NUCLEAR MEDICINE: INTRODUCTION AND GENERAL PRINCIPLES
KEY POINTS
- Nuclear medicine has important niche roles to play in head and neck disease.
- The use of radionuclide studies must be thoughtfully integrated with the data from anatomic imaging studies for almost all indications.
Several nuclear medicine studies provide useful information in focused clinical problems. Currently, the dominant application is positron emission tomography (PET) using fluorine-18 2-fluoro-2-deoxy-D-glucose (FDG) predominantly for tumor imaging, even though FDG is an imperfect tumor-imaging agent. Each of the studies currently used with some frequency are discussed in the following sections. It is very important than any of these radionuclide studies, when suggested or ordered, be properly integrated with anatomic imaging studies and contribute incremental data that will make a difference in medical decision making and clinical outcomes.
POSITRON EMISSION TOMOGRAPHY
FDG-PET with or without computed tomography (CT) anatomic registration has an evolving role in the imaging of head and neck cancer. Earlier stand-alone PET instruments have essentially given way to combined PET/CT units. PET/CT makes FDG-PET images easier to interpret. The earliest experience regarding the management of head and neck cancer using FDG imaging was generated with single photon emission computed tomography (SPECT) and stand-alone PET instruments.1–3 That early data has now been enriched and essentially corroborated by the rapidly expanding reported PET/CT experience for the legitimate uses of FDG-PET in the head and neck region.
FDG-PET was approved for reimbursement from the outset for the diagnosis, staging, and restaging of head and neck cancer based on that earlier experience. This has led to some current significant overusage of the technique. The role of FDG-PET should be focused and based on the need for this data in medical decision making for each particular patient.
There is a role for FDG-PET in the initial diagnosis of head and neck cancer. The specific indications vary among the institutions and preferences of the referring physicians. Such indications will be discussed in this chapter.
It is not simple to perform a truly diagnostic CT examination for head and neck cancer using the CT images obtained from PET/CT. CT protocols, while more simple with the newer volume acquisition techniques (Appendix A), still require more careful attention to field of view, gantry angulation, and slice thickness than studies typically obtained during a PET/CT examination even when intravenous contrast is administered. These protocols are often not compatible with the “fixed” gantry necessary of registration of the PET/CT images. Currently, the best approach is to do a “nondiagnostic” CT for attenuation correction and to help with anatomic localization along with the PET examination and then a separate diagnostic CT for the proper anatomic imaging of the cancer. This strategy obviously adds expense on the front end. The more careful anatomic approach will, however, will likely save expense on the back end by providing optimal data for medical decision making.
Initial Staging
The majority of squamous cell carcinoma (SCCA) primary sites >1 cc can be detected with FDG-PET. Smaller lesions may not be detected. Mucosal extent cannot be accurately shown.3,4 Hence, there is limited, if any, value in performing FDG-PET for diagnostic evaluation of the primary site.
PET stages lymph nodes in head and neck cancer with a sensitivity of 70% to 95%, comparable to CT or magnetic resonance (MR), depending on the population studied.3–8 There may be some incremental gain in neck staging with FDG-PET in selected clinical circumstances. A 95% sensitivity, however, is likely not a sustainable expectation. There may be a high negative predictive value (NPV) for FDG-PET for evaluating the N0 neck; however, it should not be used to confirm the N0 neck since the risk assessment should be based on factors other than any imaging study result. There remains significant debate regarding the role of FDG-PET for evaluating cervical lymph node metastases.
The reluctance for blanket recommendations for the use of FDG-PET is judicious since such additional information may frequently not alter treatment plans and also may have no survival or morbidity reduction impact. The important question is whether the cost is justified by any real change in medical decision making and whether that in turn provides survival or quality-of-life benefits. Currently, such benefit has not been established by well-controlled prospective data.
Planning Radiotherapy and Chemoradiation Strategies
FDG activity using standard uptake values (SUV-max) may help predict response to therapy. This is in part based on the notion that a higher SUV value is correlated with a worse prognosis. This requires standardization of technique at individual institutions to establish the “local” reliability and consistency of SUV data. SUV changes after a trial of chemotherapy data might help to decide between whether organ preservation with multimodality therapy is possible (Fig. 5.1A–D). By the same reasoning, even when both surgery and radiation are planned, such a trial may suggest that chemoradiation may be enough or that chemotherapy will not result in an improved rate of local control. Such data may also be used in refining dose escalation strategies (Fig. 5.1E). By and large, SUV is really not a parameter that should be strictly relied on for serious medical decision making.
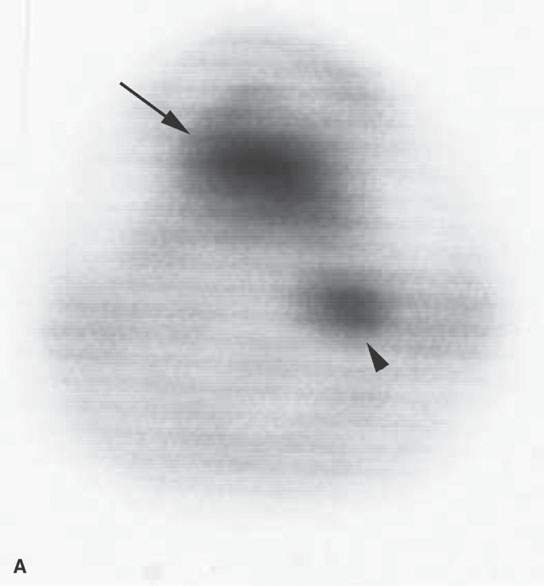
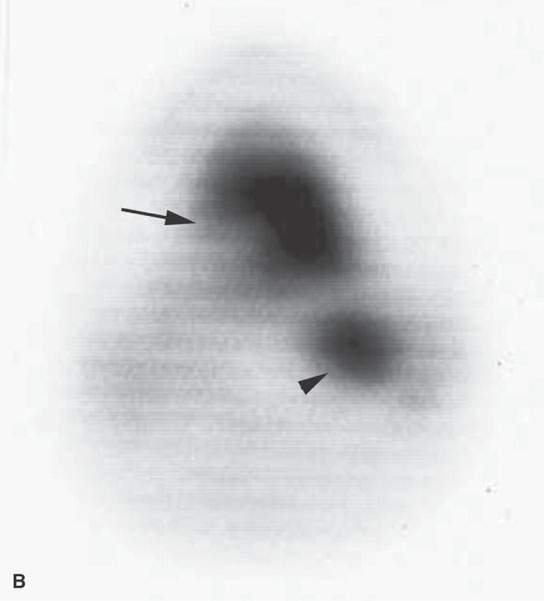
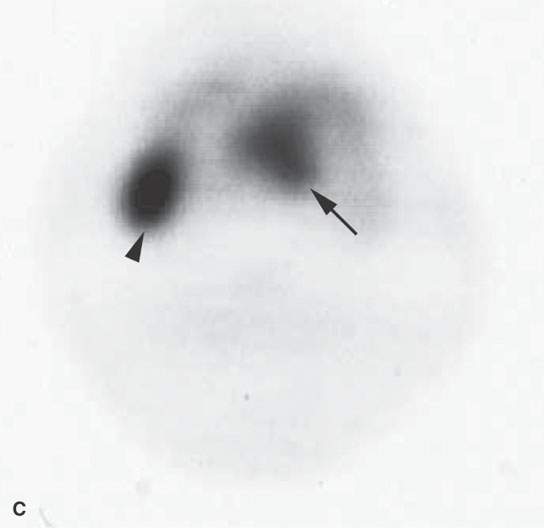
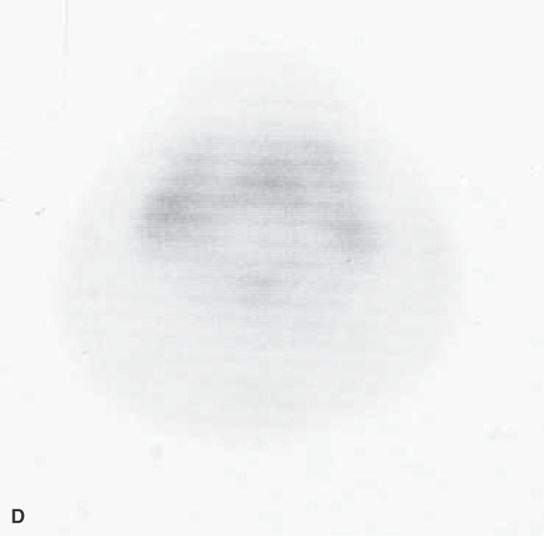
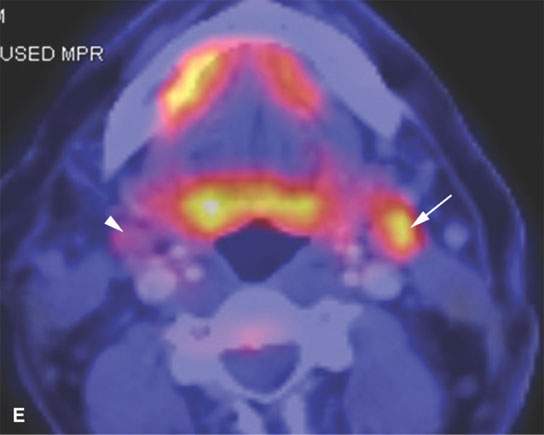
FIGURE 5.1. Fluorine-18 2-fluoro-2-deoxy-D-glucose positron emission tomography (FDG-PET) to predict the response to neoadjuvant therapy. A, B: Axial PET was performed pretreatment and following one cycle of neoadjuvant chemotherapy. There is no reduction in FDG uptake at the tongue base squamous cell carcinoma (arrows) or in the abnormal lymph node (arrowheads) following one cycle of neoadjuvant therapy. The persistent FDG uptake corresponded to <50% reduction in size at endoscopy. As a result, this patient was felt to a “nonresponder” to neoadjuvant therapy and was treated surgically. C, D: Axial PET was performed pretreatment and following one cycle of neoadjuvant chemotherapy in a different patient. The posttreatment study showed complete reduction at the primary site (arrow) and lymph node (arrowhead). These findings corresponded with >50% reduction in size at endoscopy. As a result, this patient was felt to be a responder to neoadjuvant chemotherapy and was treated with nonsurgical organ preservation therapy. E: Dose modulation for lymph node treatment. This patient had a low-volume tongue base carcinoma (note as an aside all of the spurious activity involving the floor of the mouth on both sides) and elected to be treated with nonsurgical organ preservation therapy. The white arrow shows unequivocal uptake in a left level II lymph node. This node was part of the gross tumor volume and was treated to full dose. The arrowhead shows mild uptake in a nonenlarged level II node. Because of this uptake, this lymph node was included in the clinical tumor volume. Multiple level V nodes have no uptake. No dose escalation was performed on these lymph nodes.
Some propose that the targeting of gross tumor volume (GTV) using FDG-PET data changes the GTV contours when compared with contours obtained using CT. However, there has been no definitive study ensuring that these contours are more accurate.1–5 This requires far more validation until it is accepted as true, since errors in this regard could lead to undertreatment. Treatment plans in place are based on 30 to 40 years of experience in the modern era of radiotherapy (RT) and more modern principles of intensity-modulated radiotherapy (IMRT). This knowledge base cannot be discarded before newer approaches are validated by properly controlled studies by at least several experienced groups.
“Unknown” Primary
Patients who presents with a cervical node secondary to squamous cell cancer may not have a detectable primary tumor site. CT/MR alone, in the hands of experienced observers, identifies the primary site in about 50% of these cases.3 FDG imaging identifies the primary site with greater sensitivity approaching 90% but a specificity of about 50%. However, PET/CT is still a reasonable modality for this indication in imaging negative patients since a positive FDG-PET study can help direct endoscopic biopsy, making this procedure less “speculative” than in the past (Fig. 5.2).9 The main reasons for false-positive studies and low specificity is the tendency of pharyngeal tonsillar tissue to take up FDG normally (Fig. 5.3).
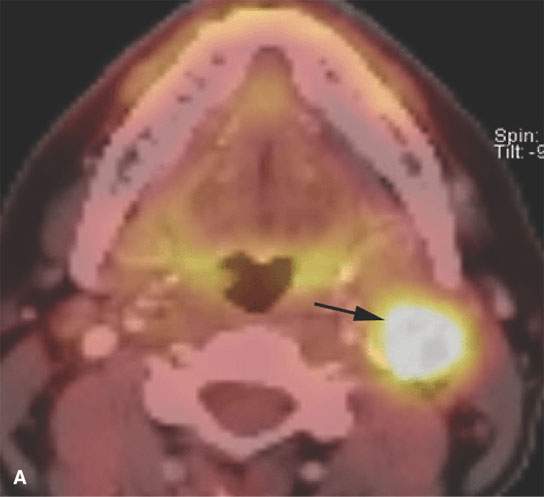
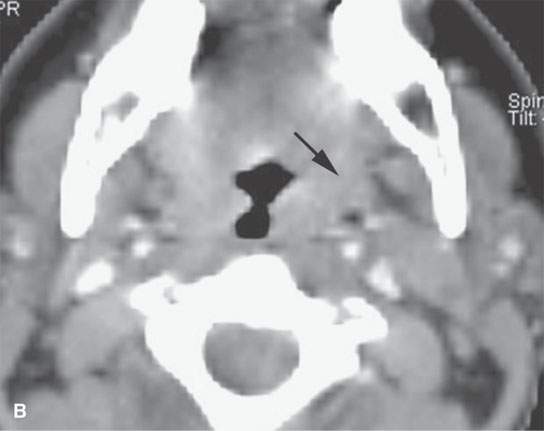

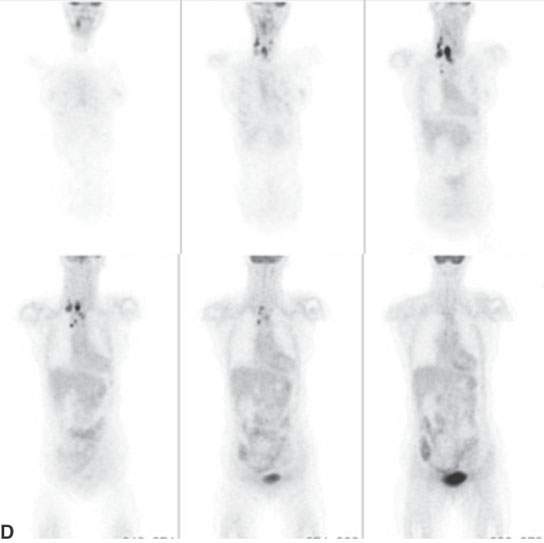
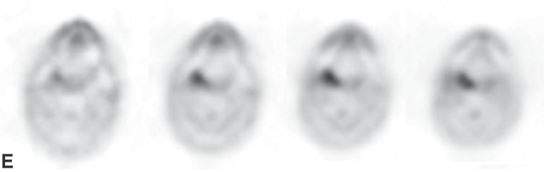
FIGURE 5.2. Unknown primary. A: There is an enlarged, fluorine-18 2-fluoro-2-deoxy-D-glucose (FDG) avid left level II node. Biopsy revealed squamous cell carcinoma (arrow). There was no mucosal lesion seen at endoscopy. B: Axial computed tomography (CT) from positron emission tomography (PET)/CT shows no aggressive lesion (arrow). C: Co-registered PET/CT shows a focal area of increased uptake involving the left tonsil (arrow). The patient underwent a left tonsillectomy, which was confirmed to be a clinically occult left tonsillar carcinoma. D: Coronal PET images (progressing anterior to posterior), showing widespread cervical, supraclavicular, and right paratracheal adenopathy. The “unknown primary tumor” site is also seen but more obvious in (E). E: Transverse slices from a “zoomed” PET acquisition of the face (separate from the whole-body PET study), showing the now-obvious right tonsillar primary tumor site. Separate “zoomed” acquisitions of the face are not typically done at most centers but are considered essential to state-of-the-art head and neck FDG-PET.
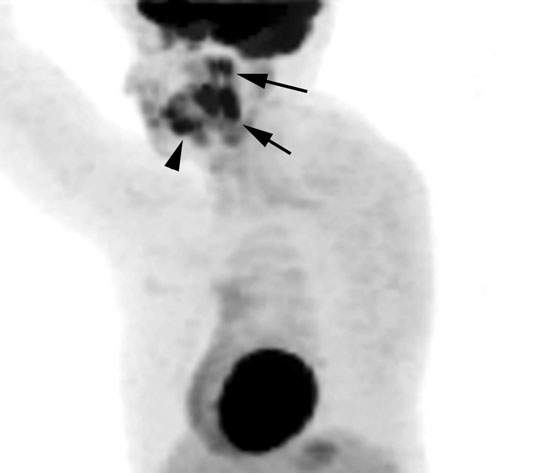
FIGURE 5.3. Normal relatively symmetric uptake in the lymphoid tissue of the Waldeyer ring (arrows) and also in oral cavity structures(arrowhead). Such uptake limits the utility of fluorine-18 2-fluoro-2-deoxy-D-glucose positron emission tomography (FDG-PET) for detecting mucosally nonapparent tumors of the upper pharynx.
Posttreatment Surveillance
FDG-PET is a very useful tool in posttreatment surveillance (Fig. 5.4). Postradiotherapy tissue necrosis or persistent masses can mimic recurrent tumor on anatomic imaging studies. Both may result in contrast-enhancing focal masses (Figs. 5.5 and 5.6). FDG-PET imaging is imperfect for distinguishing between the effects of treatment or posttreatment “sterilized” residual masses but can improve somewhat on anatomic imaging with CT and MRI (Fig. 5.6). FDG is a good but nonspecific tumor-imaging agent that has its own limitations in this regard, mainly related to the timing of the studies following RT and false-positive results.
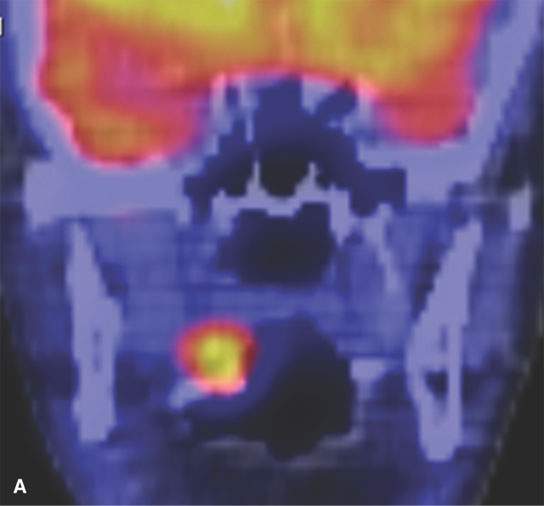
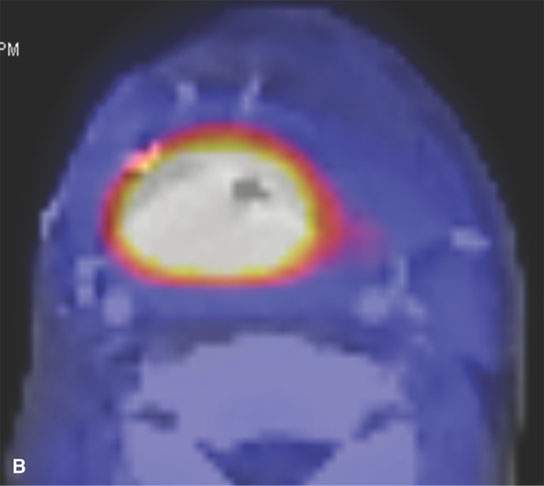
FIGURE 5.4. Restaging of recurrent squamous cell carcinoma (SCCA). This patient had a posterior wall pharyngeal SCCA that was treated surgically with reconstruction of the pharynx with a myocutaneous flap. This patient developed a new primary carcinoma of the soft palate, and the patient was felt to be a surgical candidate since there were no other lesions seen at endoscopy. A: Positron emission tomography/computed tomography (PET/CT) shows a focal area of abnormal uptake involving the soft palate corresponding to the soft palate carcinoma. B: However, there is a large area of abnormal uptake involving the pharynx. This represents a large clinically occult recurrence deep to the surgical flap. As a result of the PET/CT findings, this patient was treated with palliative therapy.
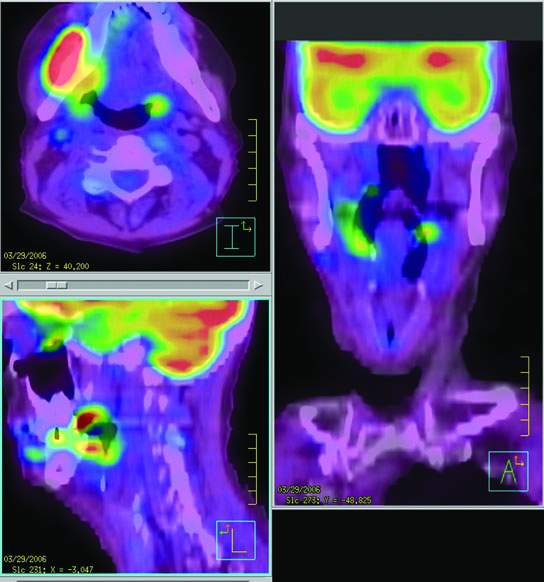
FIGURE 5.5. Fluorine-18 2-fluoro-2-deoxy-D-glucose positron emission tomography (FDG-PET)/computed tomography fusion images showing a large area of recurrent tumor growing around the right mandible as well as adjacent to an ulcer in the right base of tongue and in the left tonsil. Originally, there was concern that this might be an osteoradionecrosis of the mandible following radiotherapy.
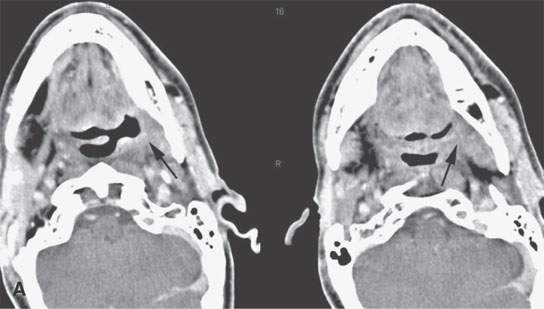

FIGURE 5.6. A patient treated for tongue base cancer who developed a soft tissue mass at the left glossotonsillar sulcus and tongue base about 6 weeks after the completion of radiotherapy. A: Contrast-enhanced computed tomography shows a residual infiltrating mass. (arrows) B: Selected correlating images from a contemporary fluorine-18 2-fluoro-2-deoxy-D-glucose positron emission tomography (FDG-PET) study showing the tissue to be hypermetabolic (arrows). (NOTE: The soft tissue findings on physical examination appeared to be due to tissue necrosis. Biopsy was delayed, and the anatomic imaging showed no progressive increase in the size of the mass over the next 3 months. FDG-PET remained positive for over 2 years. The patient is at 6 years, and the primary site is controlled. The patient is disease free.)
FDG accumulation in a cancer may disappear rapidly under therapy in the absence of ultimate control.10–14 In general, most head and neck cancers treated with RT and/or chemo RT will disappear on FDG imaging during and after therapy; however, uptake may return at the primary site until about 10 to 12 weeks post therapy. Therefore, current practice is to withhold FDG imaging for early post RT and/or chemo RT surveillance to 12 weeks post therapy (Fig. 5.1). If a tumor fails to disappear at FDG-PET, it is an unfavorable prognostic sign. However, surveillance during and up to 12 weeks following treatment is not cost justified outside of clinical trials assessing tumor metabolism and aimed at creating new treatment strategies based on early response measured by this parameter (Fig. 5.1A–D). Even at 12 weeks post therapy, FDG-PET imaging remains imperfect. The most reliable result is a negative scan. NPVs after 12 weeks approach 100%.14 Unfortunately, postsurgical and postirradiation reactive changes including necrosis with resulting reactive changes and granulation tissue can accumulate FDG so that a positive study is only about 70% predictive of recurrence (Fig. 5.6).10–14 If definitive medical decision making requires a higher true-positive rate, positive FDG results must be verified with tissue sampling. It is also important to keep in mind that deep biopsies to confirm false-positive FDG-PET findings can initiate and/or accelerate a laryngeal or mandibular necrosis. The decisions with regard to when to sample and how aggressive to be in that sampling remain a very difficult dilemma even with our most modern imaging tools.
Studies have shown variable results regarding the ability of PET/CT to predict lymph node response following chemoradiation.10–14 This has important treatment implications since patients with known lymph node metastases often undergo planned neck dissection 6 to 8 weeks after completion of nonsurgical organ preservation therapy. One can argue that patients can avoid a planned neck dissection if an imaging study can accurately identify successfully treated lymph nodes that have no pathologic evidence of tumor. However, there have been no prospective studies to properly evaluate this important management issue. Retrospective CT studies show that posttreatment contrast-enhanced computed tomography (CECT) alone can help eliminate planned neck dissection in a limited number of patients based on a very specific and simple morphologic analysis of nodes remaining visible in the neck on that examination.15–17 Based on those studies, the CECT is very accurate and can be applied in the usual window for such decision making about 4 to 6 weeks following the completion of RT or combined chemoradiation treatment.
The diagnostic accuracy of FDG-PET for identifying successfully treated lymph nodes appears to be highly dependent on the time interval between the PET/CT study and the completion of treatment. One group18 reported a 100% positive predictive value (PPV) but only a 14% NPV when FDG-PET was performed 1 month after the completion of treatment. Other groups19,20 reported a lower PPV (77%) but a higher NPV (100% and 97%, respectively) when FDG-PET was performed 3 to 4 months after completion of treatment. Further studies are needed to establish the utility of FDG-PET in the recently treated neck for deciding if planned neck dissection can be avoided in an FDG-PET negative neck. Such a utility seems unlikely based on current knowledge unless one is willing to wait 12 weeks post treatment to decide. Currently, such a delay is not considered the best course of action because of the progressive scarring that complicates surgery when such delays go beyond 4 to 8 weeks post RT.
Advanced Disease: Risk of Metastases and Secondary Primary Tumors
FDG-PET can be used in selected patients to search for pulmonary metastases. Reasonable indications would include advanced primary site disease, advanced neck disease such as many positive nodes and/or low neck nodes, biologic aggressiveness, and pathologic evidence of vascular space invasion. As more is understood about tumor biology and as PET agents for tumor imaging improve, indications may expand.
Solitary or multiple pulmonary nodules are often detected on anatomic imaging studies such as chest x-ray and chest CT in patients with mucosal SCCA (Fig. 5.7). FDG-PET is extremely useful to assess the risk of malignancy in pulmonary nodules. Delays to start of therapy to work up such problems in the past were common. Physicians feared that unnecessary morbid treatment for the primary and regional disease would be done in patients who might have distant disease or a second lung primary. FDG-PET helps confirm malignancy when positive. When negative, FDG-PET increases confidence in proceeding with treatment of the head and neck cancer and a policy of watchful waiting with regard to the pulmonary findings. PET/CT does not always obviate the need for tissue confirmation.
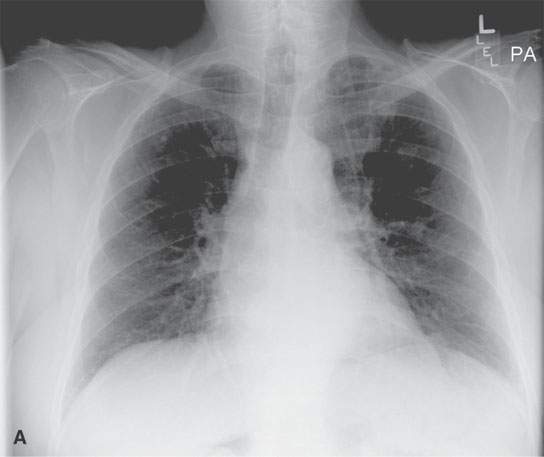
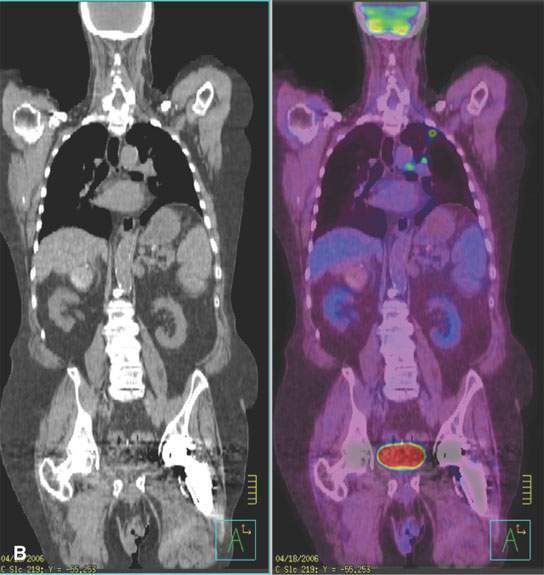
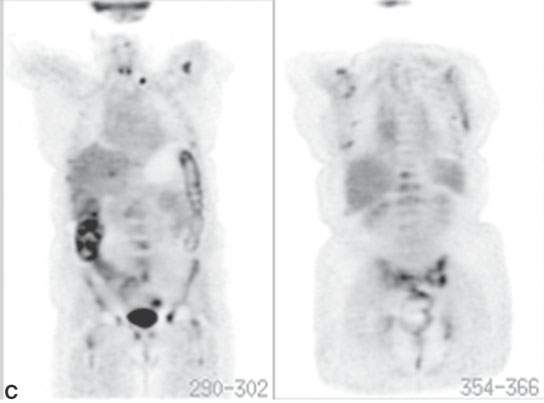
FIGURE 5.7. A patient with head and neck cancer and a suspicious chest x-ray as part of the initial evaluation. A: There is a subtle nodule beneath the left first rib and left clavicle. B: Fluorine-18 2-fluoro-2-deoxy-D-glucose positron emission tomography/computed tomography (FDG-PET/CT) shows this nodule to be malignant, with metastatic involvement of both left hilar and anteroposterior window nodes. C: A different patient with widespread metastases from squamous cell head and neck cancer. The patient was originally being planned for locoregional control but had fairly extensive disease at the primary site and in the neck and a poorly differentiated tumor. Selected coronal tomography from an FDG-PET scan shows a left supraclavicular metastasis, widespread bony metastases (multiple ribs, lumbar vertebrae, throughout the pelvis, proximal femurs, and both shoulders), and a liver metastasis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








