Magnetic resonance (MR) imaging is the modality of choice for evaluating the soft tissues of the thigh and leg because of its superior soft tissue contrast resolution, multiplanar imaging capability, and lack of ionizing radiation. The superb image quality facilitates learning normal imaging anatomy, which ultimately forms the foundation of diagnostic interpretation. The purpose of this article is twofold: (1) depict normal MR anatomy throughout the thigh and leg using representative MR images, emphasizing a compartmental approach; and (2) describe and explain the rationale of standard imaging protocols.
Developing a solid understanding of basic magnetic resonance imaging (MR imaging) principles and musculoskeletal imaging protocols, as well as the appearance of normal imaging anatomy, is crucial to interpret musculoskeletal MR imaging examinations at a diagnostic level. This knowledge can then be applied to one’s understanding of pathology commonly encountered in the area of interest. Careful attention should be focused on awareness of commonly encountered anatomic variants and diagnostic pitfalls to improve diagnostic accuracy and avoid misinterpretation.
In this article, focus is placed on depicting normal anatomy at representative levels throughout the thigh and leg, describing and providing rationale for routine imaging protocols, and discussing frequently encountered anatomical variants and imaging pitfalls. This will serve as a basic foundation for accurate evaluation of the many pathologic processes that may involve the thigh and leg.
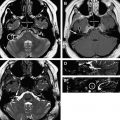
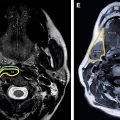
MR imaging of a healthy volunteer was performed on a 3T MR imaging unit (Siemens, Erlangen, Germany). Select axial T1-weighted (T1W) images are displayed to depict anatomical structures to best advantage, and allow the reader to conceptualize relevant anatomy while emphasizing compartmental organization.
Protocols
Routine thigh and leg MR imaging protocols at our institution include a combination of T1W, T2W, and short tau inversion recovery (STIR) sequences. T1W sequences provide excellent depiction of anatomic detail, bone marrow signal alteration, fat within mass lesions, identification of subacute blood products, and presence of enhancing tissue after gadolinium contrast administration. T2W sequences identify tissues with increased water content that can be seen in the setting of a broad range of pathology, including neoplastic, infectious, inflammatory, and traumatic processes. Acquisition of T2W sequences is performed using the fast spin-echo (FSE) technique to reduce scan time and minimize susceptibility artifact from field inhomogeneity. Frequency selective fat suppression is used on T2W sequences to accentuate pathologic abnormalities. STIR sequences allow for a more sensitive evaluation of soft tissue and bone marrow edema, and offer more reliable uniform fat suppression; however, currently, in many institutions, FSE T2W and STIR sequences are used similarly. Intravenous gadolinium contrast administration allows differentiation of cystic versus solid masses, and detection of hyperemic tissues related to viable tumor as opposed to necrosis, and phlegmonous/inflammatory tissue as opposed to abscess formation. The axial plane of imaging is preferred for a compartmental approach to evaluation and in assessing the neurovascular structures, muscles, and fascial layers. The coronal plane provides a general overview of the region of interest, and the sagittal plane aids in better depicting the cranial-caudal extent of muscle disease and myotendinous junction involvement. The field strength, coil (volume surface phased array), slice thickness, field of view, matrix size, and other select imaging parameters are optimized with the goal of increasing the signal-to-noise ratio and decreasing scan time, thereby decreasing motion artifact. Patient-specific factors including body habitus and ability to cooperate, desired region of coverage, and presence of metallic hardware or foreign bodies must also be considered.
Specifically, our routine protocol for both the thigh and leg ( Table 1 ) includes an axial T2W sequence with fat saturation, at least 2 planes of T1W sequences without fat saturation, and coronal and sagittal STIR sequences. If gadolinium contrast is indicated, at minimum, precontrast and postcontrast fat-suppressed axial T1W sequences are obtained. At least one additional postcontrast fat-suppressed T1W sequence is acquired, either in the sagittal or coronal orientation; however, both are preferable. Ultimately, the final imaging protocol is tailored to patient-specific factors with the desired intention of obtaining the best image quality to answer the clinical question.
| Thigh | ||||||
| Sequence | Fat Saturation | FOV, cm | Matrix | Slice Thickness/Gap, mm | TR/TI, ms | TE, ms |
| Coronal T1 | N | 40 | 256 × 256 | 5/2.5 | 750 | 9.5 |
| Axial T1 | N | 20 | 256 × 256 | 4/2.0 | 750 | 9.6 |
| Sagittal T1 | N | 40 | 256 × 256 | 5/2.5 | 750 | 9.5 |
| Axial T2 | Y | 20 | 256 × 256 | 4/1.2 | 5250 | 81 |
| Coronal STIR | N/A | 40 | 184 × 384 | 3/0.9 | 7380/210 | 27 |
| Sagittal STIR | N/A | 40 | 184 × 384 | 3/0.9 | 7380/210 | 27 |
| a Axial T1 Pre. | Y | 20 | 256 × 256 | 4/2.0 | 750 | 9.6 |
| Leg | ||||||
| Sequence | Fat Saturation | FOV, cm | Matrix | Slick Thickness/Gap, mm | TR/TI, ms | TE, ms |
| Coronal T1 | N | 35 | 256 × 256 | 5/1.5 | 750 | 9.5 |
| Axial T1 | N | 20 | 256 × 256 | 5/1.5 | 750 | 9.6 |
| Sagittal T1 | N | 40 | 256 × 256 | 5/2.5 | 750 | 9.5 |
| Axial T2 | Y | 20 | 256 × 256 | 5/1.5 | 5250 | 81 |
| Coronal STIR | N/A | 35 | 184 × 384 | 3/0.9 | 7380/210 | 27 |
| Sagittal STIR | N/A | 40 | 184 × 384 | 3/0.9 | 7380/210 | 27 |
| a Axial T1 Pre. | Y | 20 | 256 × 256 | 5/1.5 | 750 | 9.6 |
a Optional, if intravenous contrast is indicated. Post–gadolinium contrast T1W sequences are obtained in at least 2 orthogonal planes with fat suppression.
Imaging anatomy
Thigh
The thigh is best described in terms of compartmental anatomy, and is composed of anterior, posterior, and medial (adductor) compartments. In terms of spread of pathologic processes, such as tumor and infection, other delineated compartments include the skin and subcutaneous fat, bone bounded by periosteum and cortex, and parosteal space (between the bone and overlying soft tissues). The thigh extends from the superior margin of the subtrochanteric region through the distal femoral metadiaphysis. Each compartment is composed of muscles, neurovascular structures, and intermuscular fascia. Muscles are of intermediate signal intensity to fat on T1W and T2W FSE sequences. Peripheral nerves are round or oval and have a fascicular appearance, best depicted on T2W sequences. They are isointense to muscle on T1W sequences with intermixed increased signal intensity similar to fat. On T2W sequences, they are isointense to slightly hyperintense relative to muscle. In general, arteries should be hypointense to muscle on all sequences. Veins have variable signal intensity on T1W and T2W sequences.
The iliotibial tract, tensor muscle of fascia lata, quadriceps femoris (vastus medialis, vastus lateralis, vastus intermedius, and rectus femoris), and sartorius muscles are located within the anterior compartment. The sartorius muscle is long, thin, and bandlike, originating from the anterior superior iliac spine, obliquely coursing over the proximal thigh along the inner margin of the quadriceps muscles, and extending to the posteromedial aspect of the knee. Its tendon extends anteriorly and attaches to the anteromedial surface of the proximal tibia superficial to the gracilis and semitendinosus tendons. Together, these 3 tendons comprise the pes anserinus tendon complex. The rectus femoris muscle originates from the anterior inferior iliac spine as 2 tendons: the straight and reflected heads. The vastus lateralis muscle arises from the anterior superior aspect of the femoral shaft and the lateral facet of the linea aspera; the vastus medialis muscle originates from the intertrochanteric line and medial aspect of linea aspera; the vastus intermedius muscle arises between these 2 muscles and subjacent to the rectus femoris muscle, along the anterior aspect of the femoral shaft. Differentiation of these muscles is sometimes difficult as they may be partially fused at their origins and insertions. Distally, these 4 muscles form the quadriceps tendon, which contains the patella, the largest sesamoid in the body.
The posterior compartment contains the semimembranosus, semitendinosus, and long and short heads of the biceps femoris muscles. The major innervation of the lower extremity, the sciatic nerve, is also located in this compartment. The semitendinosus and long head of the biceps femoris muscles originate from a common tendon along the medial facet and distal margin of the ischial tuberosity. The semitendinosus muscle, fusiform in shape, is more tendinous distally, and inserts along the medial aspect of the proximal tibia deep to the sartorius tendon. The short head of the biceps femoris muscle originates from the linea aspera in the mid to distal thigh and joins the long head of the biceps femoris muscle to insert on the fibular head laterally. The semimembranosus tendon arises from the lateral facet of the ischial tuberosity and has a broad insertion along the proximal posteromedial tibia.
The medial compartment contains the adductor brevis, longus, and magnus muscles as well as gracilis, pectineus, and obturator externus musculature. The gracilis muscle is the most superficial and medial, and originates from the inferior ischiopubic ramus and inserts deep to the sartorius tendon along the proximal medial tibia after curving anteriorly around the posteromedial femoral condyle. The pectineus muscle is triangular in shape and originates at the superior pubic ramus along with the adductor longus muscle more medially. It inserts onto the pectineal line of the femoral shaft, whereas the adductor longus muscle inserts onto the middle third of the linea aspera. The adductor brevis muscle is also triangular in shape, and originates from the inferior pubic ramus and inserts along the upper third of the linea aspera. The adductor magnus muscle, the largest of the adductor muscle group, originates along the inferior pubic ramus and ischial tuberosity, and inserts along the entire linea aspera as well as the adductor tubercle of the distal femur. The obturator externus muscle, the deepest of the muscles in the medial compartment, originates from the anterior two-thirds of the obturator foramen (formed by the lateral surface of the ischiopubic ramus) and inserts into the trochanteric fossa of the proximal femur. The neurovascular bundle, including the saphenous nerve, is located in this compartment.
Leg
The leg extends from the proximal tibial metaphysis through the distal metaphysis. The soft tissues are similarly organized in a compartmental fashion, and are supported by the tibia and fibula. The lower leg is composed of 4 compartments: anterior, superficial posterior, deep posterior, and lateral. The interosseous membrane separates the anterior and deep posterior compartments. The transverse septum separates the superficial and deep posterior compartments.
The anterior compartment contains the tibialis anterior, extensor digitorum longus, and extensor hallucis longus muscles, and the anterior neurovascular bundle, including the anterior tibial artery and vein, and deep peroneal nerve. The tibialis anterior muscle originates from the lateral surface of the tibia and neighboring interosseous membrane in the upper leg, and extends distally over the anterior tibia to insert upon the dorsal aspect of the first metatarsal. The extensor digitorum longus muscle originates from the anterior surface of the interosseous membrane and fibula, courses inferiorly along the anterior tibia, and gives rise to tendons that insert upon the distal phalanges of the second through fifth toes. The peroneus tertius muscle, when variably present, is closely associated with the extensor digitorum longus muscle, coursing in the same synovial sheath; however, its tendon attaches to the dorsal aspect of the base of the fifth metatarsal. The extensor hallucis longus muscle originates from the distal aspect of the fibula and interosseous membrane, and extends distally across the ankle and foot to insert upon the distal phalanx of the first toe. At the level of the ankle, the tendons in this compartment are stabilized by the superior and inferior extensor retinacula.
The deep posterior compartment contains the popliteus, tibialis posterior, flexor digitorum, and flexor hallucis longus muscles, as well as the posterior tibial and peroneal arteries and the posterior tibial nerve. The popliteus muscle originates from the lateral femoral condyle and inserts upon the popliteal line of the tibia. The flexor digitorum longus muscle originates from the popliteal line and posterior aspect of the tibia. Its tendon passes posterior and around the medial malleolus, and gives rise to 4 tendinous slips that insert upon the bases of the distal phalanges of the second through fourth toes. The flexor hallucis longus muscle originates from the distal two-thirds of the fibula, and its tendon courses around the medial malleolus, posterior to the flexor digitorum longus tendon, and between the medial and lateral tubercles of the posterior process of the talus to insert upon the distal phalynx of the first toe. The tibialis posterior muscle originates from the lateral aspect of the tibia and adjacent interosseous membrane. It courses around the medial malleolus, anterior to the flexor digitorum longus tendon, and has a broad insertion upon multiple structures along the plantar surface of the foot, predominantly inserting upon the navicular and, to a lesser degree, the cuneiform bones.
The plantaris, soleus, and medial and lateral heads of the gastrocnemius muscles, along with the sural nerve, are located within the superficial posterior compartment. The medial and lateral heads of the gastrocnemius musculature originate from immediately superior to the medial and lateral femoral condyles, respectively, and insert upon the deep aspect of the Achilles tendon at mid leg. The soleus muscle originates from the tibia and fibula, deep to the gastrocnemius musculature, and inserts upon the deep aspect of the Achilles tendon at a variable level. The plantaris muscle belly is short and originates from the distal lateral linea aspera in close association with the lateral head of gastrocnemius muscle. Its long tendon courses inferiorly between the soleus muscle and the medial head of gastrocnemius muscle, and inserts upon the posterior superior aspect of the calcaneus along the medial margin of the Achilles tendon.
The lateral compartment contains the peroneus longus and peroneus brevis muscles as well as the common and superficial peroneal nerves. It is separated from the anterior and posterior compartments by intermuscular septa. The peroneus longus muscle arises from the upper half of the lateral surface of the fibula and adjacent structures, descends lateral and then posterior to the peroneus brevis muscle, and inserts along the plantar surface of the base of the first metatarsal. It lies posterior to the lateral malleolus and lateral to the calcaneus at these respective levels. Along the plantar surface of the foot, the tendon courses adjacent to the cuboid (cuboid tunnel) and tarsometatarsal articulations. The peroneus brevis muscle originates from the middle one-third of the lateral aspect of the fibula and inserts upon the dorsolateral aspect of the base of the fifth metatarsal. Both peroneal tendons are stabilized by the superior and inferior peroneal retinacula.
Anatomic variants occur most commonly within the mid to distal leg, and with less frequency within the thigh. Accessory muscles comprise most of the variant anatomy. The peroneus tertius, a common anatomic variant located within the anterior compartment, originates from the anterior aspect of the distal fibula and extensor digitorum longus muscle as discussed previously. Accessory soleus musculature is most commonly unilateral, and arises from the fibula, soleal line of the tibia, and anterior aspect of the soleus. There are 5 types related to insertion location. The peroneus quartus muscle is located within the lateral compartment. It originates from and is situated medial and posterior to the peroneus brevis and longus musculature. Several types exist and are further classified based on their insertions. The peroneus calcaneus internus muscle is a rare anatomic variant that is usually asymptomatic; however, it has been clinically associated with posterior ankle impingement and flexor hallucis longus tenosynovitis. Flexor digitorum accessorius longus is an uncommon variant that has been associated with tarsal tunnel syndrome.
Variations, including accessory slips and anomalous origins of the gastrocnemius and popliteus musculature, some of which may lead to popliteal artery entrapment syndrome depending on their effect upon the underlying popliteal vasculature, are also not infrequently encountered. An uncommon accessory popliteus shares a common origin with the lateral head of the gastrocnemius and courses inferomedially within the deep popliteal fossa, situated anterior to the popliteal vessels. It inserts onto the posteromedial joint capsule of the knee, and may potentially have a compressive effect upon the overlying popliteal neurovascular bundle.
Tensor fasciae suralis, a very rare accessory muscle, can arise from any hamstring muscle; however, it most commonly originates from the distal semitendinosus muscle. It can insert onto the medial head of the gastrocnemius, posterior fascia of the leg, or onto the superficial aspect of the Achilles tendon by means of a long, thin tendon. Tensor fasciae suralis is superficial within the popliteal fossa, situated lateral to the semimembranosus and semitendinosus muscles and medial to the biceps femoris muscle.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree