fan-shaped striated appearance on both T1-weighted and T2-weighted sequences whereas, in contrast, the PCL appears homogeneously hypointense on all sequences. The PCL has a broad origin along the mid aspect of the medial femoral condyle and tapers as it inserts along the posterior mid tibia approximately 1 cm below the joint line. Both cruciate ligaments have two distinct components, an anterolateral and posteromedial bundle. A normal recess, which can accumulate fluid, is located posterior to the PCL.
The extensor mechanism of the knee is composed of the quadriceps tendon, prepatellar quadriceps continuation, and patellar tendon. The quadriceps tendon is striated in appearance, due to interspersed fat between 4 contributing muscles: vastus lateralis, vastus intermedius (deep), rectus femoris (superficial), and vastus medialis. The patellar tendon is a hypointense band arising from the inferior pole of the patella and attaching to the tibial tuberosity. The prepatellar quadriceps continuation is a thin sliver of hypointense signal comprising superficial fibers from the rectus femoris tendon.
Numerous bursae are present around the knee joint, and allow for smooth motion of various stabilizing structures in relation to one another. Visualization of these potential spaces is commonly due to pathologic fluid accumulation (bursitis). The semimembranosus-gastrocnemius bursa, located within the posteromedial aspect of the knee, communicates with the knee joint in a majority of individuals, and is referred to as a popliteal (Baker’s) cyst. The neck of the cyst is formed by the tendon of the medial head of the gastrocnemius muscle laterally and semimembranosus tendon medially. Anteriorly, 4 bursae are commonly visualized and include the suprapatellar, prepatellar, and superficial and deep infrapatellar bursae. The anterior and posterior bursae are best seen on axial or sagittal sequences.
Medially, the pes anserine, tibial collateral ligament, and semimembranosus-tibial collateral ligament bursae are seen. The pes anserine bursa is located between the distal tibial collateral ligament and the pesanserinus, which is composed of the sartorius, gracilis, and semitendinosus tendons at their tibial insertion. The tibial collateral ligament (MCL) bursa is located at the level of the knee joint line between the superficial and deep components of the MCL, and is elongated in a vertical fashion. The semimembranosus-tibial collateral ligament bursa, an inverted U-shaped structure, does not communicate with the joint, and is positioned between the semimembranosus tendon and tibial collateral ligament at the level of the medial tibial plateau. Laterally, the iliotibial band and fibular collateral ligament (FCL)-biceps femoris bursae are found. The iliotibial band bursa is situated between the tibia and distal iliotibial band immediately proximal to its insertion on Gerdy’s tubercle. The FCL-biceps femoris bursa is found lateral to the distal FCL, and insinuates anterior and anteromedial in relation to this ligament. Superiorly, it extends to the level of the crossing of the biceps femoris tendon, and remains superficial to FCL in this location.
Knowledge of normal locations of bursae is important in order to distinguish these from pathologic processes. One example exists within the soft tissues deep to the distal iliotibial tract at the level of the lateral femoral condyle. As a normal bursa does not exist in this location, fluid accumulation is likely pathologic and related to iliotibial band friction syndrome; however, it must be differentiated from joint fluid within the lateral parapatellar recess.
The popliteal fossa is located posterior to the knee and contains several neurovascular structures that course between the thigh and leg. The popliteal artery most commonly bifurcates at the caudal aspect of the popliteus muscle into the posterior and anterior tibial arteries. A rare but important variant branching pattern, termed the aberrant anterior tibial artery, occurs when there is high (early) division of the popliteal artery, and the anterior tibial artery courses inferiorly along the anterior surface of the popliteal muscle. This vessel is at high risk of injury during orthopedic operations involving posterior knee soft tissue manipulation, drilling through the posterior tibial cortex, and proximal tibial osteomoties.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree