Presentation and Presenting Images
( ▶ Fig. 54.1, ▶ Fig. 54.2, ▶ Fig. 54.3, ▶ Fig. 54.4)
A 47-year-old female with a history of an excisional biopsy of a benign left axillary lymph node presents for routine screening mammography.
54.2 Key Images
( ▶ Fig. 54.5, ▶ Fig. 54.6, ▶ Fig. 54.7, ▶ Fig. 54.8)
54.2.1 Breast Tissue Density
The breasts are heterogeneously dense, which may obscure small masses.
54.2.2 Imaging Findings
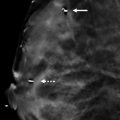
The imaging of the right breast is normal (not shown). The left breast demonstrates an obscured mass (circle in ▶ Fig. 54.5 and ▶ Fig. 54.6) measuring 7 mm at the 3 o’clock location in the middle depth, 7 cm from the nipple. The left breast tomosynthesis images ( ▶ Fig. 54.7 and ▶ Fig. 54.8) confirm the findings seen on mammography and that the mass is of low density. Sonography is required to definitively characterize masses. Benign and malignant lesions may present as well-circumscribed masses on tomosynthesis.
54.3 BI-RADS Classification and Action
Category 0: Mammography: Incomplete. Need additional imaging evaluation and/or prior mammograms for comparison.
54.4 Diagnostic Images
( ▶ Fig. 54.9)
54.4.1 Imaging Findings
Sonography shows an anechoic well-circumscribed mass with posterior acoustic enhancement at the 3 o’clock location that corresponds directly with the mass seen on the mammogram ( ▶ Fig. 54.9). Note on the ultrasound that the cyst is located within dense fibroglandular tissue, which can limit the visualization on conventional mammography.
54.5 BI-RADS Classification and Action
Category 2: Benign
54.6 Differential Diagnosis
Cyst: Cystic and solid masses may have the same appearance on mammography. Sonography can reliably differentiate between cystic and solid masses. This mass is a circumscribed anechoic mass with posterior acoustic enhancement and is consistent with a simple cyst.
Cancer: High-grade carcinomas and medullary carcinomas can mimic complicated cysts. These carcinomas may be markedly hypoechoic (a nearly anechoic appearance) and rounded.
Fibroadenoma: Fibroadenomas are oval or gently lobulated masses with parallel orientation and circumscribed margins. The internal echogenicity may range from isoechoic to hypoechoic.
54.7 Essential Facts
Tomosynthesis can confirm findings seen on conventional mammography and better define the mass and its margins. Tomosynthesis shows that the mass is lower density and well circumscribed.
The layers of breast tissue are shown separately on tomosynthesis and indeterminate or suspicious lesions seen on conventional mammography may be shown to have a benign appearance on tomosynthesis.
Radiologists should be careful not to dismiss all benign-appearing tomosynthesis-detected masses as benign.
If no correlate is seen on sonography, tomosynthesis-directed stereotactic biopsy may be performed.
54.8 Management and Digital Breast Tomosynthesis Principles
Rafferty and colleagues (2013) found that care must be taken to avoid misclassification of malignancies. It was evident in this study that circumscribed lobular cancers were dismissed as benign.
Additional studies evaluating circumscribed cancers need to be performed to identify commonalities among these lesions.
In a letter to the radiology editor (2013), Dr. Kopans described cancers that will be missed with both conventional mammography and tomosynthesis. These cancers arise in fibroglandular tissue, do not have a margin highlighted in fat, do not distort the architecture, and do not produce calcifications.
Although there are some malignancies that are occult and undetected on all imaging studies, additional studies to evaluate tomosynthesis and missed cancers need to be performed to reduce the numbers of missed and misclassified malignancies.
54.9 Further Reading
[1] Kopans DB. Digital breast tomosynthesis: a better mammogram. Radiology. 2013; 267(3): 968‐969 PubMed
[2] Rafferty EA, Park JM, Philpotts LE, et al. Assessing radiologist performance using combined digital mammography and breast tomosynthesis compared with digital mammography alone: results of a multicenter, multireader trial. Radiology. 2013; 266(1): 104‐113 PubMed

Fig. 54.1 Left craniocaudal (LCC) mammogram.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree