When initially conceptualized, this issue was tasked with providing a practical guide to the normal MRI anatomy “from head to toe.” Describing the innumerable anatomic features of a given body part could fill an entire journal, if not a full textbook; this is a task that would be impractical in this setting. Conversely, distilling normal anatomy down to a more clinically important subset is also a daunting task and requires careful consideration—what to include, what to exclude, when to direct the reader to an additional source. Fortunately, clinical MRI is largely driven by protocols.
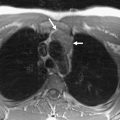
Since protocols directly control what images are obtained and why the images have certain characteristics, they are central to any discussion on the MRI appearance of normal anatomy. Therefore, the body can be segmented into smaller pieces based on anatomic regions that have unique or similar imaging protocols, providing a basis for the various articles that follow. These articles are deliberately more numerous and slightly shorter in length than a typical issue. Traditional systems-based radiology subspecialties have been subdivided into several parts, including four separate areas of the central nervous system (brain, skull base, neck, and spine) and seven separate areas of the musculoskeletal system, with different articles addressing joint-specific considerations and longitudinal anatomy of the extremities as a whole. Although computed tomography (CT) is a mainstay for imaging the chest, abdomen, and pelvis, advances in MRI have led to increasing utilization in each of these body sections, particularly with novel organ-specific imaging protocols. Continued interest and adoption in these areas are likely due to increasing concerns about cumulative radiation doses from multiple CT exams. Breast MRI has also emerged as a powerful clinical tool with unique technical facets and anatomy.
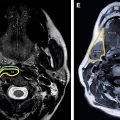
Each article in this issue features a discussion of relevant protocol considerations, along with sample technical specifications from the author’s institution. The normal anatomy is reviewed, highlighted by annotated figures and detailed figure legends. Important variants and clinical pitfalls are also discussed and illustrated. The goal of each article is to provide a framework for both anatomic knowledge and technical understanding. If further detail is required, appropriate references have been cited to allow for additional reading.
I would like to thank the contributing authors for their dedication and hard work. Each has done an outstanding job of creating a contribution that blends text and figures to reveal specific anatomy using their own individual style. Although the task of delineating normal anatomy can seem overwhelming at first, all of the contributing authors have tackled this challenge with remarkable skill and thought. Ideally, the reader will find pragmatic gains from each of the articles, whether from technical refinement, anatomic detail, or both. I hope that the knowledge gained from each article will provide a foundation for the classic radiology teaching paradigm of “you see what you know”—without understanding why the image was acquired and what normal anatomic features are present, correct identification of pathology would be impossible.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree