Presentation and Presenting Images
A 52-year-old female with a personal history of right breast cancer treated with lumpectomy and radiation therapy 4 years prior presents for screening mammography.
40.2 Key Images
40.2.1 Breast Tissue Density
There are scattered areas of fibroglandular density.
40.2.2 Imaging Findings
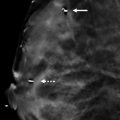
In the upper inner quadrant at the 10 o’clock location in the middle depth of the left breast, there is a small obscured mass. The complexity of the breast tissue pattern makes it difficult to localize this mass from the background on the conventional digital mammograms ( ▶ Fig. 40.1 and ▶ Fig. 40.2). The tomosynthesis images, help to identify and localize this small mass ( ▶ Fig. 40.3 and ▶ Fig. 40.4).
40.3 BI-RADS Classification and Action
Category 0: Mammography: Incomplete. Need additional imaging evaluation and/or prior mammograms for comparison.
40.4 Diagnostic Images
( ▶ Fig. 40.5, ▶ Fig. 40.6, ▶ Fig. 40.7, ▶ Fig. 40.8, ▶ Fig. 40.9, ▶ Fig. 40.10, ▶ Fig. 40.11, ▶ Fig. 40.12)
40.4.1 Imaging Findings
The diagnostic imaging demonstrates a persistent 6-mm irregular mass with spiculated margins. It is best seen on the craniocaudal (CC) view ( ▶ Fig. 40.5), and remains mostly obscured on the mediolateral oblique (MLO) spot-compression view ( ▶ Fig. 40.6 and ▶ Fig. 40.8). A targeted ultrasound ( ▶ Fig. 40.9) reveals a corresponding 6-mm irregular hypoechoic mass with angular margins and mild posterior shadowing located at 10 o’clock, 5 cm from the nipple. An ultrasound-guided biopsy was performed and the postprocedure mammograms reveal the coil biopsy marker clip in the area of the mammographic mass ( ▶ Fig. 40.10 and ▶ Fig. 40.11). This mass was eventually localized by a wire for surgical excision. The specimen radiograph demonstrates a small spiculated mass with the localization wire and coil marker clip adjacent to it ( ▶ Fig. 40.12).
40.5 BI-RADS Classification and Action
Category 4C: High suspicion for malignancy
40.6 Differential Diagnosis
Breast cancer (invasive ductal carcinoma): The margins of the mass as seen on DBT and ultrasound suggest a suspicious finding. Cancer is highly suspected.
Sclerosing adenosis (SA): Sclerosing adenosis is known to mimic cancer. When assessing biopsy concordance, the size of the lesion seen on imaging should be reflective of the lesion size on pathology. A microscopic focus of SA in the background of other breast tissue would not be concordant, and excision should be recommended.
Focal fibrosis (FF): Similar to SA, FF can also mimic cancer, as an architectural distortion or an irregular mass. Similar to SA, a pathologic diagnosis based on an image-guided biopsy should reflect the size of the lesion on imaging to be considered concordant.
40.7 Essential Facts
DBT is very helpful in localizing a lesion seen in one projection to the orthogonal image. In this case, the lesion is well seen on the FFDM CC view, where there little if any overlap of tissues in the medial aspect of the breast. However, on the FFDM MLO view, there are many similar-appearing densities in the breast at the depth of the lesion seen on the FFDM CC view.
A lesion seen in only one DBT projection still affords the potential for localization. The side-to-side (MLO projection) or head-to-foot (CC projection) location within the DBT stack will aid in directing diagnostic mammography and/or an ultrasound examination.
A developing asymmetry is a focal asymmetry that is new or increasing in size compared to prior imaging studies.
DBT may increase the perception of developing asymmetries due to its unmasking ability.
40.8 Management and DBT Principles
Developing asymmetries are often subtle mammographic findings.
Developing asymmetries can often present as only a one-view finding. Traditional triangulation techniques are helpful to localize a lesion. DBT may provide added benefit in triangulating a lesion in two orthogonal planes to optimize characterization, ultrasound evaluation, and biopsy.
Lesions that are only seen on one view are difficult to evaluate. A nontargeted ultrasound exam may find one or several lesions. The risk is that one or none of these might be the lesion seen mammographically.
40.9 Further Reading
[1] Price ER, Joe BN, Sickles EA. The developing asymmetry: revisiting a perceptual and diagnostic challenge. Radiology. 2015; 274(3): 642‐651 PubMed
[2] Roth RG, Maidment AD, Weinstein SP, Roth SO, Conant EF. Digital breast tomosynthesis: lessons learned from early clinical implementation. Radiographics. 2014; 34(4): E89‐E102 PubMed

Fig. 40.1 Left craniocaudal (LCC) mammogram.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree